Difference between revisions of "Equine Orthopaedics and Rheumatology Q&A 04"
Ggaitskell (talk | contribs) |
|||
| (2 intermediate revisions by one other user not shown) | |||
| Line 16: | Line 16: | ||
*the subcutaneous tissues. <br><br> | *the subcutaneous tissues. <br><br> | ||
There are no discernible abnormalities of the flexor tendons. The annular ligament was 4 mm thick, with the annular ligament and subcutaneous fibrosis being 7 mm thick. <br>'''Normal size of the palmar/plantar annular ligament is 1–2 mm'''. | There are no discernible abnormalities of the flexor tendons. The annular ligament was 4 mm thick, with the annular ligament and subcutaneous fibrosis being 7 mm thick. <br>'''Normal size of the palmar/plantar annular ligament is 1–2 mm'''. | ||
| − | |l1= | + | |l1= Annular Ligament Syndrome#Introduction |
|q2=What is the diagnosis? | |q2=What is the diagnosis? | ||
|a2=This horse is suffering from annular ligament syndrome (ALS). The three layers superficial to the flexor tendons are affected in different proportions between individual cases, and the division between the layers can be difficult to identify in some cases. <br><br> | |a2=This horse is suffering from annular ligament syndrome (ALS). The three layers superficial to the flexor tendons are affected in different proportions between individual cases, and the division between the layers can be difficult to identify in some cases. <br><br> | ||
As a result, the total thickness between the skin and flexor tendons is sometimes measured (mean normal thickness 3.7 mm ± 0.5 mm). | As a result, the total thickness between the skin and flexor tendons is sometimes measured (mean normal thickness 3.7 mm ± 0.5 mm). | ||
| − | |l2= | + | |l2= Annular Ligament Syndrome#Introduction |
|q3=What complications may be present? | |q3=What complications may be present? | ||
|a3=The full extent of the sheath should be evaluated in these cases to identify any adhesions. However, this requires some experience as adhesions can be overdiagnosed ultrasonographically. <br><br> | |a3=The full extent of the sheath should be evaluated in these cases to identify any adhesions. However, this requires some experience as adhesions can be overdiagnosed ultrasonographically. <br><br> | ||
Extra definition can be provided by prior distension of the sheath with, for example, a local analgesic agent following clinical examination, provided care is taken to prevent any air being iatrogenically introduced which will compromise the ultrasound image. | Extra definition can be provided by prior distension of the sheath with, for example, a local analgesic agent following clinical examination, provided care is taken to prevent any air being iatrogenically introduced which will compromise the ultrasound image. | ||
| − | |l3= | + | |l3= Annular Ligament Syndrome#Diagnosis |
|q4=What methods of treatment are available, and what is the prognosis? | |q4=What methods of treatment are available, and what is the prognosis? | ||
|a4= | |a4= | ||
| Line 31: | Line 31: | ||
*The prognosis is related to the primary cause and the presence of adhesions. In those cases of primary desmitis or secondary desmitis associated with aseptic digital sheath tenosynovitis, a prognosis of 60–70% return to full exercise can be expected. <br><br> | *The prognosis is related to the primary cause and the presence of adhesions. In those cases of primary desmitis or secondary desmitis associated with aseptic digital sheath tenosynovitis, a prognosis of 60–70% return to full exercise can be expected. <br><br> | ||
*Failure rate is thought to be related to the formation of adhesions. Intra-sheath hyaluronic acid can be used postoperatively to minimise this complication. | *Failure rate is thought to be related to the formation of adhesions. Intra-sheath hyaluronic acid can be used postoperatively to minimise this complication. | ||
| − | |l4= | + | |l4= Annular Ligament Syndrome#Treatment |
</FlashCard> | </FlashCard> | ||
Latest revision as of 19:08, 27 July 2011
| This question was provided by Manson Publishing as part of the OVAL Project. See more Equine Orthopaedic and Rheumatological questions |
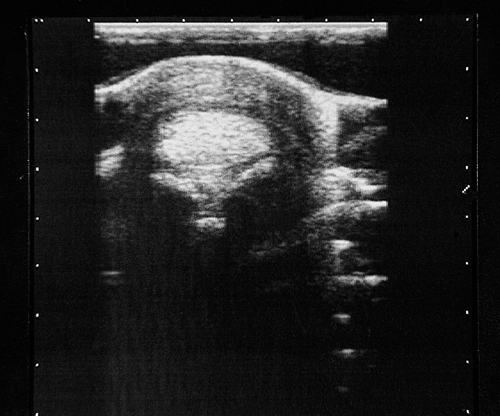
A nine-year-old pony mare has a left hindlimb lameness of two months duration. The lameness has not responded to rest. On clinical examination, the pony is only mildly lame but this is exacerbated by distal limb flexion. There is a digital sheath effusion and a ‘notch’ on the plantar aspect of the metatarsophalangeal joint.
| Question | Answer | Article | |
| Describe the ultrasonographic findings revealed in the image. | There is thickening of all the layers on the palmar aspect of the metatarsophalangeal region between the superficial digital flexor tendon (SDFT) and the skin. These layers consist of:
There are no discernible abnormalities of the flexor tendons. The annular ligament was 4 mm thick, with the annular ligament and subcutaneous fibrosis being 7 mm thick. |
Link to Article | |
| What is the diagnosis? | This horse is suffering from annular ligament syndrome (ALS). The three layers superficial to the flexor tendons are affected in different proportions between individual cases, and the division between the layers can be difficult to identify in some cases. As a result, the total thickness between the skin and flexor tendons is sometimes measured (mean normal thickness 3.7 mm ± 0.5 mm). |
Link to Article | |
| What complications may be present? | The full extent of the sheath should be evaluated in these cases to identify any adhesions. However, this requires some experience as adhesions can be overdiagnosed ultrasonographically. Extra definition can be provided by prior distension of the sheath with, for example, a local analgesic agent following clinical examination, provided care is taken to prevent any air being iatrogenically introduced which will compromise the ultrasound image. |
Link to Article | |
| What methods of treatment are available, and what is the prognosis? |
|
Link to Article | |