Difference between revisions of "Tick-Borne Fever"
| (23 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
| − | + | {{OpenPagesTop}} | |
| + | Also Known As: '''''Pasture Fever''''' — '''''Tickborne Fever''''' — '''''Ruminant Anaplasmosis''''' — '''''TBF''''' | ||
| − | + | Caused By: '''''Anaplasma phagocytophilum''''', previously known as '''''Ehrlichia phagocytophila''''' | |
| − | |||
| − | |||
| − | |||
| − | + | ==Introduction== | |
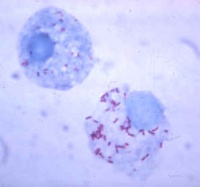
| − | + | [[File:Anaplasmosis.jpg|thumb|200px|right|''Rickettsia'' spp. inside tick haemolymph cells. Sourced from Wikimedia Commons]] | |
| − | + | [[File:Swollen tick-SteveFE.jpg|thumb|200px|right|''Ixodes'' tick. Sourced from Wikimedia commons]] | |
| − | + | Tick Borne Fever is a '''[[Rickettsiales |rickettsial]]''' disease affecting the '''[[Leucocytes |white blood cells]]''' of sheep and cattle, causing '''anaemia''' and seasonal “pasture fever”. | |
| − | |||
| − | |||
| − | + | Seasonal pasture fever occurs in cattle that are returned to tick infected pasture in the Spring. | |
| − | |||
| − | |||
| − | + | Human granulocytic ehrlichiosis, the '''zoonotic''' form of TBF is a potentially '''fatal''' disease reported in the UK, Europe and USA. | |
| − | |||
| − | |||
| − | |||
| − | == | + | ==Signalment== |
| − | + | TBF naturally affects primarily sheep and cattle, and less commonly, deer, horses and dogs. | |
| + | ==Distribution== | ||
| + | TBF has worldwide distribution including the UK. It is transmitted by '''''[[Ixodes spp. |Ixodes]]''''' ticks. Both adults and nymphs can transmit the disease. Transmission is '''[[Tick Disease Transmission |trans-stadial]].''' | ||
| − | Use | + | ==Clinical Signs== |
| + | TBF causes '''multisystemic''' disease, causing cardiovascular, gastrointestinal, respiratory, reproductive and neurological signs, and also lymphadenopathy and wasting disease. | ||
| + | |||
| + | '''Severe haematological changes''' including profound [[:Category:Anaemia|'''anaemia''']] and '''leucopaenia''' cause significant clinical signs. | ||
| + | |||
| + | Initial [[lymphocytopaenia]] and '''prolonged [[neutropaenia]]''' are also features of TBF. | ||
| + | |||
| + | A profound '''[[eosinophilia]]''' will occur for 17-20 days post-infection. <ref>Miert, A. S. J. P. A. Mvan., Duin, C. T. Mvan., Schotman, A. J. H., Franssen, F. F. (1984) '''Clinical, haematological and blood biochemical changes in goats after experimental infection with tick-borne fever. '''''Vet Parasitology, ''16(3/4):225-233; 29 </ref> | ||
| + | |||
| + | Low serum Alkaline Phosphatase (ALP) and decreased zinc, iron and albumin are also common biochemical findings, along with high [[urea]], [[creatinine]] and [[bilirubin]]. | ||
| + | |||
| + | Recovered animals develop immunity but it is unknown how long this is effective for. | ||
| + | |||
| + | ==Diagnosis== | ||
| + | Haematological and Biochemical changes as listed above along with '''marked pyrexia''' are highly suggestive, especially if historical findings are conducive. | ||
| + | |||
| + | Demonstration of the '''organism''' in the '''[[Leucocytes |leucocytes]]''' in peripheral blood is confirmative. | ||
| + | |||
