Difference between revisions of "Principles of Fluid Therapy"
| Line 28: | Line 28: | ||
#Colloids | #Colloids | ||
#Blood Products | #Blood Products | ||
| + | |||
| + | If there is an electrolyte imbalance present then it may be necessary to add the appropriate electrolyte solution. | ||
==Fluid Rate Calculations== | ==Fluid Rate Calculations== | ||
| Line 65: | Line 67: | ||
These calculations are then added together to allow for the total fluid requirement in a 24 hour period. It is important to assess these requirements on a daily basis as losses may be increased/reduceed for example. | These calculations are then added together to allow for the total fluid requirement in a 24 hour period. It is important to assess these requirements on a daily basis as losses may be increased/reduceed for example. | ||
| − | |||
The calculated fluid requirement is multiplied by the bodyweight of the individual patient to give the total amount of fluid required for that patient as ml/24hr period. This is then further calculated depending on whether a ddrip pump is used or fluid rate is adjusted manually as shown below. | The calculated fluid requirement is multiplied by the bodyweight of the individual patient to give the total amount of fluid required for that patient as ml/24hr period. This is then further calculated depending on whether a ddrip pump is used or fluid rate is adjusted manually as shown below. | ||
| Line 88: | Line 89: | ||
===Anaesthesia=== | ===Anaesthesia=== | ||
====Pre-anaesthetic==== | ====Pre-anaesthetic==== | ||
| + | Before an anaesthestic is performed, it is important to stabilise a patient, both fluid deficits and any electrolyte or acid-base inbalances. In many cases, it is ideal to have a minimum blood database. This should include Packed Cell Volume (PCV) and Total Protein (TP) and if possible urea, creatinine, electrolyes and glucose. If there is any evidence of haemoconcentration, azotemia, or electrolyte imbalances then the patient should be given fluids to correct these abnormalities before the anaesthetic. When giving fluids ideally they should be warmed to help the patient maintain a normal body temperature. | ||
| + | |||
| + | |||
====Intra-anaesthetic==== | ====Intra-anaesthetic==== | ||
| + | During an anaesthetic, glucose levels should be closely monitored, especially patients with diabetes, liver disease or paediatric patients. If necessary it is then possible to add glucose or dextrose to the fluid the patient is receiving. | ||
| + | |||
| + | Some patients may develop an anaesthetic-induced hypotension from the side-effects of the agents used to induce and maintain anaesthesia. Fluids are therefore often given as a preventative measure. | ||
| + | |||
| + | If there is significant blood loss during a procedure, it is necessary to replace these losses, either using blood products or an appropriate fluid. | ||
| + | |||
| + | |||
====Post-anaesthetic==== | ====Post-anaesthetic==== | ||
| + | If a patient has been receiving fluids during a procedure, it is often continued after until the patient is either stable and fully recovered from the anaesthetic. The length of time the fluids continue for after the procedure is dependent on the individual patient and the individual case. | ||
| + | |||
| + | |||
===Cardiac=== | ===Cardiac=== | ||
| + | It is important to avoid fluid overload in cardiac patients who often have reduced cardiac function. | ||
| + | |||
| + | |||
===Central Nervous System=== | ===Central Nervous System=== | ||
| + | Patients with head trama or increased intracranial pressure are particularly suscetible to insufficient or excessive fluid loading. It is therefore with care that fluids are administered and monitored. The choice of fluid is dependent on the other clinical signs of the patient such as haemodynamics. The status of the blood brain barrier is an important consideration in any patient and in the selection of fluid. However, fluids containing glucose should be avoided in these patients. | ||
Revision as of 20:59, 12 April 2009
| This article is still under construction. |
What is Fluid Therapy?
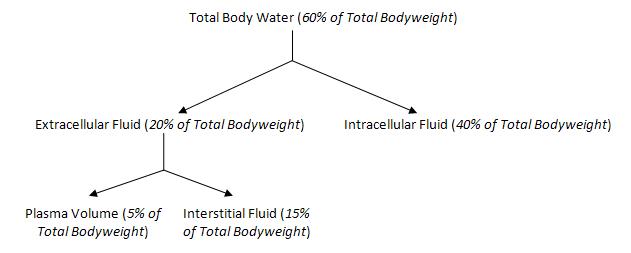
Fluid Therapy is the administration of fluids to a patient as a treatment or preventative measure. It can be administered via an intravenous, intraperitoneal and subcutaneous routes. 60% of total bodyweight is accounted for by the total body water. This can further be divided into intracellular or extracellular as shown below.
