Necrosis - Pathology
Jump to navigation
Jump to search
Introduction
- Necrosis means the death of cells within the living body.
- Two things happen when necrosis occurs:
- Further changes can take place in the tissue itself.
- The surrounding unaffected living tissue can react against this necrotic tissue.
Causes of Necrosis
- There are three main causes of necrosis:
Loss of Blood Supply
- Necrosis due to interuption of blood supply to a portion of tissue is known as ischaemic necrosis, or infarction.
- The effects of ischaemia on a tissue vary according to:
- The tissue affected.
- Some tissues are more susceptible than others.
- The type of cell in the tissue.
- Generally, parenchymatous (functioning) cells are more susceptible than the stromal supporting cells.
- The metabolic activity of the tissue.
- Very active organs are more susceptible.
- Whether there is a good or potential collateral blood supply.
- The tissue affected.
- Tissue ischamia can be brought about in three ways:
- Compression of the blood vessel.
- Narrowing of the lumen.
- Blocking of the lumen .
Compression of the Blood Vessel
- A common cause of tissue ischaemia is strangulation of the intestine by a twist upon itself.
- Compression of the mesenteric veins prevents outflow of blood
- The affected portion becomes congested and swollen.
- The arterial supply cannot supply sufficient blood because of pressure in the swollen intestine and its vessels.
- The affected area undergoes an ischaemic necrosis.
- Sequelae include
- Rupture and peritonitis
- Gangrene and toxaemia
- Due to absorption of toxic products of the necrosis and intestinal bacteria.
- Sequelae include
- The affected area undergoes an ischaemic necrosis.
- Compression of the mesenteric veins prevents outflow of blood
- Another cause is a mass, such a lipoma, forming in the mesentery
- Becomes pedunculated (attached by a fine band of the mesentery).
- Can encompass and strangulate a portion of intestine.
- Becomes pedunculated (attached by a fine band of the mesentery).
Narrowing of the Lumen
- E.g. thickening of the wall in arteriosclerosis.
Blocking of the Lumen
Physical or Chemical Agents
Physical Agents
- Include:
- Burns
- Cold
- Frostbite
- X-rays
- Pressure
- Pinching or crushing of the tissue.
- Necrosis my be:
- Direct
- E.g. in the case of burns.
- Indirect
- E.g. in crushing or pinching.
- Vessels supplying the tissue are occluded, leading to necrosis of the tissue.
- Direct
Chemical Agents
- May be directly caustic or corrosive in action.
- May exert their effects when absorbed and metabolised to a more toxic substance.
Living agents
- Living agents exert their effects though either
- Their toxic effects on cells, or
- Their colonisation of the cells.
Appearance of Necrotic Lesions
- There are three zones in a typical necrotic lesion.
- There is a sphere of necrosis where the effect of the causal agent is maximal.
- A little further away there is a zone where the tissue is damaged, but not yet dead.
- Still farther away, the effect of the agent is insufficient to cause death or degeneration of cells.
- There is a zone where the body is reacting to the dead tissue.
Gross and Histological Features of Necrotic Tissue
- A change in colour is seen in necrotic tissue,
- Dead tissue tends to be paler than live tissue.
- This is partly because there is no circulation.
- Dead tissue tends to be paler than live tissue.
- There is also a change in the consistency of the tissue.
- The appearance of the centre of the necrotic lesion varies according to:
- The type of agent responsible
- The tissue in which the agent is acting.
- This appearance may give a clue to the agent responsible.
Types of Necrosis
- The types of necrosis encountered are based on their gross description.
Coagulation Necrosis
- Coagulation necrosis is a feature of:
- Bacteria which produce toxins
- Infarction
- Some foci of viral replication.
Gross
- The necrotic lesion is firmer and dryer on the cut surface. The
- There is some resemblance to the nearby living tissue.
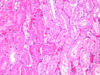
Histological
- The general architecture of the tissue is preserved.
- Certain changes related to loss of cellular detail can be recognised in an ordinary H&E section.
- Cells may appear larger and their outline may be lost
- Cytoplasm appears structureless and homogenous.
