Dirofilaria immitis
| This article is still under construction. |
Description
Heartworm (HW) infection is caused by a filarial organism, Dirofilaria immitis . At least 70 species of mosquitos can serve as intermediate hosts; Aedes , Anopheles , and Culex are the most common genera acting as vectors. Patent infections are possible in numerous wild and companion animal species. Wild animal reservoirs include wolves, coyotes, foxes, California gray seals, sea lions, and raccoons. In companion animals, HW infection is seen primarily in dogs and less commonly in cats and ferrets. HW disease has been reported in most countries with temperate, semitropical, or tropical climates, including the USA, Canada, and southern Europe. In companion animals, infection risk is greatest in dogs and cats housed outdoors. Although any dog, indoor or outdoor, is capable of being infected, most infections are diagnosed in medium- to large-sized, 3- to 8-yr-old dogs. Infected mosquitos are capable of transmitting HW infections to humans, but there are no reports of such infections becoming patent. Maturation of the infective larvae may progress to the point where they reach the lungs, become encapsulated, and die. The dead larvae precipitate granulomatous reactions called “coin lesions,” which are medically significant because radiographically they appear similar to metastatic lung cancer. HW infection rates in other companion animals such as ferrets and cats tend to parallel those in dogs in the same geographic region, but usually at a lower prevalence. No age predilection has been reported in ferrets or cats, but male cats have been reported to be more susceptible than females. Indoor and outdoor ferrets and cats can be infected. Other infections in cats, such as those caused by the feline leukemia virus or feline immunodeficiency virus, are not predisposing factors.
Life Cycle
Mosquito vector species acquire the first stage larvae (microfilariae) while feeding on an infected host. Development of microfilariae to the second larval stage (L2) and to the infective third stage (L3) occurs within the mosquito in ~1-4 wk, depending on environmental temperatures. This development phase requires the shortest time when the ambient temperature is >86°F (30°C). When mature, the infective larvae migrate to the labium of the mosquito. As the mosquito feeds, the infective larvae erupt through the tip of the labium with a small amount of hemolymph onto the host’s skin. The larvae migrate into the bite wound, beginning the mammalian portion of their life cycle. A typical Aedes mosquito is only capable of surviving the developmental phase of small numbers of HW larvae, usually <10 larvae per mosquito. In canids and other susceptible hosts, infective larvae (L3) molt into a fourth stage (L4) in 2-3 days. After remaining in the subcutaneous tissue for close to 2 mo, they molt into young adults (L5) that migrate through host tissue, arriving in the pulmonary arteries ~50 days later. Adult worms (males ~15 cm in length, females ~25 cm) develop primarily in the pulmonary arteries of the caudal lung lobes over the next 2-3 mo. They reside primarily in the pulmonary arteries but can move into the right ventricle when the worm burden is high. Microfilariae are produced by gravid females ~6-7 mo postinfection. Microfilariae are usually detectable in infected canids not receiving macrolide prophylaxis. However, 25% to >50% of infected canids may not have circulating microfilariae. Thus, the number of circulating microfilariae does not necessarily correlate strongly to adult female HW burden. Adults typically live 3-5 yr, while microfilariae may survive for 1-2 yr while awaiting a mosquito intermediate host. Most dogs are highly susceptible to HW infection, and the majority of infective larvae (L3) develop into adults. Ferrets are susceptible hosts, and cats are somewhat resistant. A lower percentage of exposed cats develop adult infections and the burden is often only 1-3 worms. Further evidence of relative resistance in cats is the short survival time of many L5 in the pulmonary arteries; adult worms probably survive no longer than 2 yr. Aberrant migration into different organs, including the CNS, has been described in cats.
Pathogenesis
Signalment
Diagnosis
Diagnosis:
- Physical examination:
- signs of heart disease
- lung involvement
- Radiography:
- enlargement of right heart, main pulmonary arteries; arteries in lung lobes with thickening and tortuosity; inflammation in surrounding tissues
- ECG:
- right axis deviation → deep S waves
- Echocardiography:
- if post caval syndrome suspected - right ventricular enlargement with worms in ventricle appearing as parallel lines.
Clinical pathology:
- needed alongside physical examination and other tests to determine treatment strategy and prognosis.
