Difference between revisions of "Major Histocompatability Complexes"
Jump to navigation
Jump to search
(→MHC I) |
|||
| (89 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
| − | {{ | + | {{toplink |
| − | + | |backcolour = FFE4E1 | |
| − | ==Introduction | + | |linkpage =Immunology - WikiBlood |
| − | T-cells rely on Major Histocompatability Complexes (MHC) | + | |linktext =IMMUNOLOGY |
| + | |maplink = Adaptive Immune System (Concept Map) - WikiBlood | ||
| + | |tablelink = Adaptive Immune System (Table) - WikiBlood | ||
| + | |sublink1 =Adaptive Immune System - WikiBlood | ||
| + | |subtext1 =Adaptive Immune System | ||
| + | |pagetype =Blood | ||
| + | }} | ||
| + | |||
| + | =Introduction= | ||
| + | T-cells rely on Major Histocompatability Complexes (MHC) to present antigen fragments for their recognition. MHC has evolved to form two classes to present antigen: '''MHC I''' presents digestion fragments from antigen in '''cellular cytoplasm''', and '''MHC II''' presents digestion fragments from antigen in the '''tissue fluid'''. As such, MHC I tends to bind slightly smaller peptides (~9 amino acids) than MHC II (~15 amino acids). | ||
| + | |||
| + | =Classes= | ||
==MHC I== | ==MHC I== | ||
| + | [[Image:MHC I processing.jpg|thumb|200px|right|'''MHC I presentation pathway, courtesy of B. Catchpole, 2008''']] | ||
===Structure=== | ===Structure=== | ||
| − | + | * MHC class I is expressed on virtually all nucleated cells | |
| − | + | * MHC class I consists of a membrane-associated heavy chain bound non-covalently with a secreted light chain | |
| − | MHC class I is expressed on virtually all nucleated cells | + | ** Heavy chain: |
| − | + | *** Made up of three distinct extracellular protein domains | |
| − | + | **** α1, α2 and α3 | |
| − | The MHC class I domains are structurally and genetically related to immunoglobulin and TcR domains | + | *** The C- terminus is cytoplasmic |
| − | + | ** Light chain: | |
| − | MHC class I molecules are folded to form specific 3-dimensional structures | + | *** Known as β2-microglobulin |
| + | *** Similar in structure to one of the heavy chain domains | ||
| + | *** Not membrane associated | ||
| + | **** But binds to the α3-domain of the heavy chain | ||
| + | * The MHC class I domains are structurally and genetically related to immunoglobulin and TcR domains | ||
| + | ** The outer domains (α1 and α2) are like the variable domains | ||
| + | ** The α3 domain and β2m are like thrconstant domains | ||
| + | * MHC class I molecules are folded to form specific 3-dimensional structures | ||
| + | ** The α1 and α2 domains are folded to produce an antigen-binding groove | ||
| + | *** This groove can bind molecules of a limited size only (8-10 amino acids) | ||
| + | **** This limits the size of epitope seen by the T-cell receptors | ||
===Presentation Pathway=== | ===Presentation Pathway=== | ||
| − | + | *Viral proteins are broken down to peptides by the proteasome and transferred to the endoplasmic reticulum via TAP (Transporters associated with Antigen Processing) molecules | |
| − | + | *In the ER< peptides are processed with empty MHC I molecules and exported to the cell surface for presentation | |
| + | * MHC class I molecules bind antigenic peptides derived from within the cell and present these to the T-cell receptors of '''CD8+ T-cells''' | ||
| + | * Endogenously produced proteins are produced in the cell cytoplasm | ||
| + | ** Intracellular pathogens utilise this cellular metabolic machinery for protein synthesis | ||
| + | ** Many of the proteins synthesised are not used and are re-utilised by the cell | ||
| + | *** Peptides from these proteins are transported to the Golgi apparatus by specific transporter molecules | ||
| + | *** These peptides then interact with newly synthesized MHC class I molecules. | ||
| + | * Only MHC class I that is associated with peptide will be expressed at the surface | ||
| + | ** The immune system is therefore able to see antigen from intracleeular pathogens | ||
==MHC II== | ==MHC II== | ||
| − | |||
| − | |||
===Structure=== | ===Structure=== | ||
| − | MHC class II is expressed mainly on | + | * MHC class II is expressed mainly on '''macrophages''', '''dendritic cells''' and '''B-lymphocytes''' |
| − | + | * MHC class II consists of membrane-associated α and β chains | |
