Difference between revisions of "Bones - Anatomy & Physiology"
(→Cells) |
m (→Types of Bone) |
||
| (24 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
| − | + | {{OpenPagesTop}} | |
==Overview== | ==Overview== | ||
| − | |||
| − | |||
[[Image:Horse Skeleton.jpg|thumb|right|250px|Horse Skeleton - Copyright Nottingham]] | [[Image:Horse Skeleton.jpg|thumb|right|250px|Horse Skeleton - Copyright Nottingham]] | ||
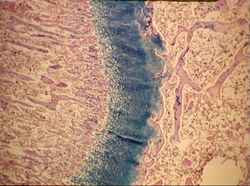
| + | [[Image:Growth plate.jpg|right|thumb|250px|<small><center>Growth plate (Image sourced from Bristol Biomed Image Archive with permission)</center></small>]] | ||
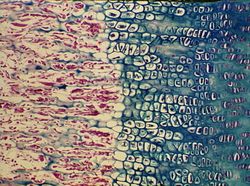
| + | [[Image:Growth plate closer.jpg|right|thumb|250px|<small><center>Growth plate magnified (Image sourced from Bristol Biomed Image Archive with permission)</center></small>]] | ||
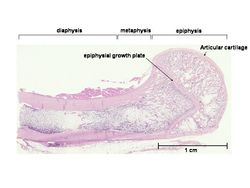
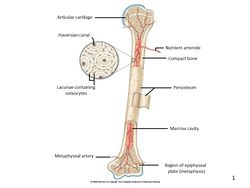
| + | [[Image:Aspinall Slide1.JPG|thumb|right|250px|<small>Image from [http://www.elsevierhealth.co.uk/veterinary-nursing/spe-60136/ Aspinall, The Complete Textbook of Veterinary Nursing], Elsevier Health Sciences, ''All rights reserved''</small>]] | ||
| + | Bone comprises the structure of the skeletal system and provides lever arms for locomotion. Bone also plays important roles in maintaining mineral homeostasis, as well as providing the environment for [[Haematopoiesis - Overview|hematopoesis]] in [[Bone Marrow|marrow]]. | ||
| − | + | '''Short bones''' - Endochondral ossification continues in the diaphysis, until only the cartilage rim remains. | |
| − | |||
| − | ''' | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | '''Long bones''' - A secondary center of ossification develops in the epiphyses. | |
| − | + | See [[Bone & Cartilage Development - Anatomy & Physiology|Bone and Cartilage Development]] | |
| − | |||
| − | |||
| − | |||
| − | + | ==Bone Growth== | |
| − | + | ===Length=== | |
| + | The '''epiphyseal growth plate (EGP, physis)''' is a transverse disc of cartilage between the two ossification centers and allows the bone to continue to grow in length after birth. It then closes. The EGP is a region of continuous chondroblast differentiation and maturation and can be divided into five zones: | ||
| − | + | # '''Germinal Zone''' - chondroblast division at a low rate, and self renewal. | |
| + | # '''Proliferation Zone''' - chondroblast division at a fast rate. | ||
| + | # '''Maturation Zone''' - chondroblast differentiation into chondrocytes. | ||
| + | # '''Hypertrophic Zone''' - chondrocytes enlarge and then die. | ||
| + | # '''Dead cells''' become the matrix for bone growth. | ||
| − | + | ===Girth=== | |
| − | ''' | + | The '''periosteum''' lines the outer surface of the diaphysis of the bone. It has a cellular inner layer, consisting of osteoblasts, and a fibrous outer layer. The '''endosteum''' lines the inner surface of the diaphysis of the bone. It contains osteoblasts ''and'' osteoclasts. Bone growth occurs by a shift in the equilibrium between osteoblasts and osteoclasts. Osteoblasts on the outside in the periosteum add bone to increase the bone's diameter. Osteoclasts on the inside in the endosteum remove this bone to maintain the bone diameter. When osteoclasts start removing less bone, or osteoblasts start adding more bone, the girth increases. |
| − | |||
| − | + | ==Bone Remodeling== | |
| + | [[Image:Haversian system.jpg|right|thumb|250px|<small><center>Haversian system (Courtesy of RVC Histology images)</center></small>]] | ||
| + | '''Primary''' bone has not yet been '''remodelled'''. It contains less mineral and more randomly arranged collagen fibers, known as trabecular organization. Remodelling of bone occurs by '''haversian canals'''. The osteoclasts dig out the canal longitudinally through the bone connecting with bone marrow cavity and periosteum. They are followed by anastamosing and branching blood vessels. Concentric bony lamellae are laid down with rows of interconnected lacunae containing '''osteocytes''' within. The osteocytes communicate by channels in young bones. Phased resorption happens concurrently. | ||
| − | + | '''Haversion canals + lamellae + osteocytes = Haversion system''' | |
| − | |||
| − | |||
| − | |||
| − | ''' | ||
==Types of Bone== | ==Types of Bone== | ||
| Line 58: | Line 50: | ||
