Innate Immune System
|
|
Introduction
The Innate immune system is the body's first barrier of defense to infection. It relies on an older, more generic, and faster acting set of tools than the adaptive system. While the adaptive system is essential for a specific response to infection, it is ultimately the innate system that conquers foreign attackers through means of phagocytosis.
- Non-specific protective mechanisms include such innate factors as:
- Physical barriers
- Skin
- Ciliated mucous membranes
- Commensal organisms
- Humoral factors
- Lysozyme
- Complement
- Interferons
- Cellular mechanisms
- Phagocytosis
- Factors which regulate species specificity
- Membrane receptors for pathogens
- Nutritional requirements
- Temperature
- pH
- Physical barriers
- Mechanisms of innate immunity are always present and generally unchanging
- Adaptive immunity is acquired only on contact with the infectious agent (antigen) and therefore does not function before first contact with the antigen
Actions of the Innate Immune System
Recognition of Microorganisms
- The innate immune system recognises components of pathogens which are intrinsically foreign (i.e. not present on normal mammalian cells), such as:
- Lipopolysaccharides of gram-negative bacteria
- Peptidoglycans of gram-positive bacteria
- Mannose sugars
- D-isoform amino acids
- These are given away as foreign by expressing pathogen-associated molecular patterns (PAMPs)
- PAMPs are recognised by pattern recognition receptors (PRRs) expressed on mammalian cells
- Pattern recognition receptors are expressed on many different cell types, not just on phagocytes
- Not all are expressed by all cells: different cell types express a different range of PRRs
- PRRs are either intracellular, membrane-associated or soluble:
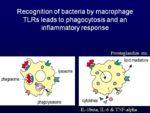
- Recognition of pathogens via the cellular PRRs results in phagocytosis and inflammation
- Recognition of pathogens via the humoral PRRs results in various killing mechanisms
- Engagement of PRRs by PAMPs triggers:
- Phagocytosis
- The expression of cytokines, which brings about inflammation and other immune responses
| Receptor | Location | Ligands |
|---|---|---|
| TLR2 (Toll-like receptor) | Cell Membrane | Peptidoglycan of gram +ve bacteria |
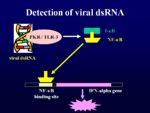
| TLR3 | Cell Membrane | dsRNA of RNA viruses (e.g. avian influenza) |
| TLR4 | Cell Membrane | Lipoplysaccharide from gram-negative bacteria (e.g. E. coli, Salmonella) |
| TLR5 | Cell Membrane | Bacterial flagellin |
| TLR9 | Cell Membrane | Bacterial DNA (CpG DNA) |
| C-type lectins | Soluble | Carbohydrates, all bacteria, dead cells |
| fmlf | Soluble | Formyl peptides (i.e. all bacteria) |
| Complement receptors | Soluble | Fixed complement components (e.g. iC3b) |
| NOD2 | Cytoplasm | Peptidoglycan of gram +ve bacteria |
| dsRNA-dependent Protein Kinase Receptor | Cytoplasm | ds RNA of RNA viruses |
Phagocytosis
- Phagocytosis is a very primitive system of defence against infection
- Even exists in invertebrates
- Phagocytosis is a form of endocytosis (cell eating), it is the method of removal of bacteria and dead cells by vesicular internalisation
- The internalised vesicle is referred to as the "phagosome"
- Lysosomes, which contain a large range of enzymes, fuse with the phagosome, killing the microbes in an energy-dependent way
- Oxygen-dependent degradation utilizes Oxygen and chlorine free-radicals, Hydrogen peroxide, and Nitric oxide
- Oxygen-independed degradation depends on granules containing proteolytic enzymes such as Defensins, Lysozyme, and cationic proteins
- In addition, these granules contain antimicrobial elements such as lactoferrin
- Microbes are then digested by a number of different catabolic enzymes
- Glycosidases: Digest carbohydrates
- Lipases: Digest lipids
- Proteases: Digest protein
- Waste products of phagocytosis are either exocytosed or further degraded by the phagocyte
- Neutrophils and macrophages are phagocytic
- Opsonins promote and accelerate phagocytosis
- Phagocytic cells target pathogens by using cell membrane receptors (PRRs) that recognize intrinsically foreign components of microorganisms (pathogen-associated molecular patterns; PAMPs)
Tools of Innate Immunity
Barriers
Physical Barriers
Skin
The simplest way to avoid infection is to prevent microorganisms gaining access to the body. The skin has an external coating of dead cells (cuticle) that, when intact, is impermeable to most infectious agents.