| + | On '''post-mortem''' examination, the '''[[Spleen - Anatomy & Physiology|spleen]]''' is enlarged and mild liver damage is common. Lesions within the [[Lungs - Anatomy & Physiology|'''lung''']] are present and contain mononuclear infiltrate on histopathology. Thickening, ulceration and haemorrhage of the gastrointestinal tract become worse distally. | ||
| + | |||
| + | The parasites may be visible within the neutrophils in sections of liver and lung. | ||
| + | |||
| + | Antibodies can be detected using [[FAT|'''Indirect Immunofluorescence''' (IFAT)]], '''[[Complement Fixation]]''' and Immunoelectrophoresis (CIEP). | ||
| + | |||
| + | ==Treatment== | ||
| + | ''A. phagocytophilum'' is susceptible to '''oxytetracycline, sulphamethazine, sulphadimidine, doxycycline''' and '''trimethoprim-sulphonamides'''. | ||
| + | |||
| + | ==Control== | ||
| + | [[Tick Control|Control of the tick vector ]]is expensive but effective. | ||
| + | Use of [[Ectoparasiticides |ectoparasiticides]] and tick resistant breeds is also valuable. | ||
| + | |||
| + | ==Human Granulocytic Ehrlichiosis== | ||
| + | Causes fever, malaise, headaches, sweats, nausea, confusion, anorexia, vomiting, weakness, diarrhoea, pneumonia, vertigo, seizures, GI bleeding and a skin rash.<ref>Bakken, J. S., Krueth, J., Tilden, R. L., Dumler, J. S., Kristiansen, B. E. (1996). '''Serological evidence of human granulocytic ehrlichiosis in Norway. '''''Eur J Clin Microbiol Inf Dis,'' 15(10):829-832; 12</ref> | ||
| + | |||
| + | |||
| + | {{Learning | ||
| + | |flashcards = [[Tick-Borne Fever Flashcards]] | ||
| + | }} | ||
| + | |||
| + | |||
| + | ==References== | ||
| + | <references/> | ||
| + | {{CABI source | ||
| + | |datasheet = [http://www.cabi.org/ahpc/?compid=3&dsid=61126&loadmodule=datasheet&page=2144&site=160 tick-borne fever] | ||
| + | |date = 6 June 2011 | ||
| + | }} | ||
<br><br><br> | <br><br><br> | ||
| − | |||
| + | {{review}} | ||
| + | |||
| + | {{OpenPages}} | ||
| + | |||
| + | [[Category:Rickettsiales]][[Category:Cattle Bacteria]][[Category:Sheep Bacteria]][[Category:Goat Bacteria]] | ||
| + | [[Category:Zoonoses]] | ||
| + | [[Category:Cardiovascular Diseases - Cattle]][[Category:Respiratory Diseases - Cattle]][[Category:Alimentary Diseases - Cattle]][[Category:Reproductive Diseases - Cattle]][[Category:Neurological Diseases - Cattle]][[Category:Lymphoreticular and Haematopoietic Diseases - Cattle]] | ||
| − | [[Category: | + | [[Category:Cardiovascular Diseases - Sheep]] |
| − | [[Category: | + | [[Category:Respiratory Diseases - Sheep]] |
| + | [[Category:Alimentary Diseases - Sheep]][[Category:Reproductive Diseases - Sheep]][[Category:Neurological Diseases - Sheep]] | ||
| + | [[Category:Lymphoreticular and Haematopoietic Diseases - Sheep]] | ||
| + | [[Category:CABI Expert Review]][[Category:CABI AHPC Pages]] | ||
| + | [[Category:Nick L]] | ||
| + | [[Category:Cardiology Section]] | ||
Latest revision as of 17:30, 17 October 2013
Also Known As: Pasture Fever — Tickborne Fever — Ruminant Anaplasmosis — TBF
Caused By: Anaplasma phagocytophilum, previously known as Ehrlichia phagocytophila
Introduction
Tick Borne Fever is a rickettsial disease affecting the white blood cells of sheep and cattle, causing anaemia and seasonal “pasture fever”.
Seasonal pasture fever occurs in cattle that are returned to tick infected pasture in the Spring.
Human granulocytic ehrlichiosis, the zoonotic form of TBF is a potentially fatal disease reported in the UK, Europe and USA.