| − | The 3-dimensional structure of MHC class II is similar to MHC class I | + | ** Each chain is a transmembrane glycoprotein |
| − | + | ** The extracellular parts of each chain have two Ig-like domains | |
| − | + | *** α1 and 7alpha;2, β1 and β2 | |
| − | + | **** The outer domains (α1 and β1) are variable-like | |
| − | + | **** The inner domains (α2 and β2) are constant-like | |
| − | * | + | * The 3-dimensional structure of MHC class II is similar to MHC class I |
| − | * | + | ** The outer domains of the α and β chains fold in a similar way to the α1 and α2 domains of class I |
| − | + | *** Produce the antigen-binding groove | |
| − | * | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | ===Function=== | |
| + | * MHC class II molecules bind antigenic peptides and present them to TCR on CD4+ T-cells | ||
| + | * The antigen-binding groove is larger and more open than that of MHC class I | ||
| + | ** MHC II can therefore interact with larger peptides | ||
| + | * MHC class II are present on those cells that have antigen-processing ability | ||
| + | ** Interact with antigenic peptides originating from an extracellular source | ||
| + | * After synthesis, MHC class II molecules are transported into special endosomes | ||
| + | ** These endosomes fuse with lysosomes that contain the digested remnants of phagocytosed microorganisms | ||
| + | *** The peptides from the lysosome interact with the MHC class II molecules | ||
| + | **** The peptide-MHC class II complex gets transported to the cell surface | ||
| − | MHC molecules | + | =Interaction of MHC With Antigen= |
| + | * The MHC molecules do not recognise specific amino acid sequences of antigens | ||
| + | ** Instead, they recognise particular motifs of amino acids | ||
| + | * The association of any MHC allele with a peptide may be determined by the presence of as few as two amino acids | ||
| + | ** However, these determinants must be present within a particular array | ||
| + | * The actual identity of the amino acids in not important for MHC binding | ||
| + | ** Instead, the physical and chemical characteristics of the amino acid are vital | ||
| + | * Interactions of individual amino acids at the head and tail of the peptide-binding groove control the binding of peptides | ||
| + | ** Are mainly positioned at the floor of the antigen-binding groove, or within the helices facing into the groove | ||
| + | ** These MHC amino acids associate with amino acids near the ends of the peptides | ||
| + | *** The intervening stretch of peptide folds into a helix within the groove | ||
| + | *** Is the target for T cell receptor recognition | ||
==TCR-MHC Interaction== | ==TCR-MHC Interaction== | ||
| − | + | * Only peptide associated with self-MHC will interact with and activate T-cells | |
| − | Only peptide associated with MHC will interact with and activate | + | ** T-cells cannot be activated by a peptide on a foreign cell |
| + | ** T-cells will react against foreign MHC molecules | ||
| + | *** This is the basis of graft rejection | ||
| − | + | ==The Genetics of the MHC== | |
| − | + | * Different individuals have different critical amino acids within the MHC | |
| − | ==MHC | + | ** I.e. different amino acids that determine peptide binding |
| − | + | ** This variation is termed '''MHC polymorphism''' | |
| − | + | * There are millions of variations in antibodies and TCR | |
| − | + | ** However, with MHC there is very limited variation between molecules | |
| − | Different individuals have different critical amino acids within the MHC | ||
| − | * | ||
| − | |||
| − | |||
| − | |||
* MHC polymorphism has been best studied in the human | * MHC polymorphism has been best studied in the human | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| + | ==In the Human== | ||
| + | * Humans express: | ||
| + | ** Three types (loci) of MHC class I molecules | ||
| + | *** HLA (Human Leukocyte Antigen)- A, B, and C | ||
| + | ** Three loci of MHC class II molecules | ||
| + | *** HLA-DP, DQ and DR | ||
| + | * In the entire human population there are only approximately 50 different variants (alleles) at each MHC class I and class II locus | ||
| + | ** The variation within MHC class I is entirely on the class I heavy chain | ||
| + | *** The β2m is invariant | ||
| + | ** The variation within MHC class II is mainly within the β chains | ||
| + | * Every individual has two alleles at each MHC locus | ||
