Difference between revisions of "Flea Allergic Dermatitis"
| Line 40: | Line 40: | ||
==References== | ==References== | ||
Nuttall, T (2001) Current concepts in the diagnosis and management of atopic dermatitis. ''In Practice'', '''23(8)''', 442-452. | Nuttall, T (2001) Current concepts in the diagnosis and management of atopic dermatitis. ''In Practice'', '''23(8)''', 442-452. | ||
| + | |||
Perrins and Hendricks (2007) Recent advanced in flea control. ''In Practice'', '''29(4)''', 202-207. | Perrins and Hendricks (2007) Recent advanced in flea control. ''In Practice'', '''29(4)''', 202-207. | ||
[[Category:To_Do_-_Lizzie]] | [[Category:To_Do_-_Lizzie]] | ||
Revision as of 15:56, 4 August 2010
| This article is still under construction. |
| Also known as: | FAD, Flea Allergy Dermatitis, Flea Bite Hypersensitivity, FBH, Flea Dermatosis |
Description
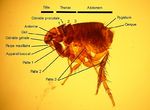
Flea allergic dermatitis is the most common skin disease of dogs and cats worldwide. Cases are caused by flea infestation, mainly by Ctenocephalides felis, the cat flea, but Ctenocephalides canis, Archaeopsylla erinacei, Spylopsyllus cuniculi and Pulex irritans can also be found on cats and dogs. Fleas are blood sucking, wingless insects that live and breed in the hair coat of an animal and often cause pruritis and annoyance. The term flea allergic dermatitis refers to the condition that arises due to hypersensitivity to flea saliva when a flea bites. Flea saliva also contains irritant components that contribute to the disease.
Signalment
Dogs and cats of any age may be afflicted by flea allergic dermatitis.
Diagnosis
Clinical Signs
In dogs, flea allergic dermatitis usually causes marked pruritus, although individual variation does exist. Lesions are most typically seen on the caudal dorsum, the inner and posterior thighs and the umbilical area , but any region may be affected. Within fifteen minutes of receiving a flea bite a papule appears and persits for up to 72 hours, when it forms a crust. However, these lesions may be difficult to appreciate due to the secondary changes that result from self-trauma in response to pruritus. These may include excoriations, erythema, seborrhoea, hyperpigmentation and lichenification. A mild secondary bacterial folliculitis may also be present.
Cats respond to most cutaneous insults in one of four reactions patterns (miliary dermatitis, eosinophilic granuloma complex, head and neck pruritus, symmetrical alopecia). This is also true in flea infestation and flea allergic dermatitis. Miliary dermatitis is by far the most common presentation in this case, but symmetrical alopecia and eosinophilic granuloma complex may also be seen.
Additional Tests
If clinical signs are suggestive of flea allergic dermatitis, demonstration of the presence of fleas or flea faeces will help confirm the diagnosis. Parting the hair and visually inspecting for fleas may be sufficient for this; alternatively a flea comb can be used. Material obtained by combing may be placed on a moistened, light-coloured paper- brown material will "bleed" on the paper if it is indeed flea faeces.
If doubt still remains over the diagnosis of flea allergic dermatitis, the response to a flea control programme will help rule the diagnosis out or in.
Pathology
Grossly, papular dermatitis is seen in combination with any of crusting, erythema, alopecia, excoriations, hyperpigmentation or lichenification. Microscopically, flea allergic dermatitis presents as a hyperplastic superficial perivascular dermatitis. Oedema may be seen, together with an influx of mast cells, eosinophils, lymphocytes and histiocytes.
Treatment
Prognosis
If flea control is implemented correctly, and the client and patient are compliant, prognosis is excellent.
References
Nuttall, T (2001) Current concepts in the diagnosis and management of atopic dermatitis. In Practice, 23(8), 442-452.
Perrins and Hendricks (2007) Recent advanced in flea control. In Practice, 29(4), 202-207.