- There are nuclear changes
- This is the most important feature.
- There are three types of nuclear change.
- Pyknosis
- Greek for dense.
- The normal nuclear structure is replaced by a very dense, heavily staining, smaller, angular mass of chromatin.
- Karyorrhexis
- This is from the Greek:
- karyon = nucleus
- rhexis = breaking up
- The nucleus appears as though it has exploded rather than condensed.
- Irregular-sized bits of dense nuclear material are found scattered throughout the centre of the cytoplasm.
- A kind of "reverse appearance" to pyknosis.
- This is from the Greek:
- Karyolysis
- Karyolysis means dissolution of the nucleus.
- The nucleus is more faintly stained with haematoxylin.
- Only the ghost outline of the nucleus remains.
- Pyknosis
Liquefactive Necrosis
Malacia
- This is liquefactive necrosis in the brain.
- There is a lot of lipid in the brain.
- The intracellular enzymatic changes involved in necrosis make this softer and more fluid.
- Initially the affected area becomes swollen and gelatinous.
- Is sometimes bloodtinged due to disruption of the blood vessels.
- Later the area becomes fluid.
- The microscopic appearance does not resemble the nearby living tissue.
- The tissue is becoming a fluid.
Pus Formation
- Occurs when the organism causing the initial necrosis in the tissue is capable of attracting and killing large numbers of neutrophils]].
- I.e the pyogenic bacteria.
- Neutrophils release proteolytic enzymes when they die.
- These digest the dead tissue and also more incoming neutrophils.
- The liquid formed is called pus.
- These digest the dead tissue and also more incoming neutrophils.
- Pus is mainly composed of dead and dying neutrophils .
- Also contains the remnants of the necrotic tissue cells.
- Although in favourable cases the neutrophils may eventually kill the organisms, in most cases the organisms persist, producing more pus.
- Produces an expanding sphere of pus known as an abscess.
- If the abscess is near to the skin and pressure becomes sufficient after build up, it will burst.
- Pus is discharged, hopefully along with the organisms responsible.
- This is nature's way of ridding the body of an injurious agent.
- If the abscess is near to the skin and pressure becomes sufficient after build up, it will burst.
- Produces an expanding sphere of pus known as an abscess.
Histological Appearance of an Abscess
- The necrotic area shows varying stages of degeneration of the neutrophils.
- Ranges from nearly normal neutrophils, through pyknosis, karyorrhexis and karyolysis, finally to a homogenous, structureless, mixture of remnants.
- Stains faintly bluish.
- Ranges from nearly normal neutrophils, through pyknosis, karyorrhexis and karyolysis, finally to a homogenous, structureless, mixture of remnants.
- There is a host inflammatory response directed against the sphere of pus as it is forming.
- Results in a capsule of fibrous tissue which has many blood vessels on its inner surface.
- Allows the transport of the vast number of neutrophils into the necrotic centre.
- Known as the 'pyogenic membrane'.
- Can be viewed following abscess discharge as a crater that has a reddish, somewhat ragged lining.
- The fibrous capsule around the pus is markedly thickened when the abscess is deep within an organ, such as the liver, and there is nowhere to discharge to.
- Results in a capsule of fibrous tissue which has many blood vessels on its inner surface.
Caseation Necrosis
- Caseation necrosis is a feature of granulomatous processes.
- E.g. tuberculosis in the ox, pig and sheep.
- Necrotic tissue is not derived from the organ in which it occurs.
- Formed from Macrophages sent into the tissue in large numbers to engulf the causative organism.
- The organism has defences against the enzymes of the Macrophages.
- Is able to grow and multiply within these macrophages and eventually causes their death.
- In some granulomas, the macrophages will combine together and form giant cells.
- Fungi and parasites also cause granulomas.
Gross
- The necrotic tissue appears grossly like cheese.
- Colour varies from white-grey to yellowish.
- Appears whitish in sheep.
- There may be a yellowish tinge in cattle.
- Fluid content also varies.
- Some cases have a dry, crumbling consistency
- Others are more like cottage cheese.
- Colour varies from white-grey to yellowish.
