Pulpy Kidney
| This article is still under construction. |
Description
Pulpy kidney is a common, peracute and usually fatal enterotoxaemia of sheep of all ages, caused by the ε toxin of Clostridium perfringens type D. C. perfringens is a large, gram positive, anaerobic bacillus that is ubiquitous in the environment and commensalises the gastrointestinal tract of most mammals1, although type D is found less abundantly in healthy animals than the other genotypesivis. Five genotypes of Clostridium perfringens exist, named A-E, and all genotypes produce potent exotoxins. There are 12 exotoxins in total, some of which are lethal and others which are of minor significance2. These are produced as pro-toxins, and are converted to their toxic forms by digestive enzymes such as trypsin. The enterotoxaemias are a group of diseases caused by proliferation of C. perfringens in the lumen of the gastrointestinal tract and excessive production of exotoxin.
In healthy animals, there is a balance between multiplication of Clostridium perfringens and its passage in the faeces. This ensures that infection is maintained at a low level. However, C. perfringens is saccharolytic and is therefore able to multiply rapidly when large quantities of fermentable carbohydrate are introduced to the anaerobic conditions of the abomasum and small intestine, leading to build-up of exotoxin. Gut statis, for example due to insufficient dietray fibre or a high gastrointestinal parasite burden, can also contribute to the accumulation of toxins.
Enterotoxaemia due to Clostridium perfringens type D causes sudden death in sheep of any age, particularly well-grown lambs of between 4 and 10 weeks of age and fattening lambs of 6 months to 1 year oldlewis. Rams are also susceptible when they are subjected to an incraesed plane of nutrition prior to mating. The condition is associated with a change in diet, for example to include lush grass or high proportions of concentrate. This leads to rapid multiplication of the bacterium and excessive production of its ε toxin. ε toxin causes vascular damage, particularly of the capillaries in the brainmerck. The incidence of pulpy kidney declined over the past 25 years or so, due to the widespread use of clostridial vaccines3, but the condition is now becoming a problem again as complacency reduces the use of vaccination. At its most extreme, pulpy kidney can cause losses of 10-15% of the lamb crop. The disease can also occur in cattle, but this is rareivis.
ivis: perfringens type D causes enterotoxemia in small ruminants of all ages; [1,10] disease in cattle appears to be very rare [27]. Clostridium perfringens type D is not considered to be a common inhabitant of the gastrointestinal tract of normal ruminants, although it can be carried sporadically by healthy animals [10]. As for type C enterotoxemia, passage of soluble carbohydrates or protein into the small intestine is thought to induce rapid replication and elaboration of epsilon toxin from this organism [24]. Unlike beta toxin, however, epsilon toxin is activated by intestinal and pancreatic proteases [1]. Once absorbed into the bloodstream, epsilon toxin causes loss of endothelial integrity, increased capillary permeability, and edema formation in multiple tissues [28].
Type D enterotoxemia in sheep is typically a peracute illness, with many cases simply being found dead. If a live ovine case is detected, neurologic signs predominate. Lethargy and ataxia are evident early on, with collapse, hyperesthesia, lateral recumbency, convulsive paddling, and opisthotonus following within hours. Diarrhea is inconsistently seen. Glucosuria is frequently present [29].
Signalment
Pulpy kidney can affect unvaccinated sheep of all ages. However, it is most common in 4-10 week old lambs, and fattening lambs between 6 months and 1 year of age.
Diagnosis
merck A presumptive diagnosis of enterotoxemia is based on sudden, convulsive deaths in lambs on carbohydrate-rich feed. Smears of intestinal contents reveal many short, thick gram-positive rods. Confirmation requires demonstration of ɛ toxin in the small-intestinal fluid. Fluid, not ingesta, should be collected in a sterile vial within a few hours after death and sent under refrigeration to a laboratory for toxin identification. Chloroform, added at 1 drop for each 10 mL of intestinal fluid, will stabilize any toxin present. Although immunologic tests have been developed to replace the traditional mouse assay for detection of toxin, they are less sensitive than the mouse assay. A PCR protocol for detection of the gene for ɛ toxin is effective in identifying isolates as either type B or D.
- Location of the organism in the gut contents is not helpful, since it is always present (as a commensal).
- Therefore, diagnosis is by location of the toxin in the gut contents.
- Toxin is tested for by administering filtered intestinal fluid intravenously to a mouse (mouse protection test).
- If the toxin is present, the mouse should die within minutes or hours.
- Another mouse can be protected from the effect of the toxin with a specific antibody.
- An ELISA test is also possible.
- However, an ELISA is often too sensitive as the toxin can be present in the normal sheep gut and the ELISA can pick this up.
Clinical Signs
Animals are occasionally seen alive with hyperaesthesis and ataxia, which rapidly progresses to recumbency, opisthotonus, convulsions and death. In lambs which live longer, diarrhoea and signs associated with focal symmetrical encephalomalacia can be seen.
merck Usually, sudden deaths in the best-conditioned lambs are the first indication of enterotoxemia. In some cases, excitement, incoordination, and convulsions occur before death. Opisthotonos, circling, and pushing the head against fixed objects are common signs of CNS involvement; frequently, hyperglycemia or glycosuria is seen. Diarrhea may or may not develop. Occasionally, adult sheep are affected; they show weakness, incoordination, and convulsions and die within 24 hr. In goats, the course of disease ranges from peracute to chronic, with signs that vary from sudden death to watery diarrhea with or without blood. Acutely affected calves not found dead show mania, convulsions, blindness, and death in a few hours. Subacutely affected calves are stuporous for a few days and may recover. In goats, diarrhea and nervous signs are seen, and death occurs in several weeks. Type D enterotoxemia occasionally is seen in young horses that have overeaten.
lewis The disease is peracute and the majority of cases are found dead. In the rare instances that animals survive for a short time, diarrhoea is a feature, as are CNS signs due to the development of focal symmetrical encephalomalacia; typcially, there is ataxia, progressing to recumbency, opisthotonos, convulsions with or without nystagmus, and death.
