Difference between revisions of "Toxoplasmosis - Sheep"
| (29 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
| − | {{ | + | {{unfinished}} |
| − | == | + | |
| − | Toxoplasmosis is the disease caused by '' | + | ==Description== |
| + | |||
| + | Toxoplasmosis is the disease caused by ''Toxoplasma gondii'', an intracelluler protozoan parasite. Although the definitive host is the cat, ''T. gondii'' can infect all mammals including man and is a significant cause of abortion in sheep and goats. Toxoplasmosis does not seem to cause disease in cattle. | ||
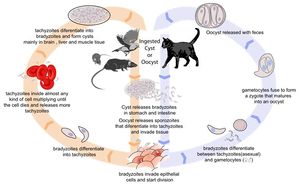
[[Image:Toxoplasmosis Life Cycle.jpg|thumb|right|300px| Life cycle of ''Toxoplasma gondii''. Source: Wikimedia Commons; Author: LadyofHats (2010)]] | [[Image:Toxoplasmosis Life Cycle.jpg|thumb|right|300px| Life cycle of ''Toxoplasma gondii''. Source: Wikimedia Commons; Author: LadyofHats (2010)]] | ||
| + | ===Life Cycle=== | ||
| + | |||
| + | There are three infectious stages of ''Toxoplasma gondii'': 1) sporozoites; 2) actively reproducing tachyzoites; and 3) slowly multiplying bradyzoites. Tachyzoites and bradyzoites are found in tissue cysts, whereas sporozoites are containted within oocysts, which are excreted in the faeces. This means that the protozoa can be transmitted by ingestion of oocyst-contaminated food or water, or by consumption of infected tissue. | ||
| + | |||
| + | In naive cats, ''Toxoplasma gondii'' undergoes an enteroepithelial life cycle. Cats ingests intermediate hosts containing tissue cysts, which release bradyzoites in the gastrointestinal tract. The bradyzoites penetrate the small intestinal epithelium and sexual reproductio ensues, eventually resulting the production of oocysts. Oocysts are passed in the cat's faeces and sporulate to become infectious once in the environment. These can then be ingested by other mammals, including sheep. | ||
| + | |||
| + | When sheep ingest oocysts, ''T.gondii'' intiates extraintestinal replication. This process is the same for all hosts, and also occurs when carnivores ingest tissue cysts in other animals. Sporozoites (or bradyzoites, if cysts are consumed) are released in the intestine to infect the intestinal epithelium where they replicate. This produces tachyzoites, which reproduce asexually within the infected cell. When the infected cell ruptures, tachyzoites are released and disseminate via blood and lymph to infect other tissues. Tachyzoites then replicate intracellularly again and the process continues until the host becomes immune or dies. If the infected cell does not burst, tachyzoites eventually encyst as bradyzoites and persist for the life of the host. Cyst are most commonly found in the brain or skeletal muscle, and are a source of infection for carnivorous hosts. | ||
| + | |||
==Transmission to Sheep== | ==Transmission to Sheep== | ||
| + | |||
===Oocysts in the Environment=== | ===Oocysts in the Environment=== | ||
| − | As the definitive hosts of ''Toxoplasma gondii'', cats become infected when they hunt and eat infected wild rodents and birds. Rodents are a particularly important source of | + | |
| + | As the definitive hosts of ''Toxoplasma gondii'', cats become infected when they hunt and eat infected wild rodents and birds. Rodents are a particularly important source of feline infection, as they can pass ''T. gondii'' infection to their offspring without causing clinical disease. This means that a farm may develop a reservoir of ''T. gondii'' tissue cysts with the potential to cause feline infection and massive oocyst excretion when a cat is introduced to the environment. Between days 3 and 14 post-infection, cats shed over 100 million of oocysts in their faeces. Studies have shown an association between ovine toxoplasma infection, and the contamination of feed or grazing with sporulated oocysts<sup>1</sup>, highligting the importance of oocysts as a source of infection for sheep. It has also been demonstrated that the prevalence of ovine toxoplasmosis varies with the presence of cats on a farm<sup>2</sup>. | ||
===Congenital Transmission=== | ===Congenital Transmission=== | ||
| + | |||
Apart from ingestion of oocysts in the environment, the only other method of transmission of toxoplasmosis to sheep is vertical spread from mother to foetus during pregnancy. This is because sheep are herbivorous, and do not consume animal tissues containing cysts. The outcome of transplacental infection depends on the stage of pregnancy. Infection in early gestation usually causes foetal death, as the foetal immune system is immature at this stage. In mid-gestation, infection may cause the birth of weak or stillborn lambs, sometimes accompanied by a mummified sibling. Ewes infected in the third trimester normally give birth to infected but clinically normal lambs. | Apart from ingestion of oocysts in the environment, the only other method of transmission of toxoplasmosis to sheep is vertical spread from mother to foetus during pregnancy. This is because sheep are herbivorous, and do not consume animal tissues containing cysts. The outcome of transplacental infection depends on the stage of pregnancy. Infection in early gestation usually causes foetal death, as the foetal immune system is immature at this stage. In mid-gestation, infection may cause the birth of weak or stillborn lambs, sometimes accompanied by a mummified sibling. Ewes infected in the third trimester normally give birth to infected but clinically normal lambs. | ||