Found in the skull, pelvic girdle, and scapula. It expands in two directions, with a broad surface for attachment of large muscle masses and protection of underlying structures. | Found in the skull, pelvic girdle, and scapula. It expands in two directions, with a broad surface for attachment of large muscle masses and protection of underlying structures. | ||
| − | 4. '''Sesamoid | + | 4. '''Irregular Bone''' |
| + | |||
| + | Found in the vertebrae. | ||
| + | |||
| + | 5. '''Sesamoid Bone''' | ||
Eg. Patella and navicular bone. Found within tendons, where they change direction over prominences that would otherwise cause damage. They form '''synovial joints''' with major bones with which they are in contact. They also serve to displace tendon from the axis of the joint, increasing the leverage exerted by the muscle. | Eg. Patella and navicular bone. Found within tendons, where they change direction over prominences that would otherwise cause damage. They form '''synovial joints''' with major bones with which they are in contact. They also serve to displace tendon from the axis of the joint, increasing the leverage exerted by the muscle. | ||
| − | + | 6. '''Splanchnic Bone''' | |
Develop in soft organs remote from skeletal connection, eg. '''os penis'''. | Develop in soft organs remote from skeletal connection, eg. '''os penis'''. | ||
| − | + | 7. '''Pneumatic Bone''' | |
Excavated to contain air spaces, such as the skull in the instance of paranasal sinuses, and the post-cranial skeleton of birds. | Excavated to contain air spaces, such as the skull in the instance of paranasal sinuses, and the post-cranial skeleton of birds. | ||
==Composition of Bone== | ==Composition of Bone== | ||
| − | |||
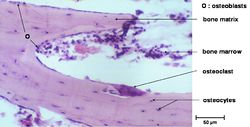
[[Image:Bone histo.jpg|right|thumb|250px|<small><center>Histological structure of bone (Courtesy of RVC Histology images)</center></small>]] | [[Image:Bone histo.jpg|right|thumb|250px|<small><center>Histological structure of bone (Courtesy of RVC Histology images)</center></small>]] | ||
[[Image:Bone micro structure.jpg|right|thumb|250px|<small><center>Microscopic bone (Courtesy of RVC Histology images)</center></small>]] | [[Image:Bone micro structure.jpg|right|thumb|250px|<small><center>Microscopic bone (Courtesy of RVC Histology images)</center></small>]] | ||
| − | |||
Bone is a hard, highly specialised connective tissue . It consists of interconnected cells embedded in a calcified, collagenous matrix. It is a living, dynamic, responsive tissue, growing and remodelling throughout life. | Bone is a hard, highly specialised connective tissue . It consists of interconnected cells embedded in a calcified, collagenous matrix. It is a living, dynamic, responsive tissue, growing and remodelling throughout life. | ||
| − | Bone is | + | Bone is composed of: |
===Matrix=== | ===Matrix=== | ||
| − | '''Osteoid'''- An organic, uncalcified, homogeneous substance that stains light pink with H&E . Osteoid consists of type I collagen (90%), which resists tension and bone-specific proteins(10%), including; Osteonectin, Osteopontin and Osteocalcin. | + | '''Osteoid'''- An organic, uncalcified, homogeneous substance that stains light pink with H&E . Osteoid consists of type I collagen (90%), which resists tension, and bone-specific proteins (10%), including; Osteonectin, Osteopontin and Osteocalcin. |
| − | '''Mineral'''- An inorganic component | + | '''Mineral'''- An inorganic component that provides rigidity and consists of a crystalline lattice of calcium phosphate and calcium carbonate. It also contains Mg, Mn, Zn, Cu, Na, F. It accounts for 65% of bone. |
===Cells=== | ===Cells=== | ||
| Line 89: | Line 83: | ||
'''Osteoblasts''' | '''Osteoblasts''' | ||
| − | A single layer of mesenchymal cells which synthesize bone extracellular matrix (osteoid). When active, | + | A single layer of mesenchymal cells which synthesize bone extracellular matrix (osteoid). When active, they appear plump and cuboidal, with a basophilic cytoplasm. The cell membranes are rich in alkaline phosphatase (ALP). The cells are possibly involved in pumping calcium across membranes. They are promoted by growth factors and have receptors for [[Calcium#Parathyroid Hormone (PTH)|PTH]]. They contract in response, which provides space for osteoclasts to attach. When they are inactive, there is less cytoplasm, so they become flattened. |
