Muscles - Anatomy & Physiology
Jump to navigation
Jump to search
|
|
Introduction
Muscle mass accounts for a large majority of the carcass weight of domestic animals. Muscular contraction is necessary for voluntary and involuntary movement of limbs, stabilization of joints, maintaining luminal diameter (in the case of arteries, bowel, etc), and to produce heat. The number of muscle fibers an individual possesses is determined by genetics and is set at birth, although muscle size and type (i.e. glycolytic to oxidative and vice versa) can be altered. Further muscle development therefore occurs by hypertrophy, rather than hyperplasia of muscle fibers. Three types of muscle can be described:
- Skeletal (also referred to as Striated, Somatic, Voluntary)
- Smooth (also referred to as Visceral)
- Cardiac
Skeletal Muscle
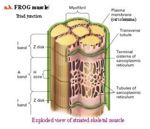
- Each muscle belly is composed of multiple fascicles, each of which consists of a bundle of muscle fibers
- Muscle "fiber" means a single cell, which is multi-nucleate, and known as syncitia
- Parallel fibers: running from origin to insertion)
- Long fibers allow for a faster contraction and a greater range of motion
- Pennate fibers: at an angle to line of pull of an internal tendon or aponeurosis
- Short fibers allow for a greater force capacity
- Parallel fibers: running from origin to insertion)
- Within each fiber are groups of parallel, longitudinal myofibrils
- Myofibrils are arranged as sarcomeres, bound by Z-discs, which are the functional unit of muscle contraction
- Each sarcomere contains 2 separate groups of myofilaments:
- Thin filament, containing Actin, located centrally
- Thick filament, containing Myosin, originating from either side of each Z-disc
- Two basic types of skeletal myofibre:
- Primary: Oxidative
- Grossly red
- High myoglobin level
- Slow rate of contraction
- High oxidative activity
- Function - postural, sustained activity
- Secondary: Glycolytic
- Grossly white
- Low myoglobin level
- Fast rate of contraction
- High glycolytic activity
- Function - exercise, bursts of activity
- Primary: Oxidative
- Neurogenic Contraction: Muscle activation is initiated by a nervous impulse crossing the Neuromuscular Junction
- Each muscle fiber is controlled by a single motor neuron
- The neurotransmitter, Acetylcholine (Ach), binds receptors in the muscle fiber to open Na+ channels
- This causes a wave of depolarization along the sarcoplasmic membrane, further opening voltage-gated Na+ channels, which propagates the signal along the sarcolemma
- Depolarization of the sarcoplasmic reticulum causes Calcium to be released, which activates muscle contraction
- Muscle contraction occurs when (thin) Actin filaments slide past (thick) Myosin filaments
- Myosin heads bind Actin subunits, forming cross-bridges, hydrolyzing ATP and providing energy for contraction
- Myosin heads undergo power stroke, displacing Actin and releasing ADP and Pi
- Control of skeletal muscle activity is regulated by the thin filament
- In the off state, tropomyosin coiled-coils block the helical grooves of the actin filament
- Tropomyosin movement relieves the steric block, allowing access to myosin binding sites
- Calcium regulates muscle contraction by binding troponin-C, which is attached to the thin filament
- This causes inhibition of the steric block keeping Actin and Myosin from interacting
- Increased Calcium causes a negative feedback inhibition of Ca release, and it is pumped back into the sarcoplasmic reticulum by the Ca/ATPase pump
- Types of Muscle Contraction:
- Concentric: muscle shortens and bones are brought closer together
- Isometric: muscle is active but does not change in length (force without motion)
- Eccentric: muscle is active while lengthening
Smooth Muscle
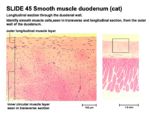
- Slower contraction and relaxation
- Undeveloped sarcoplasmic reticulum means that smooth muscle depends on the plasmalemma release of Ca: affects contractile properties
- Smooth muscle lacks troponin
- Control of smooth muscle contraction involves thin and thick filament regulation
- Thin filament regulation is carried out by the actin binding protein, Caldesmon, which binds the thin filament and blocks myosin access
- Calmodulin (activated by binding Ca) binds caldesmon and causes its dissociation from actin, enabling contraction
- Thick filament regulation occurs by the phosphorylation of the regulatory light chain (RLC)
- Calmodulin-Ca binds and activates myosin light chain kinase (MLCK)
- MLCK then phosphorylates RLC, turning myosin on
- Myosin light chain phosphatase (MLCP) switches myosin off
- Single Unit: myogenic contraction; depolarized by gap junctions; eg. intestinal smooth muscle
- Multi-unit: neurogenic contraction; no gap junctions; eg. iris
Cardiac Muscle
- Structural: striated but uninucleate, highly vascularized
- Gap junctions concentrated at intercalated discs
- Myogenic Contraction spreads cell to cell and does not depend on nervous imput to individual cells
- Areas of low electrical resistance allow rapid spread of action potentials
- Contraction is regulated by autonomic neurons and circulating hormones
- Contractile mechanism similar to skeletal muscle: increase cytosolic Ca
- Ca influx across plasma membrane AND sarcoplasmic reticulum
- Action potential has a prolonged plateau phase
Tendon
- Connective tissue point of attachment between muscle and bone
- Consists of dense collagen type 1 fibres and fibroblasts (tenocytes)
- Possess great tensile strength
- Highly elastic: important in absorbing and storing energy
- Elastic recoil provides a crucial role in locomotion
- Can be protected by sesamoid bones at a point of angulation over bony surface
- Fluid-filled bursae provide cushioning and protection where necessary
- Walls and sheaths resemble synovial joint components