Difference between revisions of "Hepatic Lipidosis"
JamesSwann (talk | contribs) |
|||
| Line 8: | Line 8: | ||
| '''Hyperlipaemia''' in [[Hyperlipaemia - Horse|'''horses''']] and [[Hyperlipaemia - Donkey|'''donkeys''']]<br> | | '''Hyperlipaemia''' in [[Hyperlipaemia - Horse|'''horses''']] and [[Hyperlipaemia - Donkey|'''donkeys''']]<br> | ||
'''[[Fatty Liver Syndrome]]''' in '''cattle'''<br> | '''[[Fatty Liver Syndrome]]''' in '''cattle'''<br> | ||
| − | '''[[White Liver Disease - | + | '''[[White Liver Disease - Sheep|White liver disease]]''' and '''[[Pregnancy Toxaemia|pregnancy toxaemia]]''' in '''sheep''' |
|} | |} | ||
Revision as of 22:28, 26 July 2010
| This article is still under construction. |
| Also known as: | Lipid Mobilisation Syndrome |
| See also: | Hyperlipaemia in horses and donkeys Fatty Liver Syndrome in cattle |
Description
Hepatic lipidosis describes a syndrome caused by derangements in lipid and protein metabolism. It occurs in both cats and dogs but it is more clinically significant in cats. Similar phenomena occur in horses, donkeys, cattle and sheep when they are exposed to periods of metabolic stress. Hepatic lipidosis may be primary (or idiopathic) or it may be secondary to another disease.
Primary Lipidosis
Primary or idiopathic hepatic lipidosis is most commonly recognised in obese indoor cats following a period of anorexia. It is the most common hepatic disease of cats in North America but it is becoming more common in Europe. It occurs due to the accumulation of large amounts of lipid in hepatocytes, producing an acute hepatopathy. The mortality rate of this disease is high unless it is treated aggressively.
The pathogenesis involves a number of factors:
- Excessive lipid mobilisation induced by anorexia, starvation, illness or stress.
- Deficiency of dietary proteins and other nutrients, which reduces the capacity of the liver to produce lipid transport proteins and to metabolise fat. Recognised micronutrient deficiencies include arginine, carnitine, taurine and methionine.
- Disturbances in the neurohormonal control of appetite resulting in inappropriate anorexia.
Secondary Lipidosis
Secondary hepatic lipidosis is a neuroendocrine response in dogs and cats to other diseases, including pancreatitis, diabetes mellitus, inflammatory bowel disease and primary hypertriglyceridaemia. Secondary hepatic lipidosis is therefore less closely associated with obesity and it may be seen in normal or even thin cats.
Signalment
Indoor and obese cats are more prone to the development of primary hepatic lipidosis during periods of stress or anorexia.
Diagnosis
Clinical Signs
- Often obese cats following a sudden starvation
- Anorexia and lethargy
- Jaundice
- Hepatic Encephalopathy
- Diarrhoea (sometimes)
- Palpable hepatomegaly (sometimes)
- Coagulopathies (sometimes)
Laboratory Tests
Biochemistry
- Markedly increased level in alanine
- Low gamma-glutamyltransferase (GGT) concentration
Diagnostic Imaging
Radiography
Abdominal radiography shows a marked hepatomegaly.
Ultrasonography
On ultrasound, an enlarged and diffusely hyperechoeic liver is seen.
Pathology
- enlarged liver with round edges
- lightish yellow in colour
- cut surface is uniform and greasy to handle
Histopathology
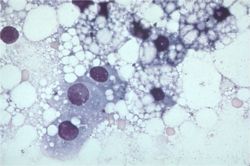
Fine needle aspirate of the liver is normally sufficient for a diagnosis. Cytology demonstrates hepatocytes swollen with lipid. Biopsy and culture of the liver tissue is always indicated to determine the underlying cause of the disease.
Treatment
- Intensive treatment of cats is required for best outcome
Nutritional support
- For a period of 4 - 6 weeks.
- This is the most important treatment in hepatic lipidosis. It is vital to ensure that the diet is of adequate calorific content with an increase in protein content. Specific nutrients such as arginine, taurine, or carnitine may also be added.