'''Osteocytes''' | '''Osteocytes''' | ||
| − | + | Osteocytes are embedded in their own matrix; reside within '''lacunae''' and are interconnected via channels forming '''canaliculi'''. Canaliculi create connections to form a huge neural-like junctional organization. They contact osteoblasts and each other with cytoplasmic processes and reach through canaliculi in the mineralised bone matrix. Osteocytes regulate the composition of bone fluid. | |
'''Osteoclasts''' | '''Osteoclasts''' | ||
| − | Osteoclasts are giant (multinucleate [[Monocytes|monocytes]]) cells. Histologically, they are large, often multinucleated cells. They have an acidophilic cytoplasm. They sit in the bone surface depression known as, '''howship's lacuna'''. Osteoclasts respond to vitamin D by increasing their numbers and activity (parathyroid independent). Osteoclasts act to resorb the bone ECM. They firstly dissolve mineral followed by collagen, using the brush border. They do <u>not</u> have receptors for PTH, but do have receptors for [[Calcium#Calcitonin|calcitonin]]. | + | Osteoclasts are giant (multinucleate [[Monocytes|monocytes]]) cells. Histologically, they are large, often multinucleated cells. They have an acidophilic cytoplasm. They sit in the bone surface depression known as, '''howship's lacuna'''. Osteoclasts respond to [[Calcium#Calcitriol (Activated Vitamin D3)|vitamin D]] by increasing their numbers and activity (parathyroid independent). Osteoclasts act to resorb the bone extracellular matrix (ECM). They firstly dissolve mineral followed by collagen, using the brush border. They do <u>not</u> have receptors for PTH, but do have receptors for [[Calcium#Calcitonin|calcitonin]]. |
Osteoblasts, osteocytes, chondroblasts and chondrocytes are derived from the stromal fibroblastic system ('''osteoprogenitor cells'''). Osteoclasts are derived from the haematopoietic system. | Osteoblasts, osteocytes, chondroblasts and chondrocytes are derived from the stromal fibroblastic system ('''osteoprogenitor cells'''). Osteoclasts are derived from the haematopoietic system. | ||
| − | == | + | ==Organisation of Bone== |
| − | The normal progression of bone is from woven bone to lamellar bone, even in pathology, except for [[ | + | The normal progression of bone is from woven bone to lamellar bone, even in pathology, except for [[Craniomandibular Osteopathy|canine craniomandibular osteopathy]] and [[Hypervitaminosis D|hypervitaminosis D]], where lamellar bone is replaced by woven bone. |
===Woven bone=== | ===Woven bone=== | ||
| Line 115: | Line 109: | ||
1. '''Compact bone (cortical)''' | 1. '''Compact bone (cortical)''' | ||
| − | A sheath covers the external surface of long bone. It is thicker in the shaft and thins over the epiphyses. It is | + | A sheath covers the external surface of long bone. It is thicker in the shaft and thins over the epiphyses. It is composed of thin lamallae in a series of concentric tubes arranged around small central canals (collectively known as an '''osteone'''). It forms 80% of the total bone mass and consists of cells and interstitial substance - 30% ossein (type of collagen) and 70% minerals, especially calcium phosphate. |
2. '''Cancellous bone (spongy or trabecular)''' | 2. '''Cancellous bone (spongy or trabecular)''' | ||
| Line 123: | Line 117: | ||
===Laminar bone=== | ===Laminar bone=== | ||
| − | Formed on the periosteal surface of diaphysis. It | + | Formed on the periosteal surface of diaphysis. It accommodates rapid growth of large dogs and farm animals. Plates of woven bone from within the periosteum. As it forms, it fuses with the bone surface. |
==Periosteum and blood supply== | ==Periosteum and blood supply== | ||
| Line 129: | Line 123: | ||
===Periosteum=== | ===Periosteum=== | ||
| − | The periosteum is the specialised sheath of connective tissue covering bone, except at the articular surfaces. It is loosely attached, except at tendon insertions and | + | The periosteum is the specialised sheath of connective tissue covering bone, except at the articular surfaces. It is loosely attached, except at tendon insertions and bony prominences. Histologically, there is an outer layer which is fibrous for support, and an inner layer that is osteogenic. It consists of a rich supply of nerves and lymph vessels, including nutrient, metaphyseal and periosteal arteries. The normal flow of blood from the medulla to the periosteum is due to higher pressures in the medulla. Young animals have a greater blood supply. |
