Difference between revisions of "Dirofilaria immitis"
Fiorecastro (talk | contribs) |
|||
| (146 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
| + | {{unfinished}} | ||
| − | |||
| − | + | ==Description== | |
| + | [[Image:Dirofilaria immitus.jpg|thumb|right|150px|''Dirofilaria immitus'' - Courtesy of the Laboratory of Parasitology, University of Pennsylvania School of Veterinary Medicine]] | ||
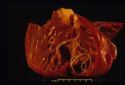
| + | [[Image:dirofilariasis.jpg|right|thumb|125px|<small><center>'''Dirofilariasis'''. Courtesy of T. Scase</center></small>]] | ||
| + | [[Image:dirofilariasis 2.jpg|right|thumb|125px|<small><center>'''Dirofilariasis'''. Courtesy of T. Scase</center></small>]] | ||
| − | + | Dirofilaria is a filarial worm. Female worms measure up to 30cm in length and males up to 15cm. The worms have a life-span of 5-7 years. Up to 250 worms may establish in the heart and [[Respiratory Parasitic Infections - Pathology#Dirofilaria immitis|pulmonary arteries]] of dogs and cats. | |
| + | Dirofilaria worms produce microfilariae, not eggs. | ||
| − | + | '''Microfilariae''': | |
| − | '' | + | *in peripheral circualtion |
| + | *periodicity - maximum numbers in blood evening/night | ||
| + | *greater than 300µm long | ||
| + | *life-span 2years | ||
| + | *present in approximately 60% of infected dogs | ||
| + | *microfilariae are absent from the circulating blood if: | ||
| + | **only immature worms present | ||
| + | **only one worm present | ||
| + | **only one sex | ||
| + | **microfilariae killed by immune response (in 15% of dogs) | ||
| + | **females sterilised by chemotherapy (e.g. ivermectin). | ||
| − | '' | + | '''Intermediate hosts''': |
| + | *many, but not all, species of mosquito. | ||
| − | + | '''Local Epidemiology''': | |
| − | '' | + | *determined by feeding preferences of local species, and population density. |
| + | *up to 45% of non-protected dogs infected in some parts of USA. | ||
| − | + | '''In mosquito''': | |
| + | *microfilariae → L1 → L2 → infective L3 | ||
| + | *this takes 1week at 30°C, or 4weeks at 18°C - there is no development below 14°C. | ||
| + | *when mosquito next feeds: | ||
| + | **L3 moves to mouthparts | ||
| + | **up to 12 L3 deposited on skin | ||
| + | **enter body via puncture wound. | ||
| − | + | '''Zoonotic hazard''': | |
| + | *human infection can occur, but few cases are diagnosed | ||
| + | *this usually happens when a radio-opaque plaque is detected in the lung, and further investigation shows it to be caused by a trapped ''D. immitis'' larva. | ||
| − | |||
| − | |||
| − | |||
| − | + | === Feline Heartworm Disease=== | |
| + | |||
| + | |||
| + | *A canine parasite - see under Dog Nematodes for life-cycle etc. | ||
| + | *Cats are abnormal hosts, and so ''D. immitis'' is not very infective for cats. | ||
| + | *Nevertheless, feline infection is common (up to 25%) in some heavily endemic areas. | ||
| + | *But only small numbers of adult worms (1-3) establish. | ||
| + | *The prepatent period is longer (approximately 8months) than in the dog. | ||
| + | *Few, if any, microfilariae are produced (<20% of cases positive). | ||
| + | *The life-span of the worm is shorter (2-3years). | ||
| + | *However: one dead adult → acute pulmonary crisis (thromboembolism). | ||
| + | *Lung pathology similar to dog, but little heart pathology. | ||
| + | *Coughing starts 4-6months post-infection. | ||
| + | *Antibody-detection ELISA used for diagnosis, but false positives occur (antigen ELISA cannot be used as antigen rarely expressed in cats). | ||
| + | *There is no licensed adulticidal therapy, and treatment may be fatal for the cat as well as the worm. | ||
| + | *Ivermectin or selamectin can be used for prevention. | ||
==Signalment== | ==Signalment== | ||
| − | |||
==Diagnosis== | ==Diagnosis== | ||
| − | |||
| − | + | '''Diagnosis''': | |
| + | *Physical examination: | ||
| + | **signs of heart disease | ||
| + | **lung involvement | ||
| + | *Radiography: | ||