- Very few pathogens are capable of penetrating the thick stratified squamous epithelium of the skin (and lower urinary tract).
- Infection becomes a problem when there is:
- Skin loss: e.g. burns
- A break in the skin: e.g. wounds
- Infection becomes a problem when there is:
Mucus Membranes
- Thin epithelial surfaces are necessary for the normal physiological functions of the bodies mucus membranes (ie absorption and gas exchange).They are therefore more susceptible to infection
- The body uses alternative protective mechanisms in these areas:
- The mucociliary escalator of the respiratory tract (assisted by coughing and sneezing)
- Peristalsis, vomiting & diarrhoea when necessary removes microorganisms from the GIT
- The body uses alternative protective mechanisms in these areas:
Biochemical Barriers
- Lactic and fatty acids in sweat and sebaceous secretions are directly bacteriocidal
- Enzymes e.g. lysozyme in saliva, sweat & tears and Gastric acid denature microorganisms
- Mucus itself is acidic, indigestible and traps microorganisms
Commensal Organisms
- Out-compete pathogens at mucosal and epithelial surfaces and produce natural antibiotics
- When commensals are disturbed, infection with opportunistic organisms is increased
- E.g. Candida (thrush) or Clostridium difficile (infectious diarrhoea)
Humoral Factors
Lysozyme
- Lysozyme is one of the major bactericidal agents in secretions
- Helps to protect vulnerable sites such as the eyes and nasal passages
- Exerts bactericidal effects by digesting bacterial cell walls
- Gram-positive bacteria are more sensitive to lysozyme action than gram-negative bacteria
- The outer membrane of gram-negative bacteria helps to protect them
Complement
- The Complement system is a group of about 30 proteins within the body fluids of all vertebrates and some invertebrates
- Complement promotes phagocytosis or causes lysis of an invading organism
- Complement acts as a cascade, like the blood clotting system
- The early enzymes in the cascade are bound to invading bacteria and fungi
- They have an affinity for components of microbial cell membranes
- This binding initiates a cascade so that the binding of one molecule will eventually lead to the fixation of millions of later molecules
- The early enzymes in the cascade are bound to invading bacteria and fungi
- The early components act as targets for phagocytes
- The later components punch holes in bacteria, causing their lysis
Interferons
- Lysozyme and complement have only marginal effects on virus infections because these are intracellular
- The body has evolved non-specific mechanisms to protect against viruses
- The most notable of these is the interferons
- The body has evolved non-specific mechanisms to protect against viruses
- Interferons are small polypeptides produced mainly by virus-infected cells
- Interact with uninfected cells and render them resistant to infection
- This resistance is mainly due to the production of enzymes that digest viral nucleic acids
- Interact with uninfected cells and render them resistant to infection
Cellular responses
- If pathogens breach the barriers formed by the skin and mucus membranes, they must be detected and destroyed by cellular and humoral means
- The cells involved with innate protection are:
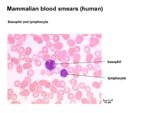
- Blood granulocytes, or Polymorphonuclear Cells
- Notable for their multi-lobed nuclei
- Neutrophils: phagocytose bacteria
- Eosinophils: kill parasites by the release of granules
- Basophils/ mast cells: kill parasites by the release of granules
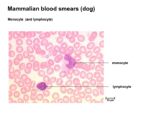
- Blood monocytes: phagocytose bacteria
- Tissue mast cells and macrophages: phagocytose bacteria
- Blood granulocytes, or Polymorphonuclear Cells
- Effectively, innate cellular response seeks to hold off the infection until the adaptive response can back it up with a more specific attack
Macrophages
- The role of macrophages in Innate Immunity is to act as primary phagocytes
- Macrophages are present within tissues and take the form of distinct, tissue-specific populations:
- Alveolar macrophages
- Tissue histiocytes
- Glomerular macrophages
- Hepatic Küpffer cells
- CNS microglia
- Sinus-lining macrophages of the lymph nodes and spleen
- Monocytes (immature macrophages) are circulating phagocytes
- Circulate for 6-8 hours
- Can function as phagocytes within the blood and as newly migrated cells in tissues
- Chiefly function to replace the various tissue macrophage populations
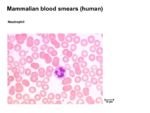
Neutrophils
- Neutrophils are the principal, highly active phagocytes in the blood
- Comprise 30-70% of white blood cells depending on species
- Kill and digest microbes in a similar way as macrophages
- Neutrophils can also cause extracellular bacterial killing by disrupting bacterial membranes
- Secrete small antibacterial peptides
- E.g. defensins and bactenecins
- Secrete small antibacterial peptides
