Fractures
Fracture classification
- Traumatic - normal bone broken by excessive force
- Pathologic - abnormal bone broken by minimal or no trauma
- E.g. due to osteomyelitis, bone neoplasia
- Closed - overlying skin and soft tissue is intact
- Compound - overlying skin and soft tissue are perforated
- Comminuted - bone is shattered at fracture site
- Compresses - the ends of the fracture are impacted into each other
- Avulsed - due to pull of a ligament
- Transverse
- Spiral
Fracture repair
- Fracture
- Ruptured blood vessels -> haemorrhage and clot formation, some ischaemic necrosis
- Dead marrow liquefies and is phagocytosed
- Dead bone is removed by osteoclasts
- Continues long after bone has been united by callus
- Periosteum tears, fragments displaced
- Ruptured blood vessels -> haemorrhage and clot formation, some ischaemic necrosis
- -> Haematoma formation, necrosis of any isolated fragments
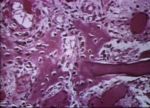
- -> Mesenchymal cells proliferate in haematoma - granulation tissue
- Invading cells: endothelial, fibroblasts, osteoprogenitor
- -> Loose collagenous tissue (primary callus)
- -> Mesenchymal cells differentiate to osteoblasts and chondroblasts
- -> Woven bone (secondary callus)
- External callus - from periosteum
- Periosteal growth eventually bridges the gap between the fracture ends
- Blood supply is outstripped
- Cartilage is produced instead of osteoid
- Blood vessels invade cartilage -> endochondral ossification
- Osteoid becomes ossified
- Internal callus - from endosteum
- Rarely forms cartilage
- May occlude the medullary cavity
- Osteoid remodelled by osteoclastic resorption
- External callus - from periosteum
- -> Mature lamellar bone
- Early reactive fracture repair may be mistaken for osteosarcoma on biopsy
Complications of fracture repair
- Malnutrition
- Lack of adequate blood supply (leads to hypoxia)
- Leads to excess cartilage in callus
- Healing can still occur since this can turn to bone
- Excess movement
- Leads to excess fibrous tissue in callus adn formation of false joint (below)
- Presence of necrotic bone (may form a sequestrum)
- Poor alignment
- Bacterial infection
Pseudoarthrosis
- False joint
- Non-osseus union
- From infection, poor imobilisation, avascularity, extensive tearing damage to periosteum
- Composed of fibrous tissue
- If mobility continues -> hyaline cartilage forms -> neoarthrosis (formation of new joint)
- In Osteodystrophia fibrosa, osteomalacia and rickets - callus forms but does not mineralise
Head and neck of femur fracture
- Vascularisation from joint capsule -> if complete separation -> bone and marrow undergo avascular necrosis
- Fibrovascular tissue and osteogenic cells invade -> deposit new bone
- Resorption of articular cartilage and subchondral bone -> osteoarthropathy commonly develops
Sore shins
- Dorsal metacarpal disease of racehorses
- In 2-3 year olds
- Excessive compressive stress on dorsal cortex of third metacarpal -> microfractures
- Hyperaemic overlying periosteum - -> new bone production to cover the lesion
Causes of Fracture
- The causes of fracture fit into two distinct categories:
- Fracture of trauma
- Breakage of normal healthy bone due to excessive stress pressure of short duration.
- Pathological fracture
- Breakage of bone weakened by some underlying metabolic, inflammatory or neoplastic condition.
- Fracture of trauma
Description of a Fracture
- There are various terms to describe a fracture's appearance.
- Separation of the ends of the fracture may be complete or incomplete.
- When there is no penetration of the overlying skin, a the fracture is described as closed.
- When the sharp ends penetrate the overlying skin, the fracture is compound.
- In this scenario there is the danger of introducing infection.
- Comminuted describes a fracture where there are multiple small fragments of bone at the site of breakage.
- Where the edges of the fracture are impacted into each other, the fracture is said to be compressed.
- When one side of the fracture is depressed below the plane of the other, the term depressed is used.
- This occurs in the flat bones of the skull.
- Microfractures are fractures that are only visible on histological section as cracks in the bone.
- Grossly, there might be evidence of some haemorrhage in the area.
Fracture Repair
- On breakage, there is rupture of the periosteal, cortical and medullary vessels, causing:
- A blood clot in the breakage area.
- Fibrin is the important component.
- Local necrosis of tissue supplied by these vessels.
- This lowers the local pH.
- A blood clot in the breakage area.
- The fate of the blood clot depends upon its location.
- The periosteal portion is lysed and disappears;
- The medullary portion is removed by macrophages.
- The necrotic material is removed by phagocytosis.
- Necrotic bone marrow is removed by macrophages.
- This is a fairly rapid process.
- Osteoclasts remove necrotic bone.
- This is a slow process.
- Necrotic bone marrow is removed by macrophages.
- On the periosteal side, the periosteum proliferates into the clot.
- Forms a fibrous collar around the bone called the soft callus.
- The cells in the inner aspect of the soft callus, particularly those near the fracture fragments, differentiate into osteoblasts.
- Grow across the divide between the two fragments, laying down coarse woven bone.
- The woven bone laid is known as the hard callus.
- This periosteal coarse bone is of utmost importance in repair.
- It is responsible for much of the strength of the fracture repair.
- This is replaced over a period of time by mature compact bone.
- Aligns itself according to the stresses applied to it.
- This periosteal coarse bone is of utmost importance in repair.
- Periosteal cells that are further away from the fracture fragments differentiate into cartilage-producing cells.
- Produce a cone of cartilage between the two fragments.
- As the local pH changes to more alkaline conditions, this cartilage undergoes calcification, with invasion by blood vessels and osteoblasts.
- The cartilage is replaced by bone - endochondral ossification.
- As the local pH changes to more alkaline conditions, this cartilage undergoes calcification, with invasion by blood vessels and osteoblasts.
- Produce a cone of cartilage between the two fragments.
- On the medullary side, the endosteum proliferates and invades the clot, laying down bone.
- This bone may totally occlude the medulla and is later remodelled to reconstitute a patent lumen.
Complications
- There are several possible complications that may arise in the repair of bone.
- Inadequate immobilisation of the fractured ends will lead to incomplete repair by callus formation.
- An intervening mass of fibrocartilage remains, forming a false joint.
- In some cases the false joint can even appear to form a synovial lining.
- If the fractured ends are sufficiently far apart, no substantial callus forms.
- The intervening space is taken up by connective tissue organisation.
- An intervening mass of fibrocartilage remains, forming a false joint.
- Failure to align the fractured ends in proper apposition to one another will produce excessive callus.
- This takes a longer time to be remodelled by the adult compact bone.
- Comminution delays healing due to persistent irritation.
- Infection delays healing due to the effects of the toxins on theproliferating cells.
- May give rise to a systemic infection affecting the rest of the body.