==Signalment== | ==Signalment== | ||
| + | |||
Ovine toxoplasmosis is only clinically apparent when primary infection of a pregnant animal occurs. | Ovine toxoplasmosis is only clinically apparent when primary infection of a pregnant animal occurs. | ||
==Diagnosis== | ==Diagnosis== | ||
| − | |||
===Clinical Signs=== | ===Clinical Signs=== | ||
| + | |||
The signs of toxoplasmosis in sheep manifest following the exposure of a naive pregnant ewe to oocysts. The sporozoites ingested excyst in the digestive tract and penetrate the intestinal epithelium, before reaching the mesenteric lymph nodes around day 4 post-infection. Here, they cause lymphomegaly and focal necrosis before contributing to a parisitaemia from day 5. Pyrexia is associated with the development of parasitaemia. | The signs of toxoplasmosis in sheep manifest following the exposure of a naive pregnant ewe to oocysts. The sporozoites ingested excyst in the digestive tract and penetrate the intestinal epithelium, before reaching the mesenteric lymph nodes around day 4 post-infection. Here, they cause lymphomegaly and focal necrosis before contributing to a parisitaemia from day 5. Pyrexia is associated with the development of parasitaemia. | ||
| − | Following dissemination of ''T. gondii'' in the blood, many tissues become infected. Parasitaemia ends when the maternal immune response becomes effective, and protozoa start to encyst as | + | Following dissemination of ''T. gondii'' in the blood, many tissues become infected. Parasitaemia ends when the maternal immune response becomes effective, and protozoa start to encyst as bradizoites. In pregnant animals, the uterus is an immunoprivileged site, and the outcome of foetal infection is influenced by the stage of gestation. In early pregnancy, the foetus is unable to mount any immune response, and so cannot inhibit parasite multiplication. The foetus rapidly dies and is resorbed. In a flock, this is visable clinically as large numbers of barren ewes. In mid-gestation (70-120 days), infection can again be fatal. This causes a mummified foetus which is often twinned with a lamb that is stillborn or weak. Abortion due to infection at 70-120 days gestation tends to occur in very late pregnancy. Because the foetal immune system is well developed in late pregnancy, infection at this stage will be resisted, and the lamb will be born infected but alive. |
===Laboratory Tests=== | ===Laboratory Tests=== | ||
| − | |||
===Pathology=== | ===Pathology=== | ||
| − | + | When infection in the | |
| + | placentome is initiated, parasite multiplication causes | ||
| + | multiple foci of necrosis29. These foci of tissue | ||
| + | damage expand throughout the remainder of gestation | ||
| + | until abortion or birth when they may be macroscopically | ||
| + | visible as white spots in the cotyledons of | ||
| + | the shed placenta, a feature used to aid diagnozsis"31. | ||
| + | Diagnosis is also helped by histological examination | ||
| + | of the brain where there may be both primary | ||
| + | and secondary lesions32'33. Glial foci, surrounding a | ||
| + | necrotic and sometimes mineralized centre, often | ||
| + | associated with a mild lymphoid meningitis, represent | ||
| + | a fetal immune response following direct damage by | ||
| + | parasite multiplication. Focal leukomalacia is also | ||
| + | common and is thought to be due to fetal anoxia in | ||
| + | late gestation caused by advanced focal necrosis in | ||
| + | the placentome preventing sufficient oxygen transfer | ||
| + | from mother to fetus33. Focal inflammatory lesions | ||
| + | and associated diffuse lymphoid infiltrates may also | ||
| + | be found in the liver, lung and heart and less | ||
| + | frequently in kidneys and skeletal muscle33. | ||
| + | These foci of tissue | ||
| + | damage expand throughout the remainder of gestation | ||
| + | until abortion or birth when they may be macroscopically | ||
| + | visible as white spots in the cotyledons of | ||
| + | the shed placenta, a feature used to aid diagnozsis"31. | ||
| + | Diagnosis is also helped by histological examination | ||
| + | of the brain where there may be both primary | ||
| + | and secondary lesions32'33. Glial foci, surrounding a | ||
| + | necrotic and sometimes mineralized centre, often | ||
| + | associated with a mild lymphoid meningitis, represent | ||
| + | a fetal immune response following direct damage by | ||
