| Cerebrum, basal nuclei, cerebellum:
|
*Abnormal menace response
- Circling
- Seizures (may be the only clinical sign)(82 in Furr)
- Abnormal electroencephalogram (EEG)
- Asymmetrical central blindness
- Facial hypoalgesia
- Cerebellar ataxia
- Altered behavior
- Depression
- Narcolepsy-like syndrome
Lesions of the brainstem, cerebrum or cerebellum are less frequently recognized than those of the spinal cord. Horse with severe EPM may be unable to stand or swallow and, if left untreated, progress to recumbency within 14 days to 6 months. (Pasq) This deterioration may occur smoothly or spasmodically (Merck) but is likely to result in death. It has been suggested that rapidly progressive presentations reflect brainstem lesions.(Furr)
Diagnosis
Differential Diagnoses
The protozoan can migrate to any region of the CNS[2], thus the differential list comprises almost all diseases of this system.
| Differential
|
Differentiating signs
|
Tests to rule out
|
| Cervical vertebral malformation (CVM, cervical compressive myelopathy, cervical vertebral instability, cervical stenotic myelopathy, cervical spondylomyelopathy, Wobbler's syndrome).
|
Symmetrical gait deficits, worse in pelvic limbs[19] with spasticity and dysmetria, good retention of strength, no muscle wasting.[4] NB:can be concurrent with EPM.[20]
|
Plain lateral radiography of C1 to T1[20], myelography. [21]
|
| West Nile encephalitis
|
Systemically ill, pyrexia. Difficult to differentiate if horse is afebrile and has no excessive muscle fasciculations.[22]
|
Leukogram, CSF analysis, IgM capture ELISA, plaque reduction neutralization test (PRNT).[21]
|
| WEE
|
Systemically ill, pyrexia, abnormal motor function.[22]
|
Leukogram, ELISA, titres, virus isolation.[21]
|
| EEE
|
Systemically ill, pyrexia, abnormal motor function[22], rapidly progressive.[21]
|
Leukogram, CSF analysis, ELISA, titres, virus isolation.[21]
|
| VEE
|
Systemically ill, pyrexia.
|
Leukogram, IgM ELISA[23]
|
| Equine herpesvirus-1 myeloencephalopathy
|
Sudden onset and early stabilization of neurological signs, multiple horses affected, recent fever, abortion.[24] Dysuria not often seen in EPM.[4]
|
CSF analysis, PCR[4], titres, virus isolation.[21]
|
| Rabies
|
Rapid progression[25], behavioural alterations, depression, seizure, coma.[22]
|
Post-mortem fluorescent antibody testing of brain required for definitive diagnosis.[25]
|
| Polyneuritis equi (previously cauda equina neuritis)
|
Cranial nerve deficits are peripheral with no change in attitude.[26]
|
Western blot analysis of CSF.[27]
|
| Equine degenerative myeloencephalopathy
|
Symmetrical signs.[28]
|
May get increased CSF creatinine kinase (CK)[29] and reduced serum Vitamin E concentrations but these are unreliable for ante mortem diagnosis.[28]
|
| Verminous encephalomyelitis
|
Acute onset.
|
CSF analysis.[30]
|
| Bacterial meningoencephalitis
|
Stiff neck.[1]
|
|
| CNS abscessation due to 'bastard strangles'[4]
|
History of Streptococcus equi subsp. equi infection.[31]
|
CSF analysis (severe, suppurative inflammation), culture of CSF.[31]
|
| Spinal trauma[1]
|
History (usually acute onset neurological signs), usually solitary lesion localised by neurological exam.[32]
|
Radiography, myelography, CT, MRI, nuclear scintigraphy, ultrasound, CSF analysis, nerve conduction velocities, EMG, transcranial magnetic stimulation.[33]
|
| Occipito-atlanto-axial malformation (OAAM)
|
Deficits develop before 6mths in Arabian horse.[34]
|
Radiography.[21]
|
| Spinal tumor
|
Signs can usually be localized to one region of the CNS.