Signalment
TBF naturally affects primarily sheep and cattle, and less commonly, deer, horses and dogs.
Distribution
TBF has worldwide distribution including the UK. It is transmitted by Ixodes ticks. Both adults and nymphs can transmit the disease. Transmission is trans-stadial.
Clinical Signs
TBF causes multisystemic disease, causing cardiovascular, gastrointestinal, respiratory, reproductive and neurological signs, and also lymphadenopathy and wasting disease.
Severe haematological changes including profound anaemia and leucopaenia cause significant clinical signs.
Initial lymphocytopaenia and prolonged neutropaenia are also features of TBF.
A profound eosinophilia will occur for 17-20 days post-infection. [1]
Low serum Alkaline Phosphatase (ALP) and decreased zinc, iron and albumin are also common biochemical findings, along with high urea, creatinine and bilirubin.
Recovered animals develop immunity but it is unknown how long this is effective for.
Diagnosis
Haematological and Biochemical changes as listed above along with marked pyrexia are highly suggestive, especially if historical findings are conducive.
Demonstration of the organism in the leucocytes in peripheral blood is confirmative.
On post-mortem examination, the spleen is enlarged and mild liver damage is common. Lesions within the lung are present and contain mononuclear infiltrate on histopathology. Thickening, ulceration and haemorrhage of the gastrointestinal tract become worse distally.
The parasites may be visible within the neutrophils in sections of liver and lung.
Antibodies can be detected using Indirect Immunofluorescence (IFAT), Complement Fixation and Immunoelectrophoresis (CIEP).
Treatment
A. phagocytophilum is susceptible to oxytetracycline, sulphamethazine, sulphadimidine, doxycycline and trimethoprim-sulphonamides.
Control
Control of the tick vector is expensive but effective. Use of ectoparasiticides and tick resistant breeds is also valuable.
Human Granulocytic Ehrlichiosis
Causes fever, malaise, headaches, sweats, nausea, confusion, anorexia, vomiting, weakness, diarrhoea, pneumonia, vertigo, seizures, GI bleeding and a skin rash.[2]
| Tick-Borne Fever Learning Resources | |
|---|---|
 Test your knowledge using flashcard type questions |
Tick-Borne Fever Flashcards |
References
- ↑ Miert, A. S. J. P. A. Mvan., Duin, C. T. Mvan., Schotman, A. J. H., Franssen, F. F. (1984) Clinical, haematological and blood biochemical changes in goats after experimental infection with tick-borne fever. Vet Parasitology, 16(3/4):225-233; 29
- ↑ Bakken, J. S., Krueth, J., Tilden, R. L., Dumler, J. S., Kristiansen, B. E. (1996). Serological evidence of human granulocytic ehrlichiosis in Norway. Eur J Clin Microbiol Inf Dis, 15(10):829-832; 12

|
This article was originally sourced from The Animal Health & Production Compendium (AHPC) published online by CABI during the OVAL Project. The datasheet was accessed on 6 June 2011. |
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
Error in widget FBRecommend: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt662107636045b3_48736722 Error in widget google+: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt66210763639361_99274961 Error in widget TwitterTweet: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt66210763668698_11008783
|
| WikiVet® Introduction - Help WikiVet - Report a Problem |
- OpenPages
- Rickettsiales
- Cattle Bacteria
- Sheep Bacteria
- Goat Bacteria
- Zoonoses
- Cardiovascular Diseases - Cattle
- Respiratory Diseases - Cattle
- Alimentary Diseases - Cattle
- Reproductive Diseases - Cattle
- Neurological Diseases - Cattle
- Lymphoreticular and Haematopoietic Diseases - Cattle
- Cardiovascular Diseases - Sheep
- Respiratory Diseases - Sheep
- Alimentary Diseases - Sheep
- Reproductive Diseases - Sheep
- Neurological Diseases - Sheep
- Lymphoreticular and Haematopoietic Diseases - Sheep
- CABI Expert Review
- CABI AHPC Pages
- Nick L
- Cardiology Section