- Neutrophils produce vasoactive peptides
- E.g. histamine and bradykinin
- Cause a great increase in extravasation of blood granulocytes and monocytes and plasma proteins at the site of infection
- Neutrophils are the archetypal cell associated with acute inflammation
- Are attracted to sites of inflammation by:
- Complement activation
- Cytokine production
- Changes to vascular endothelium
- Neutrophil activation in an inflammatory lesion results in the release of prostaglandins
- Responsible for vasoactive changes and for pain
- Are attracted to sites of inflammation by:
- The accumulation of dead and dying neutrophils at the site of infection is called pus
- Their removal from the site after the removal of infection is an important step in the resolution of the lesion
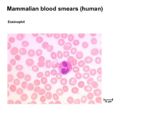
Eosinophils
- Eosinophils are less common than neutrophils, and they are not phagocytic
- Make up <5% of the leukocytes in normal blood
- Eosinophil numbers are increased:
- Slightly during the resolution phase of inflammation
- Many-fold in parasite-infected animals
- The presence of a large proportion of eosinophils in a blood smear is highly indicative of parasitaemia
- Mainly function by targeting the surface of parasites by means of specific antibody or complement
- Release a large range of toxic molecules that break down the parasite integument
- Prominent in allergic (anaphylactic) reactions
Basophils / Mast Cells
- Basophils/mast cells are principally localized at epithelial surfaces
- Very small numbers are present in blood
- less than 0.5% circulating leukocytes
- Very small numbers are present in blood
- They have two principal functions:
- Induction of acute inflammation
- Trauma and/ or bacterial infection causes the production of cytokines by the mast cells that induce a classical acute inflammatory response
- Response to parasite infection
- Specific IgE binds cells
- Subsequent contact with antigen causes the mast cells to degranulate
- Release enzymes and vasoactive substances that can result in a high level of mucus secretion and smooth muscle contraction
- Induction of acute inflammation
- Also produce factors that influence local host cell physiology
- Various mediators increase the ratio of phagocyte to microbe
Innate Immunity to Viruses
Because viruses invade host cells to take over a host's cellular machinery, the innate system has a more difficult time detecting viruses as foreign agents. However, there is a give-away element of the viral attack that the innate system can recognize: the double-stranded RNA (dsRNA) produced by a virus in its replication phase. Because mammalian cells only ever produce single-stranded RNA, the presence of dsRNA signals a forein intruder. dsRNA can be detected by TLR-3R on the cell surface or intracellularly by the presence of dsRNA-dependent protein kinase.
The innate resonse to viral attack also depends on the presence of Type-1 Interferons, which are produced by all cells on recognition of a viral attack. Interferons serve to increase degradation of mRNA, inhibit protein synthesis, and increase the effectiveness of the adaptive response by increasing antigen presentation to antibody.
Lastly, the final line of defense for the innate response to viruses lies in the actions of Natural Killer (NK) cells. These warriors monitor the production of MHC (Major Histocompatibility Complex) on the surface of cells, which is produced as part of the adaptive response. A cell whose cellular machinery is compromised by viral infection will experience a drop in the amount of MHC it produces. When a cell's MHC production drops, NK cells are triggered to phagocytose these cells. As such, this is a non-specific targeting based simply on the ability of a cell to function normally, which also lends them to playing a role in targeting malignant cells. NK cells are incapable of directly targeting viral infection.
Innate Immunity to Bacteria
The innate response to bacterial infection lies in its first-response role of detection of a foreign organism. By using the above described tools of Pattern-Recognition Receptors (PRRs), the innate response flags up problems while the adaptive response gets itself organized. Once a foreign organism is detected, the innate system responds by engaging in cell warfare via phagocytosis and engaging the inflammatory response. The release of inflammatory cytokines will cause an increase in vasodilation, vascular permeability and an influx of white blood cells. Neutrophils take on their primary role as phagocytes in this phase. In addition, systemic effects of inflammatory cytokines will sustain a rise in core temperature (fever), the release of acute phase proteins from the liver, and bone marrow mobilization as the need for white blood cells production is increased. Acute phase proteins will bind to bacterial cell walls, enhancing neutrophil, macrophage, and complement-initiated phagocytosis.