|
CT, MRI. Definitive diagnosis requires cytology, biopsy, histopathology or CSF analysis.[35]
|
| Sorghum cystitis/ataxia[1]
|
Posterior ataxia or paresis, cystitis, history of grazing Sorghum species[36]
|
Demonstration of cystitis or pyelonephritis by laboratory methods, but not specific.[37]
|
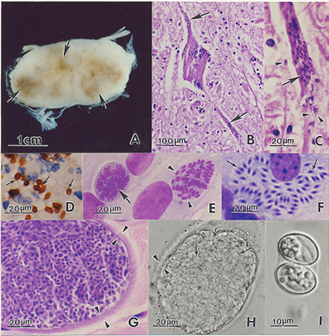
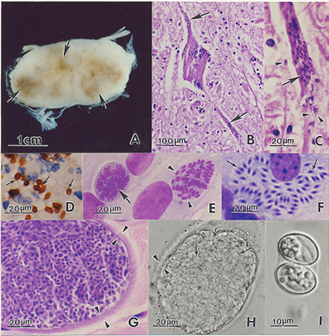 Sarcocystis neurona stages and lesions. (A). Cross section of spinal cord of horse with focal areas of discoloration (arrows) indicative of necrosis. Unstained. (B). Section of spinal cord of a horse with severe EPM. Necrosis, and a heavily infected neuron (arrows), all dots (arrows) are merozoites. H and E stain . (C). Higher magnification of a dendrite with numerous merozoites (arrows). One extracellular merozoite (arrowhead) and a young schizont (double arrowhead). (D). Section of brain of an experimentally-infected mouse stained with anti-S. neurona antibodies. Note numerous merozoites (arrows). (E). Immature schizonts in cell culture. A schizont with multilobed nucleus (arrow) and a schizont with differentiating merozoites (arrowheads). Giemsa stain. (F). Mature sarcocysts with hairlike villar protrusions (double arrowheads) on the sarcocyst wall. H and E stain. (G). Mature live sarcocyst with numerous septa (arrows) and hairlike protrusions on the sarcocyst wall (double arrowheads). Unstained. (H). An oocyst with two sporocysts each with banana-shaped sporozoites. Unstained. Created by the Agricultural Research Service, the research agency of the United States Department of Agriculture, July 2005. Sourced from the USDA Agricultural Research Service page on EPM/Sarcocystis neurona, located via WikiMedia Commons. Pathology
Widespread lesions of the CNS are typically observed in horses.[4]
Gross exam
Lesions may be up to several centimetres across.[4] They range from mild discolouration to multifocal areas of haemorrhage and/or malacia[38] of the brain, spinal cord and less commonly, peripheral nerves.[4]
Histopathology
Microscopically, both grey and white matter may be affected with focal to diffuse areas of nonsuppurative inflammation, necrosis and neuronal destruction. Perivascular infiltrates comprise lymphocytes, macrophages, plasma cells, giant cells, eosinophils and gitter cells.[4] In around 25% of cases, schizonts or merozoites may be found in the neuronal cytoplasm.[38] Less frequently, protozoa parasitize intravascular and tissue neutrophils and eosinophils, capillary endothelial cells and myelinated axons[4][38]. Free merozoites may be seen in necrotic regions. If organisms are absent, the diagnosis relies on recognition of the inflammatory changes described above.[38]
Treatment
Prognosis
Depends on duration and severity of neurological signs[3] but clinical resolution is more likely if the condition is diagnosed and treated early.[2] With standard therapy, involving 6-8months of ponazuzril or pyrimethamine-sulfadiazine (V), there is a recovery rate of around 25% and an improvement in 60-75% of cases.[39] A good prognosis might be expected if there is an improvement in clinical signs within two weeks of commencing anti-protozoal and anti-inflammatory treatment (V). The prognosis will be guarded to poor[1] for a horse with severe irreversible neuronal damage or one that has not been diagnosed or treated appropriately (V).