The '''endosteum''' lines the marrow cavity. The '''medullary cavity and cancellous interstitium''' is for bone marrow storage and production. [[Bone Marrow - Anatomy & Physiology#Red marrow|'''Red marrow''']] is a richly vascularized, gelatinous tissue with hematopoeitic properties found abundantly in young animals and [[Bone Marrow - Anatomy & Physiology#Yellow marrow|'''yellow marrow''']] has been converted from red marrow by fat infiltration, causing hematopoeitic properties to dwindle. | The '''endosteum''' lines the marrow cavity. The '''medullary cavity and cancellous interstitium''' is for bone marrow storage and production. [[Bone Marrow - Anatomy & Physiology#Red marrow|'''Red marrow''']] is a richly vascularized, gelatinous tissue with hematopoeitic properties found abundantly in young animals and [[Bone Marrow - Anatomy & Physiology#Yellow marrow|'''yellow marrow''']] has been converted from red marrow by fat infiltration, causing hematopoeitic properties to dwindle. | ||
| Line 147: | Line 141: | ||
'''Stress''': the internal forces resisting the change in dimension caused by the load. | '''Stress''': the internal forces resisting the change in dimension caused by the load. | ||
| − | Cells use strain as a stimulus to adjust mass and architecture according to load. Resorption and osteogenesis happen concurrently to maintain bone integrity. This is mediated by two | + | Cells use strain as a stimulus to adjust mass and architecture according to load. Resorption and osteogenesis happen concurrently to maintain bone integrity. This is mediated by two hormones: |
| − | 1. '''Parathyroid hormone (PTH)''' | + | 1. [[Calcium#Parathyroid Hormone (PTH)|'''Parathyroid hormone (PTH)''']] |
Produced by <u>chief cells in the parathyroid glands</u> in response to <u>decreased</u> serum calcium. In response, osteoclasts increase in number and resorb mineralised matrix to increase Ca in blood. | Produced by <u>chief cells in the parathyroid glands</u> in response to <u>decreased</u> serum calcium. In response, osteoclasts increase in number and resorb mineralised matrix to increase Ca in blood. | ||
| − | 2. '''Calcitonin''' | + | 2. [[Calcium#Calcitonin|'''Calcitonin''']] |
Produced by <u>C-cells in the thyroid glands</u> in response to <u>increased</u> serum calcium. Inhibits osteoclasts. | Produced by <u>C-cells in the thyroid glands</u> in response to <u>increased</u> serum calcium. Inhibits osteoclasts. | ||
In neonates, bone growth predominates and modelling is important. In adults, the formation of bone is balanced by resorption - remodelling. It continues throughout life under the influence of hormones and mechanical pressure. Bone resorption may exceed formation in pathological states (hormonal, trauma, nutritional) or in old age and disuse. | In neonates, bone growth predominates and modelling is important. In adults, the formation of bone is balanced by resorption - remodelling. It continues throughout life under the influence of hormones and mechanical pressure. Bone resorption may exceed formation in pathological states (hormonal, trauma, nutritional) or in old age and disuse. | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==Links== | ==Links== | ||
| + | Click here for information on [[Bone & Cartilage Development - Anatomy & Physiology|Bone and Cartilage Development]]. | ||
Click here for information on [[Bones - Pathology|bone and cartilage pathology]]. | Click here for information on [[Bones - Pathology|bone and cartilage pathology]]. | ||
| − | + | ||
| − | [[Category: | + | {{OpenPages}} |
| − | [[Category: | + | [[Category:Bone and Cartilage - Anatomy & Physiology]] |
| + | [[Category:A&P Done]] | ||
Latest revision as of 23:00, 8 December 2015
Overview
Bone comprises the structure of the skeletal system and provides lever arms for locomotion. Bone also plays important roles in maintaining mineral homeostasis, as well as providing the environment for hematopoesis in marrow.
Short bones - Endochondral ossification continues in the diaphysis, until only the cartilage rim remains.