| + | parasite multiplication. Focal leukomalacia is also | ||
| + | common and is thought to be due to fetal anoxia in | ||
| + | late gestation caused by advanced focal necrosis in | ||
| + | the placentome preventing sufficient oxygen transfer | ||
| + | from mother to fetus33. Focal inflammatory lesions | ||
| + | and associated diffuse lymphoid infiltrates may also | ||
| + | be found in the liver, lung and heart and less | ||
| + | frequently in kidneys and skeletal muscle33. | ||
| + | Aborted ewes show focal necrotic placentitis with white lesions in the cotyledons and foetal tissue | ||
| − | + | Placental | |
| + | tissue from infected ewes may also show characteristic | ||
| + | gross white spot lesions which are visible to | ||
| + | the naked eye and are areas of necrosis in the tissue | ||
| + | which will limit its effective function in supporting | ||
| + | the pregnancy (Buxton, 1990). | ||
==Treatment== | ==Treatment== | ||
| − | |||
| − | + | *Toxovax vaccine | |
| + | ***Live, avirulent strain of ''Toxoplasma'' | ||
| + | ***Does not form bradyzoites or tissue cysts | ||
| + | ***Killed by host immune system | ||
| + | ***Single dose given 6 weeks before tupping | ||
| + | ***Protects for 2 years | ||
| + | ***Immunity boosted by natural challenge | ||
| + | **Medicated feed can be given daily during the main risk period | ||
| + | ***14 weeks before lambing | ||
| + | **The best method of protection is to prevent cats from contaminating the pasture, lambing sheds and feed stores | ||
| − | The | + | The extent of environmental |
| + | contamination with T. gondii oocysts is thus | ||
| + | related to the distribution and behaviour of cats. | ||
| + | Measures to reduce environmental contamination | ||
| + | by oocysts should be aimed at reducing the number | ||
| + | of cats capable of shedding oocysts. This would include | ||
| + | attempts to limit their breeding. If male cats are | ||
| + | caught, neutered and returned to their colonies the | ||
| + | stability ofthe colony is maintained; fertile male cats | ||
| + | do not challenge the neutered males12 and breeding | ||
| + | is controlled. Thus the maintenance ofa small healthy | ||
| + | population of mature cats will reduce oocyst excretion | ||
| + | as well as help to control rodents. Sheep feed should be | ||
| + | kept covered at all times to prevent its contamination | ||
| + | by cat faeces. | ||
==Prognosis== | ==Prognosis== | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==Links== | ==Links== | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==References== | ==References== | ||
| Line 58: | Line 124: | ||
#Plant, J Wet al (1974) Toxoplasma infection and abortion in sheep associated with feeding of grain contaminated with cat faeces. ''Australian Veterinary Journal'', '''50''', 19–21. | #Plant, J Wet al (1974) Toxoplasma infection and abortion in sheep associated with feeding of grain contaminated with cat faeces. ''Australian Veterinary Journal'', '''50''', 19–21. | ||
#Skjerve, E et al (1998). Risk factors for the presence of antibodies to Toxoplasma gondii in Norwegian slaughter lambs. ''Preventative Veterinary Medicine'', '''35''', 219–227. | #Skjerve, E et al (1998). Risk factors for the presence of antibodies to Toxoplasma gondii in Norwegian slaughter lambs. ''Preventative Veterinary Medicine'', '''35''', 219–227. | ||
| − | |||
#Buxton, D (1990) Ovine toxoplasmosis: a review. ''Journal of the Royal Society of Medicine'', '''83''', 509-511. | #Buxton, D (1990) Ovine toxoplasmosis: a review. ''Journal of the Royal Society of Medicine'', '''83''', 509-511. | ||
#Innes, E A et al (2009) Ovine toxoplasmosis. ''Parastiology'', '''136''', 1887–1894. | #Innes, E A et al (2009) Ovine toxoplasmosis. ''Parastiology'', '''136''', 1887–1894. | ||
#Buxton, D et all (2007) Toxoplasma gondii and ovine toxoplasmosis: New aspects of an old story. ''Veterinary Parasitology'', '''147''', 25-28. | #Buxton, D et all (2007) Toxoplasma gondii and ovine toxoplasmosis: New aspects of an old story. ''Veterinary Parasitology'', '''147''', 25-28. | ||
#Dubey, J P (2009) Toxoplasmosis in sheep — The last 20 years. ''Veterinary Parasitology'', '''163''', 1-14. | #Dubey, J P (2009) Toxoplasmosis in sheep — The last 20 years. ''Veterinary Parasitology'', '''163''', 1-14. | ||
| − | + | [[Category:Tissue_Cyst_Forming_Coccidia]][[Category:Sheep]] | |
| − | + | [[Category:To_Do_-_Lizzie]] | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | [[Category: | ||
| − | [[Category: | ||
Revision as of 16:26, 13 August 2010
| This article is still under construction. |
Description
Toxoplasmosis is the disease caused by Toxoplasma gondii, an intracelluler protozoan parasite. Although the definitive host is the cat, T. gondii can infect all mammals including man and is a significant cause of abortion in sheep and goats. Toxoplasmosis does not seem to cause disease in cattle.