| + | ** One inherited from each parent | ||
| + | ** Any individual will therfore express two variants at most at each locus | ||
| + | *** This gives a maximum variability for an individual of: | ||
| + | **** 6 different variants of MHC class I | ||
| + | ***** 2 each of HLA- A, B and C | ||
| + | **** 6 different variants of MHC class II | ||
| + | ***** 2 each of HLA- DP, DQ and DR | ||
| + | * Many animal species have fewer loci than the human | ||
| + | ** E.g. ruminants have no MHC class II DP | ||
| − | + | ==MHC and Disease== | |
| − | + | * Antigen from a pathogen has to be seen by the host MHC before an efficient immune response can occur | |
| − | + | ** There is therefore a constant evolutionary battle between the host and the pathogen | |
| − | + | *** There is selective pressure on the pathogen to evolve proteins that do not interact with the host MHC | |
| + | *** There is selective pressure on the host to continue to recognize the pathogen | ||
| + | * The consequence of this parallel evolution is that host-pathogen relationships can lead to the selection of particular MHC variants, for example: | ||
| + | ** MHC class II alleles DR13/DR1*1301 are prevalent in Central and Western Africa | ||
| + | *** Impart resistance to malaria | ||
| + | ** MHC-DRB1 is prevalent in Western Europe, but rare in the Inuit populations of North America | ||
| + | *** Associated with the clearance of hepatitis B infection in Western Europe | ||
| + | *** Inuits have the highest incidence of hepatitis B in the world | ||
| + | ** In humans there are also strong associations between certain alleles and some autoimmune diseases, for example: | ||
| + | *** Diabetes mellitus | ||
| + | *** Ankylosing spondylitis | ||
| + | *** Rheumatoid arthritis | ||
Revision as of 15:29, 28 August 2008
|
|
Introduction
T-cells rely on Major Histocompatability Complexes (MHC) to present antigen fragments for their recognition. MHC has evolved to form two classes to present antigen: MHC I presents digestion fragments from antigen in cellular cytoplasm, and MHC II presents digestion fragments from antigen in the tissue fluid. As such, MHC I tends to bind slightly smaller peptides (~9 amino acids) than MHC II (~15 amino acids).
Classes
MHC I
Structure
- MHC class I is expressed on virtually all nucleated cells
- MHC class I consists of a membrane-associated heavy chain bound non-covalently with a secreted light chain
- Heavy chain:
- Made up of three distinct extracellular protein domains
- α1, α2 and α3
- The C- terminus is cytoplasmic
- Made up of three distinct extracellular protein domains
- Light chain:
- Known as β2-microglobulin
- Similar in structure to one of the heavy chain domains
- Not membrane associated
- But binds to the α3-domain of the heavy chain
- Heavy chain:
- The MHC class I domains are structurally and genetically related to immunoglobulin and TcR domains
- The outer domains (α1 and α2) are like the variable domains
- The α3 domain and β2m are like thrconstant domains
- MHC class I molecules are folded to form specific 3-dimensional structures
- The α1 and α2 domains are folded to produce an antigen-binding groove
- This groove can bind molecules of a limited size only (8-10 amino acids)
- This limits the size of epitope seen by the T-cell receptors
- This groove can bind molecules of a limited size only (8-10 amino acids)
- The α1 and α2 domains are folded to produce an antigen-binding groove
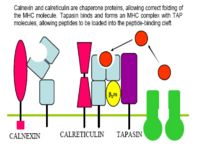
Presentation Pathway
- Viral proteins are broken down to peptides by the proteasome and transferred to the endoplasmic reticulum via TAP (Transporters associated with Antigen Processing) molecules
- In the ER< peptides are processed with empty MHC I molecules and exported to the cell surface for presentation
- MHC class I molecules bind antigenic peptides derived from within the cell and present these to the T-cell receptors of CD8+ T-cells
- Endogenously produced proteins are produced in the cell cytoplasm
- Intracellular pathogens utilise this cellular metabolic machinery for protein synthesis
- Many of the proteins synthesised are not used and are re-utilised by the cell
- Peptides from these proteins are transported to the Golgi apparatus by specific transporter molecules
- These peptides then interact with newly synthesized MHC class I molecules.
