Small Animal Emergency and Critical Care Medicine: Self-Assessment Color Review, Second Edition, Q&A 12
Jump to navigation
Jump to search

| This question was provided by CRC Press. See more case-based flashcards |

|
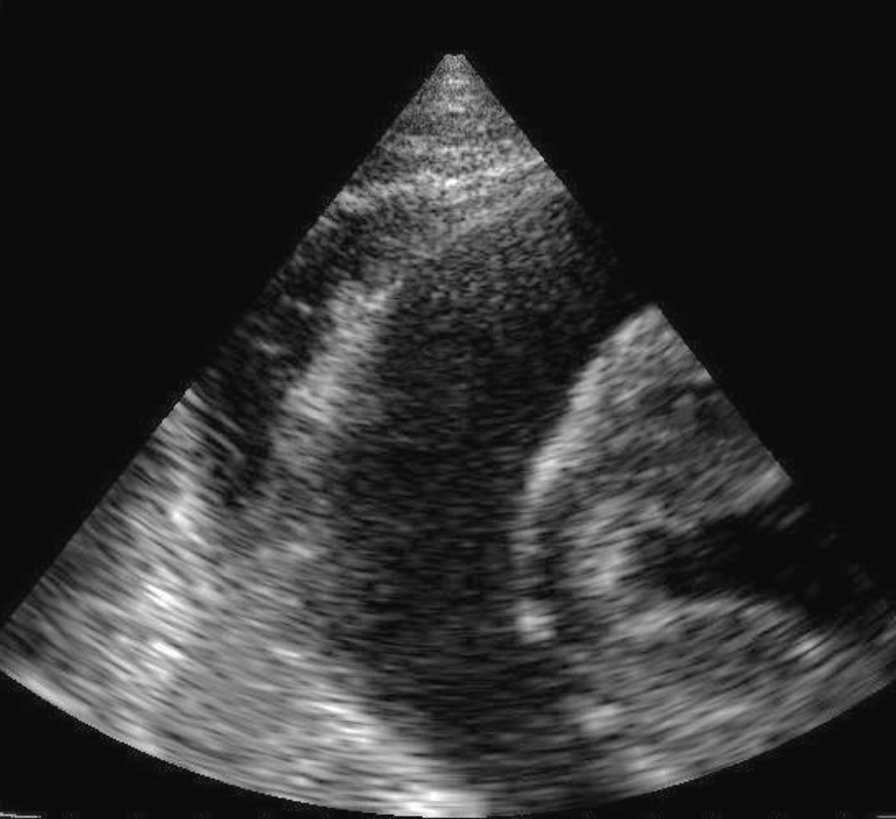
Student tip: This case is describing pericardiocentesis using an excellent ultrasound image |
A 12-year-old female neutered Golden Retriever presents for vomiting digested food and clear fluid. The dog is unable to stand. T = 37.5°C (99.6°F); HR = 170 bpm with muffled heart sounds; RR = 24 bpm; CRT = 3 sec; MM pale; jugular vein distension; poor femoral pulse quality. Radiographs demonstrate a mild increase in interstitial pattern in the lungs compatible with age and a globoid enlarged cardiac silhouette. An ultrasound image from the ventral 4th rib space is shown (12a).
| Question | Answer | Article | |
| What is the most likely cause of the clinical signs in this dog? | Cardiac tamponade. (Decreased ventricular preload from accumulation of pericardial fluid.)
|
Link to Article | |
| What procedure would you perform, and how would you do it? | Pericardiocentesis. Clip and aseptically prepare skin on the right thoracic wall, from 2nd to 6th rib space, mid chest to ventral midline. The right side is chosen to decrease the risk of lung puncture/laceration (‘cardiac notch’ between right cranial and middle lung lobes) and decrease risk of coronary artery laceration. Administer a local anesthetic in skin, subcutaneous tissue, muscle at site of needle insertion. Monitor ECG for evidence of arrhythmias. Insert a 14–18 gauge 2 inch catheter or needle perpendicular to the thoracic wall in the 3rd or 4th rib space on the cranial aspect of the rib. Advance 1–3 mm after fluid is noted in the hub, attach a 3-way stop-cock and extension set, and aspirate the fluid. The needle/catheter is removed if the heart can be felt touching the catheter and/or an arrhythmia occurs. Observation and guidance by ultrasound is ideal.
|
Link to Article | |
| List differential diagnoses. | Ruptured neoplasm or cardiac chamber (left atrium), coagulopathy, neoplastic effusions, idiopathic pericardial effusion, right heart failure, pyopericardium (less likely).
|
Link to Article | |
| After successful completion of the procedure, the dog is bright, alert, and responsive. HR | Accelerated (idio)ventricular rhythm. The QRS complex is wide and bizarre, indicating a ventricular-origin beat (rate is 1,500/13 |
Link to Article | |
| Give indications for intervention if you see this rhythm. | Intervention is indicated if there is evidence of poor cardiac output, collapse, or ‘malignant’-appearing rhythms such as multiform/multifocal ventricular rhythms, R-on-T phenomenon (no return to baseline), or ventricular tachycardia (typically if >160–180 bpm). With a ventricular rate of 100–140 there is often adequate cardiac output.
|
[[ Replace text with name and subsection of relevant WikiVet page if in existence eg. Feather - Anatomy & Physiology#Structure & Function |Link to Article]] | |
To purchase the full text with your 20% off discount, go to the CRC Press Veterinary website and use code VET18.