Life Cycle
There are three infectious stages of Toxoplasma gondii: 1) sporozoites; 2) actively reproducing tachyzoites; and 3) slowly multiplying bradyzoites. Tachyzoites and bradyzoites are found in tissue cysts, whereas sporozoites are containted within oocysts, which are excreted in the faeces. This means that the protozoa can be transmitted by ingestion of oocyst-contaminated food or water, or by consumption of infected tissue.
In naive cats, Toxoplasma gondii undergoes an enteroepithelial life cycle. Cats ingests intermediate hosts containing tissue cysts, which release bradyzoites in the gastrointestinal tract. The bradyzoites penetrate the small intestinal epithelium and sexual reproductio ensues, eventually resulting the production of oocysts. Oocysts are passed in the cat's faeces and sporulate to become infectious once in the environment. These can then be ingested by other mammals, including sheep.
When sheep ingest oocysts, T.gondii intiates extraintestinal replication. This process is the same for all hosts, and also occurs when carnivores ingest tissue cysts in other animals. Sporozoites (or bradyzoites, if cysts are consumed) are released in the intestine to infect the intestinal epithelium where they replicate. This produces tachyzoites, which reproduce asexually within the infected cell. When the infected cell ruptures, tachyzoites are released and disseminate via blood and lymph to infect other tissues. Tachyzoites then replicate intracellularly again and the process continues until the host becomes immune or dies. If the infected cell does not burst, tachyzoites eventually encyst as bradyzoites and persist for the life of the host. Cyst are most commonly found in the brain or skeletal muscle, and are a source of infection for carnivorous hosts.
Transmission to Sheep
Oocysts in the Environment
As the definitive hosts of Toxoplasma gondii, cats become infected when they hunt and eat infected wild rodents and birds. Rodents are a particularly important source of feline infection, as they can pass T. gondii infection to their offspring without causing clinical disease. This means that a farm may develop a reservoir of T. gondii tissue cysts with the potential to cause feline infection and massive oocyst excretion when a cat is introduced to the environment. Between days 3 and 14 post-infection, cats shed over 100 million of oocysts in their faeces. Studies have shown an association between ovine toxoplasma infection, and the contamination of feed or grazing with sporulated oocysts1, highligting the importance of oocysts as a source of infection for sheep. It has also been demonstrated that the prevalence of ovine toxoplasmosis varies with the presence of cats on a farm2.
Congenital Transmission
Apart from ingestion of oocysts in the environment, the only other method of transmission of toxoplasmosis to sheep is vertical spread from mother to foetus during pregnancy. This is because sheep are herbivorous, and do not consume animal tissues containing cysts. The outcome of transplacental infection depends on the stage of pregnancy. Infection in early gestation usually causes foetal death, as the foetal immune system is immature at this stage. In mid-gestation, infection may cause the birth of weak or stillborn lambs, sometimes accompanied by a mummified sibling. Ewes infected in the third trimester normally give birth to infected but clinically normal lambs.
Signalment
Ovine toxoplasmosis is only clinically apparent when primary infection of a pregnant animal occurs.
Diagnosis
Clinical Signs
The signs of toxoplasmosis in sheep manifest following the exposure of a naive pregnant ewe to oocysts. The sporozoites ingested excyst in the digestive tract and penetrate the intestinal epithelium, before reaching the mesenteric lymph nodes around day 4 post-infection. Here, they cause lymphomegaly and focal necrosis before contributing to a parisitaemia from day 5. Pyrexia is associated with the development of parasitaemia.