Fluid therapy is indicated when there is a loss of fluid to any part of these compartments. The severity of the fluid loss, and the compartment which is has been lost from with influence the choice of fluid.
Indications
- Hypotension
- Hypovolemia
- Electrolyte, metabolic and acid base disorders
- Decreased oxygen delivery
- Geriatric patients at risk of organ failure
Definitions
- Osmosis is the net movement of water across a semi permeable membrane. The movement is caused by a concentration gradient due to different solute concentrations.
- Osmotic Pressure is the pressure caused by the solutes within the solution. The solute concentration prevents water movement across the membrane.
- Tonicity is the term used to compare the osmotic pressure of different solutions
- A hypotonic solution is one that has an osmotic pressure lower than plasma.
- A isotonic solution is one that has an osmotic pressure the same than plasma.
- A hypertonic solution is one that has an osmotic pressure higher than plasma.
Types of Fluids
- Crystalloids
- Colloids
- Blood Products
If there is an electrolyte imbalance present then it may be necessary to add the appropriate electrolyte solution.
Fluid Rate Calculations
When calculating the fluid requirements of a patient, there are 3 elements to consider -
- Replacement
- Maintainance
- Ongoing Losses
Replacements are calculated based on the level of dehydration. Dehydration is based upon clinical assessment of each individual patient. Most commonly, skin tent is used for assessment. To calculate the amount required for replacement within a 24 hour period, the percentage dehydration is used in the following calculation.
| Replacement = % Dehydration x Bodyweight (kg) x 10 |
|---|
Maintainance is the basic rate which a patient requires during a 24 hour period. It is commonly calculated as 50ml/kg/24hr, or 2ml/kg/hr.
Ongoing losses are calculated based on a predicted fluid amount lost by a patient within a 24 hour period. Common losses include vomitting and diarrhoea. It is often helpful here if the owners are able to give a detailed history as this makes it easier to predict the pattern of losses. In some patients there may be no ongoing losses and so this step can be skipped. To calculate the fluid requirement, the following calculation is used.
| Ongoing losses = Amount per loss (ml/kg) x Bodyweight (kg) x No. of losses |
|---|
These calculations are then added together to allow for the total fluid requirement in a 24 hour period. It is important to assess these requirements on a daily basis as losses may be increased/reduceed for example.
The calculated fluid requirement is multiplied by the bodyweight of the individual patient to give the total amount of fluid required for that patient as ml/24hr period. This is then further calculated depending on whether a ddrip pump is used or fluid rate is adjusted manually as shown below.
| Requirement per hour (ml/hr) = Requirement per day (ml/24hr) ÷ 60
|
|---|
Special Considerations
Anaesthesia
Pre-anaesthetic
Before an anaesthestic is performed, it is important to stabilise a patient, both fluid deficits and any electrolyte or acid-base inbalances. In many cases, it is ideal to have a minimum blood database. This should include Packed Cell Volume (PCV) and Total Protein (TP) and if possible urea, creatinine, electrolyes and glucose. If there is any evidence of haemoconcentration, azotemia, or electrolyte imbalances then the patient should be given fluids to correct these abnormalities before the anaesthetic. When giving fluids ideally they should be warmed to help the patient maintain a normal body temperature.
Intra-anaesthetic
During an anaesthetic, glucose levels should be closely monitored, especially patients with diabetes, liver disease or paediatric patients. If necessary it is then possible to add glucose or dextrose to the fluid the patient is receiving.
Some patients may develop an anaesthetic-induced hypotension from the side-effects of the agents used to induce and maintain anaesthesia. Fluids are therefore often given as a preventative measure.
If there is significant blood loss during a procedure, it is necessary to replace these losses, either using blood products or an appropriate fluid.
Post-anaesthetic
If a patient has been receiving fluids during a procedure, it is often continued after until the patient is either stable and fully recovered from the anaesthetic. The length of time the fluids continue for after the procedure is dependent on the individual patient and the individual case.
Cardiac
It is important to avoid fluid overload in cardiac patients who often have reduced cardiac function.
Central Nervous System
Patients with head trama or increased intracranial pressure are particularly suscetible to insufficient or excessive fluid loading. It is therefore with care that fluids are administered and monitored. The choice of fluid is dependent on the other clinical signs of the patient such as haemodynamics. The status of the blood brain barrier is an important consideration in any patient and in the selection of fluid. However, fluids containing glucose should be avoided in these patients.