Parasite detection:
- methods for demonstrating microfilariae in blood:
- wet blood smear (okay for quick look, but insensitive) = D. immitis not progressively motile
- Knott's test = red blood cells lysed; stained sediment examined
- micropore filter = blood forced through; microfilariae held on filter; stained and examined
- antibody detection ELISA = not reliable in dogs, but it is the best for cats (although some false positives)
- antigen detection ELISA (using specific antigen from adult female worm) = reliable positives from 5-7months post-infection in dogs; although occasional false negatives occur → not useful for cats
- the immunochromatographic test (ICT) uses coloured gold colloidal particles tagged to monoclonal antibodies to visualise the presence of adult worm antigen - performance similar to antigen detection ELISA, but quicker and easier to do (but not as quantitative as some ELISAs are)
- operator error can give false positives, therefore best to confirm result with another test.
Clinical Signs
Clinical signs:
- often sudden onset severe lethargy and weakness, but:
- signs variable, reflecting multiple system dysfunction - pulmonary circulation, heart, liver and kidneys:
- lung damage (severe pulmonary hypertension; thromboembolism)
- heart failure (right-sided congestive)
- therefore, not pathognomonic
- acute prepatent = coughing
- chronic = exercise intolerance, sometimes with ascites
- acute post caval syndrome = collapse (dyspnoea, pale mucous membranes or jaundice, haemoglobinuria)
Diagnostic Imaging
Laboratory Tests
Pathology
Worms produce:
- substances that are:
- antigenic
- immunomodulatory
- pharmacologically active.
Lesions are:
- not confined to the location of the worms
- also caused by shear stress of high blood flow.
Severity:
- not associated with the number of worms
- exacerbated by exercise (i.e. by high blood flow rate)
- sedentary dogs often asymptomatic - symptoms most commonly associated with racing greyhounds.
Acute prepatent disease:
- immature adult worms in caudal distal pulmonary arteries
- leads to intense diffuse eosinophilic reaction, which in turn leads to coughing.
Chronic disease:
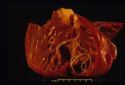
- mature worms in right heart and pulmonary arteries
- endothelial swelling and sloughing
- increased permeability → inflammation → periarteritis
- platelets/white blood cells activated → thrombosis
- proliferation of smooth muscle, thickening of media:
→ impairment of blood flow
→ pulmonary hypertension
→ right ventricular strain
→ right ventricular hypertrophy and right-sided heart failure
- insufficient blood pumped through pulmonary capillary bed → insufficient preload for left ventricle.
Post Caval Syndrome (Dirofilarial haemoglobinuria):
- can be acute or chronic
- heavy heartworm infestation:
- entangled clumps of worms → impaired closure of tricuspid valve → post-caval stagnation → hepatic congestion and hepatic failure
- this is accompanied by increased red blood cell fragility, haemolytic anaemia and haemolobinuria.
Treatment
Chemotherapy:
- three treatment objectives needing different approaches:
1) Adulticidal
- risk that dead worms → thromboembolism → respiratory failure
- therefore, hospitalise and strict exercise restriction for at least 3weeks post-treatment
- organic arsenicals for adulticidal therapy:
- Thiacetarsamide (2.2mg/kg IV bid for 2days) - hepatotoxic; skin sloughing
- Melarsomine (2.5mg/kg IM sid for 2days) - generally safer, but greater risk of thromboembolism
NB - Ivermectin preventative doses over 16months reduces adult worm numbers
2) Microfilaricidal
- start 3-6weeks after adulticidal therapy:
- Ivermectin (50µg/kg)
- Milbemycin oxime (0.5mg/kg)
NB - risk of reaction to dead microfilariae in sensitised animals (lethargy, retching, tachycardia, circulatory collapse) - observe for 8hours post-treatment
3) Preventative (prophylactic)
- objective = kill migrating L4 before they reach the heart
- monthly treatments are 100% effective and safe if used properly, but often fail because of inadequate owner compliance
- test for adult infection/microfilarie before start and annually thereafter:
- Ivermectin (6µg/kg monthly) - blocks maturation of larvae; these die only after several months
- Selamectin (6mg/kg monthly)
- Moxidectin (injectable formulation - 0.17mg/kg gives 6months protection)
- Milbemycin oxime (0.5mg/kg monthly) - care → kills microfilarie, therefore risk of reaction
- DEC (diethylcarbamazine) daily - care → kills microfilarie, therefore severe risk of reaction
Treatment of Post Caval Syndrome:
- surgical removal with forceps via jugular vein
- usually very successful, but:
- do not crush or fragment worms
→ massive release of antigen
→ cardiac failure and acute respiratory distress
→ rapid death
A typical therapy protocol:
1) Pre-treatment evaluation
2) Adulticide: 4-6weeks restricted exercise
3) Microfilaricide: 3weeks after adulticide
4) Initiation of monthly preventative treatments
5) Check for microfilariae after 2weeks
6) Check for adults (ELISA) 4-6months after adulticide, and before start of each subsequent mosquito season.