Long bones - A secondary center of ossification develops in the epiphyses.
See Bone and Cartilage Development
Bone Growth
Length
The epiphyseal growth plate (EGP, physis) is a transverse disc of cartilage between the two ossification centers and allows the bone to continue to grow in length after birth. It then closes. The EGP is a region of continuous chondroblast differentiation and maturation and can be divided into five zones:
- Germinal Zone - chondroblast division at a low rate, and self renewal.
- Proliferation Zone - chondroblast division at a fast rate.
- Maturation Zone - chondroblast differentiation into chondrocytes.
- Hypertrophic Zone - chondrocytes enlarge and then die.
- Dead cells become the matrix for bone growth.
Girth
The periosteum lines the outer surface of the diaphysis of the bone. It has a cellular inner layer, consisting of osteoblasts, and a fibrous outer layer. The endosteum lines the inner surface of the diaphysis of the bone. It contains osteoblasts and osteoclasts. Bone growth occurs by a shift in the equilibrium between osteoblasts and osteoclasts. Osteoblasts on the outside in the periosteum add bone to increase the bone's diameter. Osteoclasts on the inside in the endosteum remove this bone to maintain the bone diameter. When osteoclasts start removing less bone, or osteoblasts start adding more bone, the girth increases.
Bone Remodeling
Primary bone has not yet been remodelled. It contains less mineral and more randomly arranged collagen fibers, known as trabecular organization. Remodelling of bone occurs by haversian canals. The osteoclasts dig out the canal longitudinally through the bone connecting with bone marrow cavity and periosteum. They are followed by anastamosing and branching blood vessels. Concentric bony lamellae are laid down with rows of interconnected lacunae containing osteocytes within. The osteocytes communicate by channels in young bones. Phased resorption happens concurrently.
Haversion canals + lamellae + osteocytes = Haversion system
Types of Bone
1. Long Bone
Found in the limbs and act as levers for locomotion. An elongated diaphysis (shaft) and two epiphyses (ends), each of which encases a center for ossification.
2. Short Bone
Found in places of articulation, such as the carpus and tarsus. All dimensions are relatively equal, generally signifying one center of ossification.
3. Flat Bone
Found in the skull, pelvic girdle, and scapula. It expands in two directions, with a broad surface for attachment of large muscle masses and protection of underlying structures.
4. Irregular Bone
Found in the vertebrae.
5. Sesamoid Bone
Eg. Patella and navicular bone. Found within tendons, where they change direction over prominences that would otherwise cause damage. They form synovial joints with major bones with which they are in contact. They also serve to displace tendon from the axis of the joint, increasing the leverage exerted by the muscle.
6. Splanchnic Bone
Develop in soft organs remote from skeletal connection, eg. os penis.
7. Pneumatic Bone
Excavated to contain air spaces, such as the skull in the instance of paranasal sinuses, and the post-cranial skeleton of birds.
Composition of Bone
Bone is a hard, highly specialised connective tissue . It consists of interconnected cells embedded in a calcified, collagenous matrix. It is a living, dynamic, responsive tissue, growing and remodelling throughout life.
Bone is composed of:
Matrix
Osteoid- An organic, uncalcified, homogeneous substance that stains light pink with H&E . Osteoid consists of type I collagen (90%), which resists tension, and bone-specific proteins (10%), including; Osteonectin, Osteopontin and Osteocalcin.
Mineral- An inorganic component that provides rigidity and consists of a crystalline lattice of calcium phosphate and calcium carbonate. It also contains Mg, Mn, Zn, Cu, Na, F. It accounts for 65% of bone.
Cells
Osteoblasts
A single layer of mesenchymal cells which synthesize bone extracellular matrix (osteoid). When active, they appear plump and cuboidal, with a basophilic cytoplasm. The cell membranes are rich in alkaline phosphatase (ALP). The cells are possibly involved in pumping calcium across membranes. They are promoted by growth factors and have receptors for PTH. They contract in response, which provides space for osteoclasts to attach. When they are inactive, there is less cytoplasm, so they become flattened.
Osteocytes
Osteocytes are embedded in their own matrix; reside within lacunae and are interconnected via channels forming canaliculi. Canaliculi create connections to form a huge neural-like junctional organization. They contact osteoblasts and each other with cytoplasmic processes and reach through canaliculi in the mineralised bone matrix. Osteocytes regulate the composition of bone fluid.