Laboratory Tests
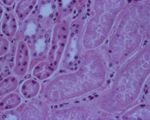
Pathology
ivis At necropsy examination, the peritoneal, pleural, and / or pericardial spaces are filled with variable volumes of straw- or red-colored fluid that may contain fibrin clots. Petechial hemorrhages are often visible on the visceral surfaces. Pulmonary and mesenteric edema may be evident. Gross lesions of the intestinal tract are frequently absent in affected sheep. Dipstick analysis of urine collected from the bladder frequently reveals the presence of glucose. The renal cortex may be softened (hence the term "pulpy kidney"), although this is a nonspecific autolytic change seen on occasion in small ruminant cadavers. The thalamus and cerebellum may be appreciably soft, with scattered hemorrhages therein. Occasionally, no gross lesions are seen in ovine cases of type D enterotoxemia [24].
merck Necropsy may reveal only a few hyperemic areas on the intestine and a fluid-filled pericardial sac. This is particularly the case in young lambs. In older animals, hemorrhagic areas on the myocardium may be found as well as petechiae and ecchymoses of the abdominal muscles and serosa of the intestine. Bilateral pulmonary edema and congestion frequently occur but usually not in young lambs. The rumen and abomasum contain an abundance of feed, and undigested feed often is found in the ileum. Edema and malacia can be detected microscopically in the basal ganglia and cerebellum of lambs. Rapid postmortem autolysis of the kidneys has led to the popular name, pulpy kidney disease; however, pulpy kidneys are by no means always found in affected young lambs and are seldom found in affected goats or cattle. Hemorrhagic or necrotic enterocolitis may be seen in goats.
- Animals are very bloated.
- Often lack lesions.
- Guts appear slightly flaccid, and a bit hyperaemic.
- The toxaemic carcase has petechial and echymotic haemorrhages, and hydropericardium.
- The kidneys are characteristically affected.
- Become oedematous, mushy and red within about 1 hour of death.
- A stream of water on cut surface of the kidney washes away the epithelium (since it is necrotic) and leaves fronds of tissue (This is the case with any kidney if the post mortem is more than a few hours after death).
- This accelerated post mortem change is a characteristic of the disease.
- Glycosuria is a feature
- The toxin affects the epithelium of the proximal part of nephron, stopping resorption of glucose.
- Note: the swelling of cells in the kidney means that anuria occurs, meaning there is no urine avaialable to rest for glucose.
- It is sometimes possible to get a positive reaction to a stick test by wiping it on the inside of the bladder.
- Periportal hepatic fatty change occurs.
- This is only really seen histologically.
- Grossly, the liver looks "half cooked", but this is true of many bacterial diseases.
- Histopathology is often not helpful.
- Necrosis of cells in proximal convoluted tubules.
- There is also a characteristic degeneration in parts of the brain - focal symmetrical encephalomalacia
- Lesions due to effect of epsilon toxin on blood vessels.
Treatment and Control
Presentation of lamb dysentery is usually peracute, with sudden deaths occuring before treatment can be implemented. Even if animals are found prior to death, treatment is usually unrewarding as organs are irreversibly damaged by toxins by the time signs present2. Instead, a definitive diagnosis should be pursued before greater losses occur, and the farmer should be encouraged to submit the carcase for further investigations.
As treatment is so ineffective, much emphasis is put on to the control of lamb dysentery. Vaccination in the face of an outbreak has been shown to be effective7, and specific hyperimmune serum can also be administered4, 6t. Oral antibiotics may be given4 but are regarded as a less appropriate therepautic. Management measures such as removing the flock from a particular pasture or reducing concentrate feeding may be implemented in other clostridial diseases but are of no benefit in lamb dysentery: over-ingestion of the dam's milk combined with poor hygiene are responsible for this disease. Therefore, sufficient supervision should be given at lambing time to ensure adequate intakes of colostrium and the maintenance of good hygiene.
Lamb dysentery can be controlled through vaccination against clostridial diseases. Before the development of modern clostridial vaccines in the 1970s, catastrophic losses of up to 30% of the lamb crop could occur due to lamb dysentery2. The vaccines used today are effective against a variety of clostridial diseases and some vaccines are combined for effects against Pasteurella. The vaccines consist of toxoids which are inactivated forms of the toxins produced by clostridial organisms. The principles of vaccination are the same whether a clostridium-only or Pasteurella-combined product is used: a sensitising dose must be given 4-6 weeks before a second, confirming dose2. As immunity wanes over a period of a year booster doses are required annually. Therefore, ewes should receive the primary vaccination course before entering the breeding flock and an annual booster approximately six weeks before lambing. Timing the booster vaccination in this way affords passive protection to lambs until they are around sixteen weeks of age. Lambs born to unvaccinated ewes should be vaccinated between 3 and 12 weeks old, with a second injection given at least four weeks later.
Links
- The Merck Veterinary Manual: Pulpy Kidney
- The Center for Food Security and Public Health Animal Disease Factsheet: Epsilon toxin of Clostridium perfringens.
- NOAH: Vaccination of farm animals
- Clostridia.net - Clostridium perfringens