Following dissemination of T. gondii in the blood, many tissues become infected. Parasitaemia ends when the maternal immune response becomes effective, and protozoa start to encyst as bradizoites. In pregnant animals, the uterus is an immunoprivileged site, and the outcome of foetal infection is influenced by the stage of gestation. In early pregnancy, the foetus is unable to mount any immune response, and so cannot inhibit parasite multiplication. The foetus rapidly dies and is resorbed. In a flock, this is visable clinically as large numbers of barren ewes. In mid-gestation (70-120 days), infection can again be fatal. This causes a mummified foetus which is often twinned with a lamb that is stillborn or weak. Abortion due to infection at 70-120 days gestation tends to occur in very late pregnancy. Because the foetal immune system is well developed in late pregnancy, infection at this stage will be resisted, and the lamb will be born infected but alive.
Laboratory Tests
Pathology
When infection in the placentome is initiated, parasite multiplication causes multiple foci of necrosis29. These foci of tissue damage expand throughout the remainder of gestation until abortion or birth when they may be macroscopically visible as white spots in the cotyledons of the shed placenta, a feature used to aid diagnozsis"31. Diagnosis is also helped by histological examination of the brain where there may be both primary and secondary lesions32'33. Glial foci, surrounding a necrotic and sometimes mineralized centre, often associated with a mild lymphoid meningitis, represent a fetal immune response following direct damage by parasite multiplication. Focal leukomalacia is also common and is thought to be due to fetal anoxia in late gestation caused by advanced focal necrosis in the placentome preventing sufficient oxygen transfer from mother to fetus33. Focal inflammatory lesions and associated diffuse lymphoid infiltrates may also be found in the liver, lung and heart and less frequently in kidneys and skeletal muscle33. These foci of tissue damage expand throughout the remainder of gestation until abortion or birth when they may be macroscopically visible as white spots in the cotyledons of the shed placenta, a feature used to aid diagnozsis"31. Diagnosis is also helped by histological examination of the brain where there may be both primary and secondary lesions32'33. Glial foci, surrounding a necrotic and sometimes mineralized centre, often associated with a mild lymphoid meningitis, represent a fetal immune response following direct damage by parasite multiplication. Focal leukomalacia is also common and is thought to be due to fetal anoxia in late gestation caused by advanced focal necrosis in the placentome preventing sufficient oxygen transfer from mother to fetus33. Focal inflammatory lesions and associated diffuse lymphoid infiltrates may also be found in the liver, lung and heart and less frequently in kidneys and skeletal muscle33. Aborted ewes show focal necrotic placentitis with white lesions in the cotyledons and foetal tissue
Placental tissue from infected ewes may also show characteristic gross white spot lesions which are visible to the naked eye and are areas of necrosis in the tissue which will limit its effective function in supporting the pregnancy (Buxton, 1990).
Treatment
- Toxovax vaccine
- Live, avirulent strain of Toxoplasma
- Does not form bradyzoites or tissue cysts
- Killed by host immune system
- Single dose given 6 weeks before tupping
- Protects for 2 years
- Immunity boosted by natural challenge
- Medicated feed can be given daily during the main risk period
- 14 weeks before lambing
- The best method of protection is to prevent cats from contaminating the pasture, lambing sheds and feed stores
The extent of environmental contamination with T. gondii oocysts is thus related to the distribution and behaviour of cats. Measures to reduce environmental contamination by oocysts should be aimed at reducing the number of cats capable of shedding oocysts. This would include attempts to limit their breeding. If male cats are caught, neutered and returned to their colonies the stability ofthe colony is maintained; fertile male cats do not challenge the neutered males12 and breeding is controlled. Thus the maintenance ofa small healthy population of mature cats will reduce oocyst excretion as well as help to control rodents. Sheep feed should be kept covered at all times to prevent its contamination by cat faeces.
Prognosis
Links
References
- Plant, J Wet al (1974) Toxoplasma infection and abortion in sheep associated with feeding of grain contaminated with cat faeces. Australian Veterinary Journal, 50, 19–21.
- Skjerve, E et al (1998). Risk factors for the presence of antibodies to Toxoplasma gondii in Norwegian slaughter lambs. Preventative Veterinary Medicine, 35, 219–227.
- Buxton, D (1990) Ovine toxoplasmosis: a review. Journal of the Royal Society of Medicine, 83, 509-511.
- Innes, E A et al (2009) Ovine toxoplasmosis. Parastiology, 136, 1887–1894.
- Buxton, D et all (2007) Toxoplasma gondii and ovine toxoplasmosis: New aspects of an old story. Veterinary Parasitology, 147, 25-28.
- Dubey, J P (2009) Toxoplasmosis in sheep — The last 20 years. Veterinary Parasitology, 163, 1-14.