Prevention
Prophylaxis
A killed vaccine, developed using S.neurona merozoites, was conditionally licensed for use in horses.[40] The vaccine proved to be ineffective in the prevention of EPM and has since been removed from the market.[4] There is evidence to suggest that the antiprotozoal, ponazuril, may be useful prophylactically to reduce the incidence and severity of clinical signs.[41] Implementing such a regime prior to and during stressful events may be beneficial, although the cost is likely to be prohibitive.[4]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Pasquini, C, Pasquini, S, Woods, P (2005) Guide to Equine Clinics Volume 1: Equine Medicine (Third edition), SUDZ Publishing, 245-250. Cite error: Invalid
<ref> tag; name "Pasq" defined multiple times with different content Cite error: Invalid <ref> tag; name "Pasq" defined multiple times with different content Cite error: Invalid <ref> tag; name "Pasq" defined multiple times with different content Cite error: Invalid <ref> tag; name "Pasq" defined multiple times with different content Cite error: Invalid <ref> tag; name "Pasq" defined multiple times with different content Cite error: Invalid <ref> tag; name "Pasq" defined multiple times with different content Cite error: Invalid <ref> tag; name "Pasq" defined multiple times with different content Cite error: Invalid <ref> tag; name "Pasq" defined multiple times with different content
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Gray, L.C, Magdesian, K.G, Sturges, B.K, Madigan, J.E (2001) Suspected protozoal myeloencephalitis in a two-month-old colt. Vet Rec, 149:269-273. Cite error: Invalid
<ref> tag; name "EPM8" defined multiple times with different content
- ↑ 3.0 3.1 Vatistas, N, Mayhew, J (1995) Differential diagnosis of polyneuritis equi. In Practice, Jan, 26-29.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ DEFRA, The Animal Health Trust, The British Equine Veterinary Association (2009) Surveillance: Equine disease surveillance, April to June 2009, The Vet Rec, Oct 24:489-492.
- ↑ Dubey, J.P, Lindsay, D.S, Saville, W.J, Reed, S.M, Granstrom, D.E, Speer, C.A (2001)A review of Sarcocystis neurona and equine protozoal myeloencephalitis (EPM). Vet Parasitol, 95:89-131. In: Pusterla, N, Wilson, W.D, Conrad, P.A, Barr, B.C, Ferraro, G.L, Daft, B.M, Leutenegger, C.M (2006) Cytokine gene signatures in neural tissue of horses with equine protozoal myeloencephalitis or equine herpes type 1 myeloencephalopathy. Vet Rec, Sep 9:Papers & Articles.
- ↑ Wobeser, B.K, Godson, D.L, Rejmanek, D, Dowling, P (2009) Equine protozoal myeloencephalitis caused by Neospora hughesi in an adult horse in Saskatchewan. Can Vet J, 50(8):851-3.
- ↑ Reed, S.M, Granstrom, D, Rivas, L.J, Saville, W.A, Moore, B.R, Mitten, L.A (1994) Results of cerebrospinal fluid analysis in 119 horses testing positive to the Western blot test on both serum and CSF to equine protozoal encephalomyelitis. In Proc Am Assoc Equine Pract, Vancouver BC, AEEP, Lexington, KY, p199. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Pitel, P.H, Pronost, S, Gargala, G, Anrioud, D, Toquet, M-P, Foucher, N, Collobert-Laugier, C, Fortier, G, Ballet, J-J (2002) Detection of Sarcocystis neurona antibodies in French horses with neurological signs, Int J Parasitol, 32:481-485. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Goehring, L.S (2001) Sloet van Oldruitenborgh-Oosterbaan MM: Equine protozoal myeloencephalitis in the Netherlands? An overview, Tijdschr Diergeneeskd, 126:346-351. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Saville, W.J.A, Reed, S.M, Granstrom, D.E, Morley, P.S (1997) Some epidemiologic aspects of equine protozoal
myeloencephalitis. Proceedings of the Annual Convention of the AAEP, 43:6-7.
- ↑ NAHMS (2000): Equine protozoal myeloencephalitis in the US, Ft Collins, CO, USDA:APHIS:VS, CEAH, National Animal Health Monitoring System. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ MacKay, R.J, Davis, S.W, Dubey, J.P (1992) Equine protozoal myeloencephalitis, Compend Contin Educ Pract Vet, 14:1359-1367. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Fayer, R, Mayhew, I.G, Baird, J.D, Dill, S.G, Foreman, J.H, Fox, J.C, Higgins, R.J Higgins, Reed, S.M, Ruoff, W.W, Sweeney, R.W, Tuttle, P (1990) Epidemiology of equine protozoal myeloencephalitis in North America based on histologically confirmed cases, J Vet Intern Med, 4:54-57. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Boy, M.G, Galligan, D.T, Divers, T.J (1990) Protozoal encephalomyelitis in horses: 82 cases (1972-1986), J Am Vet Med Assoc, 196:632-634. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Saville, W.J, Reed, S.M, Morley, P.S, Granstrom, D.E, Kohn, C.W, Hinchcliff, K.W, Wittum, T.E (2000) Analysis of risk factors for the development of equine protozoal myeloencephalitis in horses. J Am Vet Med Assoc, 217:1174-1180. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Saville, W.J.A, Reed, S.M, Morley, P.S (1999) Examination of risk factors for equine protozoal
myeloencephalitis. Proceedings of the Annual Convention of the AAEP, 45:48-49.