- Caseation necrosis is really a mixture of coagulation and liquefactive necrosis.
- Is a feature of necrosis caused by some specific organisms.
Histologically
- There is complete loss of the tissue architecture.
- The necrotic material is purplish in colour
- Due to random intermixing of components that stain with haematoxylin and eosin.
- I.e. bits of nuclear material interspersed with cytoplasmic fragments.
- Due to random intermixing of components that stain with haematoxylin and eosin.
Sequelae to Necrosis
- Sequelae vary in relation to the causes of necrosis.
Response to Local Injury
- While a piece of dead tissue on the surface of the body (e.g. skin) can be shed, dead tissue in the depths of the body (e.g. liver) cannot.
In the Depths of the Body
- Dead tissue in the center of the body can be
- Absorbed and replaced by fibrous tissue.
- Enclosed by fibrous tissue.
- As a general rule:
- Small areas of necrosis become absorbed and replaced by fibrous tissue.
- Scars.
- Larger areas of necrosis become encapsulated by fibrous tissue.
- Encapsulated portion is called a "sequestrum".
- Cuts off any contact with living tissue
- Allows further changes to occur to make the necrotic material more inert.
- E.g. by calcification
- Small areas of necrosis become absorbed and replaced by fibrous tissue.
On an Epithelial Surface
- There are two possible outcomes to necrosis occuring on an epithelial surface.
- Depends upon the depth of the necrosis.
- When the necrosis is confined to the middle and outer layers of the epithelium (an erosion), the underlying germinal layer divides and replaces the shed portion.
- Leaves no scar.
- E.g. in Foot and Mouth Disease
- When the necrosis extends below the basement membrane of the epithelium and the integrity of the epithelium is compromised (an ulceration), there is an inflammatory reaction.
- An attempt is made to repair the deficit by fibrous tissue.
- Contraction of the fibrous tissue leaves a scar.
- Caused e.g. by an applied corrosive substance or a burn.
- An attempt is made to repair the deficit by fibrous tissue.
Fat Necrosis
- Fat necrosis is confined to the fat depots of the body.
- Has a very distinctive gross appearance.
- The fat shows areas of focal opacity and is very hard.
- Is normally semi-translucent and malleable.
- The fat shows areas of focal opacity and is very hard.
- After the fat cells have died, the intracellular fat is broken down into fatty acids.
- These fatty acids combine with Ca++, Na+ and K+ ions to forms soaps.
- The soaps formed are foreign to the body and provoke an inflammatory response.
- These areas of fat necrosis remain indefinitely.
- May show great scarring.
- Quite often calcify.
- These areas of fat necrosis remain indefinitely.
- Soaps do not dissolve out in routine preparation of sections.
- There are two principal methods of fat necrosis in the body:
- Enzymatic necrosis of fat.
- Traumatic necrosis of fat.
Enzymatic Necrosis of Fat
- Occurs when there is a release of pancreatic enzymes into the neighbouring mesenteric fat.
- Release is caused by a damaged pancreas.
- E.g. due to an adjacent tumour.
- Release is caused by a damaged pancreas.
Traumatic Necrosis of Fat
- Seen in the subcutaneous tissue following trauma to the area.
- Quite common in the brisket of recumbent animals due to the prolonged pressure on the area.
Lipomatosis
- Lipomatosis is another condition of fat that can involve necrosisis and calcification.
- Occurs for some unknown reason in Channel Island breeds of cattle.
- There are focal areas of increased fat in the mesentery.
- Often surround several loops of the gut.
- If they become necrotic, they may strangle the enclosed gut with disastrous consequences for the animal.
- Often surround several loops of the gut.
Gangrene
- Gangrene is a post-necrotic change.
- In some cases is gangrene is the ultimate degradation of necrotic tissue.
- The tissue is already dead.
- There are two main types of gangrene.
- Wet gangrene
- Life-threatening
- Dry gangrene
- Non life-threatening
- Wet gangrene
Wet gangrene
- Wet gangrene can either be due to:
- The agent which initially kills the tissue.
- Gangrene is just further putrifaction.
- Primary gangrene.