- Only MHC class I that is associated with peptide will be expressed at the surface
- The immune system is therefore able to see antigen from intracleeular pathogens
MHC II
Structure
- MHC class II is expressed mainly on macrophages, dendritic cells and B-lymphocytes
- MHC class II consists of membrane-associated α and β chains
- Each chain is a transmembrane glycoprotein
- The extracellular parts of each chain have two Ig-like domains
- α1 and 7alpha;2, β1 and β2
- The outer domains (α1 and β1) are variable-like
- The inner domains (α2 and β2) are constant-like
- α1 and 7alpha;2, β1 and β2
- The 3-dimensional structure of MHC class II is similar to MHC class I
- The outer domains of the α and β chains fold in a similar way to the α1 and α2 domains of class I
- Produce the antigen-binding groove
- The outer domains of the α and β chains fold in a similar way to the α1 and α2 domains of class I
Function
- MHC class II molecules bind antigenic peptides and present them to TCR on CD4+ T-cells
- The antigen-binding groove is larger and more open than that of MHC class I
- MHC II can therefore interact with larger peptides
- MHC class II are present on those cells that have antigen-processing ability
- Interact with antigenic peptides originating from an extracellular source
- After synthesis, MHC class II molecules are transported into special endosomes
- These endosomes fuse with lysosomes that contain the digested remnants of phagocytosed microorganisms
- The peptides from the lysosome interact with the MHC class II molecules
- The peptide-MHC class II complex gets transported to the cell surface
- The peptides from the lysosome interact with the MHC class II molecules
- These endosomes fuse with lysosomes that contain the digested remnants of phagocytosed microorganisms
Interaction of MHC With Antigen
- The MHC molecules do not recognise specific amino acid sequences of antigens
- Instead, they recognise particular motifs of amino acids
- The association of any MHC allele with a peptide may be determined by the presence of as few as two amino acids
- However, these determinants must be present within a particular array
- The actual identity of the amino acids in not important for MHC binding
- Instead, the physical and chemical characteristics of the amino acid are vital
- Interactions of individual amino acids at the head and tail of the peptide-binding groove control the binding of peptides
- Are mainly positioned at the floor of the antigen-binding groove, or within the helices facing into the groove
- These MHC amino acids associate with amino acids near the ends of the peptides
- The intervening stretch of peptide folds into a helix within the groove
- Is the target for T cell receptor recognition
TCR-MHC Interaction
- Only peptide associated with self-MHC will interact with and activate T-cells
- T-cells cannot be activated by a peptide on a foreign cell
- T-cells will react against foreign MHC molecules
- This is the basis of graft rejection
The Genetics of the MHC
- Different individuals have different critical amino acids within the MHC
- I.e. different amino acids that determine peptide binding
- This variation is termed MHC polymorphism
- There are millions of variations in antibodies and TCR
- However, with MHC there is very limited variation between molecules
- MHC polymorphism has been best studied in the human
In the Human
- Humans express:
- Three types (loci) of MHC class I molecules
- HLA (Human Leukocyte Antigen)- A, B, and C
- Three loci of MHC class II molecules
- HLA-DP, DQ and DR
- Three types (loci) of MHC class I molecules
- In the entire human population there are only approximately 50 different variants (alleles) at each MHC class I and class II locus
- The variation within MHC class I is entirely on the class I heavy chain
- The β2m is invariant
- The variation within MHC class II is mainly within the β chains
- The variation within MHC class I is entirely on the class I heavy chain
- Every individual has two alleles at each MHC locus
- One inherited from each parent
- Any individual will therfore express two variants at most at each locus
- This gives a maximum variability for an individual of:
- 6 different variants of MHC class I
- 2 each of HLA- A, B and C
- 6 different variants of MHC class II
- 2 each of HLA- DP, DQ and DR
- 6 different variants of MHC class I
- This gives a maximum variability for an individual of:
- Many animal species have fewer loci than the human
- E.g. ruminants have no MHC class II DP
MHC and Disease
- Antigen from a pathogen has to be seen by the host MHC before an efficient immune response can occur
- There is therefore a constant evolutionary battle between the host and the pathogen
- There is selective pressure on the pathogen to evolve proteins that do not interact with the host MHC
- There is selective pressure on the host to continue to recognize the pathogen
- There is therefore a constant evolutionary battle between the host and the pathogen
- The consequence of this parallel evolution is that host-pathogen relationships can lead to the selection of particular MHC variants, for example:
- MHC class II alleles DR13/DR1*1301 are prevalent in Central and Western Africa
- Impart resistance to malaria
- MHC-DRB1 is prevalent in Western Europe, but rare in the Inuit populations of North America
- Associated with the clearance of hepatitis B infection in Western Europe
- Inuits have the highest incidence of hepatitis B in the world
- In humans there are also strong associations between certain alleles and some autoimmune diseases, for example:
- Diabetes mellitus
- Ankylosing spondylitis
- Rheumatoid arthritis
- MHC class II alleles DR13/DR1*1301 are prevalent in Central and Western Africa