- ↑ Tillotson, K, McCue, P.M, Granstrom, D.E, Dargatz, D.A, Smith, M.O, Traub-Dargatz, J.L (1999) Seroprevalence of antibodies to Sarcocystis neurona in horses residing in northern Colorado, J Equine Vet Sci, 19:122-126. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Mayhew, I.G, deLahunta, A, Whitlock, R.H, Krook, L, Tasker, J.B (1978) Spinal cord disease in the horse, Cornell Vet, 68(Suppl 8):110-120. In: Hahn, C.N (2010) Cervical Vertebral Malformation in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 20.0 20.1 Hahn, C.N (2010) Cervical Vertebral Malformation in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 Seino, K.K (2010) Spinal Ataxia in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 3.
- ↑ 22.0 22.1 22.2 22.3 Long, M.T (2010) Flavivirus Encephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Bertone, J.J (2010) Viral Encephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Wilson, W.D, Pusterla, N (2010) Equine Herpesvirus-1 Myeloencephalopathy in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 25.0 25.1 Sommardahl, C.S (2010) Rabies in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Scaratt, W.K, Jortner, B.S (1985) Neuritis of the cauda equina in a yearling filly. Compend Contin Educ Pract Vet, 7:S197-S202. In: Saville, W.J (2010) Polyneuritis equi in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Granstrom, D.E, Dubey, J.P, Giles, R.C (1994) Equine protozoal myeloencephalitis: biology and epidemiology. In Nakajima, H, Plowright, W, editors: Refereed Proceedings, Newmarket, England, R & W Publications. In: Saville, W.J (2010) Polyneuritis equi in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 28.0 28.1 Nout, Y.S (2010) Equine Degenerative Myeloencephalopathy in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Mayhew, I.G, deLahunta, A, Whitlock, R.H, Krook, L, Tasker, J.B (1978) Spinal cord disease in the horse, Cornell Vet, 68(Suppl 8):1-207. In: Nout, Y.S (2010) Equine Degenerative Myeloencephalopathy in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Jose-Cunilleras, E (2010) Verminous Encephalomyelitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 31.0 31.1 Byrne, B. A (2010) Diseases of the Cerebellum in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Smith, P.M, Jeffery, N.D (2005) Spinal shock - comparative aspects and clinical relevance. J Vet Intern Med, 19:788-793. In: Nout, Y.S (2010) Central Nervous System Trauma in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Nout, Y.S (2010) Central Nervous System Trauma in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Watson, A.G, Mayhew, I.G (1986) Familial congenital occipitoatlantoaxial malformation (OAAM) in the Arabian horse. Spine, 11:334-339. In: Seino, K.K (2010) Spinal Ataxia in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 3.
- ↑ Sellon, D.C (2010) Miscellaneous Neurologic Disorders in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Talcott, P (2010) Toxicoses causing signs relating to the urinary system in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 22.
- ↑ Talcott, P (2010) Toxicoses causing signs relating to the urinary system in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 22.
- ↑ 38.0 38.1 38.2 38.3 Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial
- ↑ MacKay, R.J (2006) Equine protozoa myeloencephalitis: treatment, prognosis and prevention. Clin Tech Equine Pract, 5:9-16. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Saville, W.J.A, Reed, S.M, Dubey, J.P (2002) Prevention of equine protozoal myeloencephalitis
(EPM). Proceedings of the Annual Convention of the AAEP, 48:181-185.
- ↑ Furr, M, MacKenzie, H, Dubey, J.P (2006) Pretreatment of horses with ponazuril limits infection and neurologic signs resulting from S.neurona. J Parasitol, 92:637-643. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
|