Osteoclasts
Osteoclasts are giant (multinucleate monocytes) cells. Histologically, they are large, often multinucleated cells. They have an acidophilic cytoplasm. They sit in the bone surface depression known as, howship's lacuna. Osteoclasts respond to vitamin D by increasing their numbers and activity (parathyroid independent). Osteoclasts act to resorb the bone extracellular matrix (ECM). They firstly dissolve mineral followed by collagen, using the brush border. They do not have receptors for PTH, but do have receptors for calcitonin.
Osteoblasts, osteocytes, chondroblasts and chondrocytes are derived from the stromal fibroblastic system (osteoprogenitor cells). Osteoclasts are derived from the haematopoietic system.
Organisation of Bone
The normal progression of bone is from woven bone to lamellar bone, even in pathology, except for canine craniomandibular osteopathy and hypervitaminosis D, where lamellar bone is replaced by woven bone.
Woven bone
Woven bone consists of coarse collagen fibres. It is later removed by osteoclasts and replaced by lamellar bone. In adults, it is a sign of a pathological condition (e.g. fracture, inflammation, neoplasia).
Lamellar bone
Lamellar bone consists of orderly layers, which are much stronger than woven bone. There are fine collagen fibres in concentric or parallel laminae. There are two main types of lamellar bone:
1. Compact bone (cortical)
A sheath covers the external surface of long bone. It is thicker in the shaft and thins over the epiphyses. It is composed of thin lamallae in a series of concentric tubes arranged around small central canals (collectively known as an osteone). It forms 80% of the total bone mass and consists of cells and interstitial substance - 30% ossein (type of collagen) and 70% minerals, especially calcium phosphate.
2. Cancellous bone (spongy or trabecular)
Stacks of parallel or concentrically stacked sheets arranged as rods, plates, and arches. In vertebrae, it forms flat bones and forms the hematopoeitic center of epiphyses of long bones. It contains no Haversian systems.
Laminar bone
Formed on the periosteal surface of diaphysis. It accommodates rapid growth of large dogs and farm animals. Plates of woven bone from within the periosteum. As it forms, it fuses with the bone surface.
Periosteum and blood supply
Periosteum
The periosteum is the specialised sheath of connective tissue covering bone, except at the articular surfaces. It is loosely attached, except at tendon insertions and bony prominences. Histologically, there is an outer layer which is fibrous for support, and an inner layer that is osteogenic. It consists of a rich supply of nerves and lymph vessels, including nutrient, metaphyseal and periosteal arteries. The normal flow of blood from the medulla to the periosteum is due to higher pressures in the medulla. Young animals have a greater blood supply.
The endosteum lines the marrow cavity. The medullary cavity and cancellous interstitium is for bone marrow storage and production. Red marrow is a richly vascularized, gelatinous tissue with hematopoeitic properties found abundantly in young animals and yellow marrow has been converted from red marrow by fat infiltration, causing hematopoeitic properties to dwindle.
Biomechanics of Bone
Bone growth and maintenance of normal structure are directly related to mechanical forces. Mechanical forces generate bioelectrical potentials (piezoelectricity), these potentials strengthen bone. Inactivity reduces the potentials, causing bone loss.
Wolff's Law
Bone architecture adapts in response to the loads applied upon it according to mathematical laws;
Load: the external force placed on a structure, F.
Strain: the proportional change in the structure's dimensions.
Stress: the internal forces resisting the change in dimension caused by the load.
Cells use strain as a stimulus to adjust mass and architecture according to load. Resorption and osteogenesis happen concurrently to maintain bone integrity. This is mediated by two hormones:
Produced by chief cells in the parathyroid glands in response to decreased serum calcium. In response, osteoclasts increase in number and resorb mineralised matrix to increase Ca in blood.
2. Calcitonin
Produced by C-cells in the thyroid glands in response to increased serum calcium. Inhibits osteoclasts.
In neonates, bone growth predominates and modelling is important. In adults, the formation of bone is balanced by resorption - remodelling. It continues throughout life under the influence of hormones and mechanical pressure. Bone resorption may exceed formation in pathological states (hormonal, trauma, nutritional) or in old age and disuse.
Links
Click here for information on Bone and Cartilage Development.
Click here for information on bone and cartilage pathology.
Error in widget FBRecommend: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt674b0214011d95_38483477 Error in widget google+: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt674b021409a469_27397096 Error in widget TwitterTweet: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt674b021412c954_85166558
|
| WikiVet® Introduction - Help WikiVet - Report a Problem |