- This can be done via different feeding systems such as naso-oesophageal tube, oesophagostomy tube, gastrostomy tube.
Hepatic Encephalopathy
- Treat this if presented.
Gastrointestinal drugs
- Anti-emetics and porkinetics such as ranitidine and metoclopromide if vomiting for delayed gastric emptying is present
Fluid therapy
- Intravenous fluid therapy in early stages of disease.
- Blood glucose and electrolytes especially potasium and phosphate should be monitored.
Coagulopathy
- Vitamin K supplement may be required if coagulopathy is significant.
Prognosis
This is dependent on the underlying cause. If treated appropriately, 85% of severely affected animals will recover.
References
- Ettinger, S.J. and Feldman, E. C. (2000) Textbook of Veterinary Internal Medicine Diseases of the Dog and Cat Volume 2 (Fifth Edition) W.B. Saunders Company.
- Hall, E.J, Simpson, J.W. and Williams, D.A. (2005) BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition) BSAVA
- Nelson, R.W. and Couto, C.G. (2009) Small Animal Internal Medicine (Fourth Edition) Mosby Elsevier.
- Tilley, L. P. & Smith, F. W. K. (2007) Blackwell's Five-minute Veterinary Consult: Canine & Feline (Fourth Edition) Blackwell Publishing
From Pathology
Hepatic lipidosis - fatty liver syndrome
- associated with
- dietary factors: obesity and starvation
- increased demand for energy: pregnancy, lactation, and starvation in physiological states
- Diabetes mellitus, ketosis, and pregnancy toxaemia in pathological conditions
- abnormal hepatocytic function: prevents fatty acids from forming complexes with proteins to form low density lipoproteins for secretion into the blood
The following are several important specific diseases in which fatty change is the main finding:
Feline
- diagnosis on cytology/histopathology
- Survival rate is only 50-60%
- Pathophysiology:
- Incompletely understood
- Obese cats that lose 30-40% of body weight exhibit a similar syndrome to naturally occurring hepatic lipidosis
- But many causative factors for naturally occurring hepatic lipidosis:
- Peripheral lipolysis secondary to absolute or relative lack of insulin
- Protein-calories malnutrition
- Amino acid deficiencies – inability to synthesize apolipoproteins necessary to mobilize hepatic fat
- Deficiency of lipotrophic compounds
- Error of fatty acid oxidation
- Hepatic perioxosomal damage due to oxidative stress
- Cats with hepatic lipidosis have higher nonesterified fatty acids (NEFAs) compared to controls and those with cholangiohepatitis
- NEFAs are derived from lipolysis of fat stores and enter the liver
- They are oxidized in the liver for energy or converted to phospholipids or cholesterol or reesterified to triglycerides
- Limited increase in lipoprotein synthesis and secretion of triglycerides in VLDLs
- Capacity for increase in oxidation by mitochondria and ketone body synthesis is low
- Rate of fatty acid esterification to triglycerides is not limited so can lead to a marked increase in the accumulation of stored hepatic triglycerides
- Also all triglyceride accumulation in hepatocytes in these cats comes from mobilized peripheral adipose stores during nutritional stress
- high levels of triglyceride concentrations in the liver will cause:
- severe periacinar necrosis
- jaundice
- hepatic encephalopathy
- high mortality rate
- high levels of triglyceride concentrations in the liver will cause:
- Lipolysis – under control of hormone-sensitive lipase hydrolyses triglycerides to NEFAs and glycerol
- Insulin – inhibits it
- Catecholamines (eg: released in stress, etc – neural input), glucocorticoids, thyroxine, GH and glucagons all promote lipolysis
- Lower insulin levels in cats with hepatic lipidosis or cholangiohepatitis compared to controls; and lower glucogon:insulin ratio in diseased cats
- But as not lipidosis specific, not likely to be the main factor involved
- Higher serum triglycerides in lipidotic cats compared to controls
associated with derangement of carbohydrate metabolism
Diabetes Mellitus
Ketosis
associated with anoxia and toxaemia
anoxia
- passive congestion
- anaemias
toxaemia
- toxins absorbed from the gut interfere with many stages of triglyceride metabolism