- E.g. gangrenous mastitis of the udder of the cow caused by Staphylococcus aureus.
- Invasion of dead tissue by organisms which putrefy it.
- Secondary gangrene.
- E.g. following ischaemic necrosis of the gut, the putrefactive organisms that are normally present in the gut invade the dead tissue.
- Secondary gangrene.
- The agent which initially kills the tissue.
- A further cause of wet gangrene is when a ligature around an extremity causes ischaemic
necrosis of tissue distal to it and the necrotic tissue becomes invaded with putrefactive bacteria.
- Wet gangrene is overwhelming disastrous for the animal unless treated quickly and effectively.
- The animal rapidly succumbs to toxaemia.
- The organisms produce potent toxins, either themselves, or in their breakdown of the dead tissue.
- The animal rapidly succumbs to toxaemia.
Gross Appearance
- Tissue
- Is swollen and puffy
- Is cold to the touch
- Smells horrible
- Due to the hydrogen sulphide produced in the putrefying tissue.
- The zone of inflammation between the dead putrefying tissue and living tissue is indistinct.
Gas Gangrene
Dry Gangrene
- Not life threatening.
- Is really mummification of an extremity.
- E.g. the tail, foot or ears of animals.
- There is occlusion of the blood supply to the extremity.
- The tissue becomes necrotic.
- Water is drawn out of the tissue due to air circulating around the extremity.
- Dries and preserves the extremity.
- Eventually sloughs off.
- Dries and preserves the extremity.
- Little if any bacterial growth in the tissue.
- E.g.:
- In small animals
- Crushing of the tail.
- In large animals.
- Commonly seen following a septicaemic condition when an embolus blocks the blood supply.
- When seen in calves, the possibility of salmonellosis must be kept in mind.
- Other causes are frostbite and ergot poisoning.
- Commonly seen following a septicaemic condition when an embolus blocks the blood supply.
- In small animals
Calcification
- In calcification, calcium salts are deposited within the necrotic tissue to make it more inert.
- Does NOT result from elevated blood calcium levels.
- Seen quite commonly in necrosis in cattle and sheep.
- Is a common feature in lesions which show caseation necrosis.
- Usually indicates a lesion of long standing.
Gross Appearance
- The deposits of calcium salts can be palpated.
- On cutting into the necrotic area, the calcified material may be:
- Felt as a gritty substance.
- Heard as a grating sound against the knife.
- The colour is usually chalk-white.
- There may be a yellowish-green tinge if the inciting cause is a parasite.
- Due to attraction of a large number of eosinophils.
- There may be a yellowish-green tinge if the inciting cause is a parasite.
Histological Appearance
- Calcium has a distinctive dark blue colour when stained with H&E.
- Some bacterial colonies stain a similar colour.
- May be difficult to distiunguish calcium form these.
- Some bacterial colonies stain a similar colour.
- Sections may show shattering of the calcium and adjacent tissue due to the effect of the microtome knife.
- Blunts the knife - there may be score marks throughout the rest of the section.
- Sections may be stained with silver nitrate to check for calcium by the von Kossa method.
- The calcium stains black.
Apoptosis
- Apoptosis is another method of cell death.
- Programmed death of scattered single cells in living tissues.
- Unlike necrosis, there is no reaction to the death of the cell.
- It is thought that some cells are programmed to die unless there is a change in circumstances that require them to continue living. This is a form of cell regulation.
- One such circumstance is the development of tumours.
- Cellular regulation is absent.
- One such circumstance is the development of tumours.
- Cellular apoptosis is important in many processes:
- The deletion of extra cells produced in embryogenesis.
- Cyclical physiological changes in the genital tract of females.
- The death of lymphocytes
- Graft rejection
- Cellular death by the same injurious substances that cause necrosis in higher doses.
- The process of apoptosis:
- Cells lose their connections with their neighbours and shrink.
- The nucleus becomes pyknotic.
- The cytoplasm becomes eosinophilic.
- The cell breaks up into fragments that are engulfed by neighbouring cells or local macrophages.
- Their remnants can be seen in the neighbouring cells’ cytoplasm.