Glomerular Apparatus and Filtration - Anatomy & Physiology
Glomerular Filtration
The role of the renal corpuscle is to selectively filter the blood by allowing small molecules through but preventing plasma proteins from leaving the blood. This filtration occurs extracellulary and is done by what is know as the glomerular filtration barrier. This structure is made up of three layers:
- Fenestrated capillary endothelium
- Glomerular basement membrane
- Podocytes
Fenestrated Capillary Endothelium
- There are small gaps called fenestrae in the cytoplasm of the capillary endothelium.
- They account for approximately 10% of the surface area of the cells
- They allow water and non-cellular components of the blood to pass through
- They act mainly as a barrier to the cells of the blood
Glomerular Basement Membrane
- Also known as the basal lamina
- This is the main barrier to proteins
- Restricts all but the smallest plasma proteins from passing through
- Made up of a protein mesh in a gelatinous matrix
- Composed of collagen and other matrix proteins
- Prevents filtration of compounds >7,000 Da
- Lower permeability to anions compared to cations. This allows for further selective filtration
Podocytes
The cells of the visceral layer of the Bowmans capsule possess finger like foot processes called pedicels. These wrap around the outer layer of the basal lamina. Filtration occurs through small gaps between pedicels called slit diaphragms. This is the final barrier against proteins
Factors Which Determine Selective Filtration
- Hydrostatic pressure in the capillaries causes filtration but as the filtrate is basically protein free there is no real protein osmotic pressure in the Bowmans capsule. This means the filtration is almost entirely powered by the hydrostatic pressure in the capillaries.
- Molecular size - molecules with a radius of 4nm or more aren't filtered, whilst those with a radius less than 2nm are filtered without restriction. Thus the filtration barrier is selectively permeable.
- Electrical charge
- The barrier has a net negative charge thanks to cells in the membrane having a negatively charged surface and a basal lamina with negatively charged glycoproteins.
- Therefore negatively charged molecules are filtered less than positive or neutral ones
- Proteins are negatively charged. This and their size prevents their filtration
- Protein binding
- Drugs, ions or small molecules which are bound to protein are not filtered
- Molecular configuration
- Round molecules fit less easily than ellipsoid ones
- Rigidity
- The higher the rigidity of a molecule the less easily it is filtered
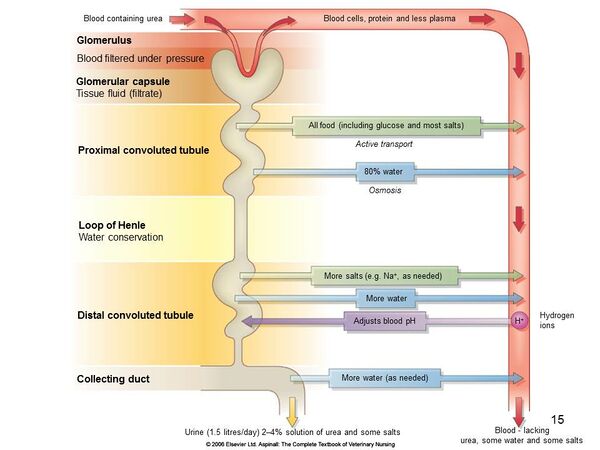
Composition of Filtrate
- Normal filtrate is basically protein free.
- However small amounts of albumin do make it across the membrane. These are completely reabsorbed in the proximal tubules
- Small molecules with a molecular weight <7,000 Da are filtered without restriction these include:
- Water
- Sodium, chloride, creatinine, urea, uric acid and phosphate are filtered in isotonic levels (same concentration as plasma)
- Larger molecules with a molecular weight >7,000 Da such as myoglobin (17,000 Da) are filtered less
- Movement of larger molecules is restricted
- Plasma proteins with molecular weights up to 70,000 Da are heavily restricted from passing through the glomerulus
- Charged molecules over 70,000 Da are not filtered at all
- The threshold for neutral molecules is 100,000 Da
| Glucose | 180 | 1 |
| Myoglobin | 17,000 | 0.75 |
| Haemoglobin | 68,000 | 0.03 |
| Albumin | 69,000 | <0.01 |
Glomerular Filtration Rate
Pressure in the Peritubular Capillaries
The peritubular capillaries have a lower hydrostatic pressure and a higher protein osmotic pressure than the rest of the capillaries in the body. This is largely thanks to the fact that the blood within them has had a substantial quantity of its plasma removed by the glomerulus, resulting in a low concentration of solutes but a high concentration of protein. These pressures however are not constant and changes in them affect reabsorption. They have the biggest effect in the proximal tubule thanks to the relatively weaker tight junctions which allow water and ions to pass paracellulary.
The Effects of Changing Pressure
If hydrostatic pressure is elevated and protein osmotic pressure reduced, then water leaves the interstitium and enters the tubular lumen thus increasing water loss. These pressure changes are characteristic of a situation where the animal drinks a large amount of water in a short period of time.
If the situation is reversed it results in a decreased urinary output and is often caused by a fall in blood pressure associated with a reduction in ECF.
Renal Clearance
Renal clearance is the ability of the kidney to remove a compound from the blood. It is intimately linked to the glomerular filtration rate, tubular reabsorption and secretion. Renal clearance is just part of the total body clearance of a compound. Other methods of clearance include; biliary, pulmonary and salivary excretion. To look at the renal clearance you need to know the amount of plasma that must have been filtered to produce that much of the substance in the urine per given unit of time. This is given by the following formula:
Clearance = (Urine Concentration of a Substance x Urine Volume per unit time) / Plasma Concentration of the Substance
Renal Clearance and GFR
For the clearance to represent the GFR the substance looked at must be filtered freely and from that point on as it travels through the nephron its concentration must not be altered. Therefore it must not be secreted or reabsorbed.
Determination of GFR from Renal Clearance
Inulin, Creatinine or Urea can be used.
Inulin
Inulin is injected into the plasma. It is freely filtered by the glomerulus and therefore its rate of excretion is directly proportional to the rate of filtration of water and solutes.
Creatinine
Creatinine is also freely filtered by the glomerulus so it represents a close approximation to GFR. You can measure endogenous creatinine. It's production from muscle is constant. In renal failure its secretion is reduced and it is secreted into the gut. You can also measure it by infusing exogenous creatinine. It is difficult as urine collection needs to be carried out over time and blood samples need to be taken.
Urea
The idea behind this is that you measure factors which would normally be excreted. The same idea is behind the measurement of endogenous creatinine. However this is not ideal as it is altered by non-renal factors and they only change when the renal failure is very advanced as there is a large functional reserve in the kidneys. Urea is also not ideal in horses and ruminants as it is used by the digestive micro flora to make microbial protein.
Revision
Use the flash card revision resource for this section to test yourself.