Sexual Differentiation - Anatomy & Physiology
Jump to navigation
Jump to search
BACK TO REPRODUCTIVE SYSTEM
BACK TO FERTILISATION , IMPLANTATION and EARLY EMBRYONIC DEVELOPMENT
BACK TO REPRODUCTIVE SYSTEM
BACK TO FERTILISATION , IMPLANTATION and EARLY EMBRYONIC DEVELOPMENT
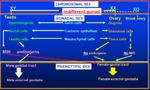
Genetic Sex
- Established at the time of fertilisation.
- The foetus receives its genetic endowment in two equal portions from the male gamete (Spermatozoon) and female gamete (Oocyte).
- The X sex chromosome is larger than the Y sex chromosome.
- Females have XX chromosomes. All oocytes contain one X chromosome, they are the homogametic sex.
- Males have XY chromosomes. Spermatozoa form two distinct populations, one containing X chromosomes and one containing Y chromosomes. They are the heterogametic sex.
- The Y chromosome is required to initiate male development.
- In absence of the Y chromosome, female gonads (Ovaries) will develop.
- The prime male determining gene is SRY (sex determining region of the Y chromosome).
- SRY is a very small piece of DNA that acts as a molecular switch to regulate structural genes and autosomal chromosomes, determining if and when they are to be activated.
- SRY encodes the protein Testes Determining Factor (TDF)
- The presence of SRY alone is sufficient to ensure development of male gonads (Testes).
- Female is the default sex, in absence of SRY female gonads (Ovaries) will develop.
- Subsequent gonadal development is dependent on a normal population of germ cells.
- Normal Oocyte growth requires the activity of both X chromosomes.
- Normal Spermatogenesis requires the activity of no more than one X chromosome.
- Early development of gonads proceeds similarly in both sexes. The gonads are derived from two distinct tissues:
- Somatic mesenchymal tissue forms the matrix of the gonad
- Primordial germ cells form the gametes
- Genital ridge forms from somatic mesenchyme.
- Primordial germ cells migrate to the genital ridge.
- At this stage it is not possible to discriminate between male and female gonads.
- Y chromosomal determination of gonadal sex is only visible when primordial germ cell colonisation is complete.
Male
- Sex cord cells proliferate to form the testes cord. During this period SRY is expressed for the first time within Sertoli cells (SRY is NOT expressed in primordial germ cells).
- Sex cords with a basement membrane become Semniferous Cords which give rise to Semniferous Tubules.
- Within the semniferous cords are two cell populations:
- Primordial germ cells - Prospermatogonia which give rise to Spermatozoa
- Mesodermal cord cells which give rise to Sertoli cells
- Between cords, the loose mesenchyme undergoes vascularisation and develops as stromal tissue.
- Within the stromal tissue, cells condense into clusters to form specialized endocrine units - the interstitial Leydig Cells
Female
- At the time the male gonad is undergoing marked changes under the direction of SRY, the female gonad continues to appear indifferent and does not express SRY.
- Small clusters of mesenchyme surround the germ cells to initiate formation of Primary Follicles, characteristic of the Ovary.
- In follicles:
- Mesenchymal cells give rise to Granulosa cells
- Germ cells give rise to Oocytes
Foetal sex differentiation
- Endocrine activity of the Ovaries is NOT essential for sex differentiation during foetal life, abnormal ovarian development will have no effect until puberty.
- Testes secrete two essential hormones:
- Steroidal hormones (mainly C19 androgens) from Leydig cells
- Mullarian Inhibiting Hormone (MIH) also known as Anti-Mullarian Hormone (AMH) from Sertoli Cells
- In absence of these testicular hormones, female differentiation occurs.
- Thus, sexual differentiation must be actively diverted down the male route, the female route requires no active intervention.
Internal Genetalia
- Male: Wolffian Duct developes from the Mesonephric Duct
- Female: Mullarian Ducts develop from the Paramesonephric Duct
- This is dependent on appropriate hormonal influence.
Male
- MIH from Sertoli cells and Androgens from Leydig cells prevent spontaneous development of female internal genetalia.
- Androgens actively maintain Wolffian Ducts, which give rise to male internal genetalia:
- Epididymis
- Vas Deferens
- Vesicular Glands/ Seminal Vesicles
- MIH causes Mullarian Ducts to regress
Female
- Wolffian Ducts spontaneously regress in absence of Androgens.
- Mullarian Ducts persist to give rise to female internal genetalia:
- Oviducts
- Uterus
- Cervix
- Cranial Vagina
- Normal Ovarian activity is NOT essential for the development of normal female internal genetalia.
External Genetalia
Male
- Potential to develop male of female external genetalia. Testosterone is required to develop male external genetalia.
- Androgen secretion from the Testes induces:
- Urethral folds to fuse to allow enclosure of the urethral tube. This, together with the cells from the genital swelling, forms the shaft of the Penis.
- Genital swellings fuse in the midline to allow formation of the Scrotum
- Genital Tubercle expands to give rise to the Glans Penis
Female
- Development is ensured by the absence of Testosterone, it is independent of Ovarian endocrine activity.
- Urethral folds and Genital Swellings remain separate to form the Labia Minora and Majora.
- Genital tubercle forms the Clitoris
- Exposure of the female tract to Androgens will masculinise external genetalia.
- Failure of proper endocrine communication between the gonads, internal and external genitalia can lead to dissociation of gonadal and genital sex.
Sexual Differentiation of the Brain
Male
- Testosterone secreted into the blood reaches the brain.
- Converted to Dehydrotestosterone and Oestradiol by Aromatase enzymes in the Hypothalamus.
- Oestradiol masculinises the brain
Female
- Alpha Fetoprotein binds Oestradiol, preventing it from crossing the blood-brain barrier.
- Oestradiol cannot access the Hypothalamus
- Protects female brain from masculising effects of Oestradiol.
Associated Disorders