| + | **enlargement of right heart, main pulmonary arteries; arteries in lung lobes with thickening and tortuosity; inflammation in surrounding tissues | ||
| + | *ECG: | ||
| + | **right axis deviation → deep S waves | ||
| + | *Echocardiography: | ||
| + | **if post caval syndrome suspected - right ventricular enlargement with worms in ventricle appearing as parallel lines. | ||
| − | + | '''Clinical pathology''': | |
| + | *needed alongside physical examination and other tests to determine treatment strategy and prognosis. | ||
| − | + | '''Parasite detection''': | |
| − | + | *methods for demonstrating microfilariae in blood: | |
| − | + | **wet blood smear (okay for quick look, but insensitive) = ''D. immitis'' not progressively motile | |
| − | + | **Knott's test = red blood cells lysed; stained sediment examined | |
| − | + | **micropore filter = blood forced through; microfilariae held on filter; stained and examined | |
| − | + | **antibody detection ELISA = not reliable in dogs, but it is the best for cats (although some false positives) | |
| − | + | **antigen detection ELISA (using specific antigen from adult female worm) = reliable positives from 5-7months post-infection in dogs; although occasional false negatives occur → '''not''' useful for cats | |
| − | * | + | *the immunochromatographic test (ICT) uses coloured gold colloidal particles tagged to monoclonal antibodies to visualise the presence of adult worm antigen - performance similar to antigen detection ELISA, but quicker and easier to do (but not as quantitative as some ELISAs are) |
| − | + | *operator error can give false positives, therefore best to confirm result with another test. | |
| − | |||
| − | |||
| − | |||
| − | * | ||
| − | * | ||
| − | * | ||
| − | * | ||
| − | |||
| − | |||
| − | |||
| − | * | ||
| − | * | ||
| − | * | ||
| − | |||
| − | |||
| − | |||
| − | * | ||
| − | * | ||
| − | |||
| − | |||
| − | ''' | + | ===Clinical Signs=== |
| + | '''Clinical signs''': | ||
| + | *often sudden onset severe lethargy and weakness, but: | ||
| + | *signs variable, reflecting multiple system dysfunction - pulmonary circulation, heart, liver and kidneys: | ||
| + | **lung damage (severe pulmonary hypertension; thromboembolism) | ||
| + | **heart failure (right-sided congestive) | ||
| + | *therefore, '''not''' pathognomonic | ||
| + | *acute prepatent = coughing | ||
| + | *chronic = exercise intolerance, sometimes with ascites | ||
| + | *acute post caval syndrome = collapse (dyspnoea, pale mucous membranes or jaundice, haemoglobinuria) | ||
| − | + | ===Diagnostic Imaging=== | |
| − | === | + | ===Laboratory Tests=== |
| − | |||
| − | + | ===Pathology=== | |
| + | '''Worms produce''': | ||
| + | *substances that are: | ||
| + | **antigenic | ||
| + | **immunomodulatory | ||
| + | **pharmacologically active. | ||
| − | + | '''Lesions are''': | |
| − | + | *'''not''' confined to the location of the worms | |
| + | *also caused by shear stress of high blood flow. | ||
| − | + | '''Severity''': | |
| + | *not associated with the number of worms | ||
| + | *exacerbated by exercise (i.e. by high blood flow rate) | ||
| + | *sedentary dogs often asymptomatic - symptoms most commonly associated with racing greyhounds. | ||
| − | + | '''Acute prepatent disease''': | |
| − | + | *immature adult worms in caudal distal pulmonary arteries | |
| + | *leads to intense diffuse eosinophilic reaction, which in turn leads to coughing. | ||
| − | + | '''Chronic disease''': | |
| + | *mature worms in right heart and pulmonary arteries | ||
| + | *endothelial swelling and sloughing | ||
| + | *increased permeability → inflammation → periarteritis | ||
| + | *platelets/white blood cells activated → thrombosis | ||
| + | *proliferation of smooth muscle, thickening of media: | ||
| − | + | → impairment of blood flow | |
| − | |||
| − | + | → pulmonary hypertension | |
| − | |||
| − | |||
| − | |||
| − | + | → right ventricular strain | |
| − | + | → right ventricular hypertrophy and right-sided heart failure | |
| + | *insufficient blood pumped through pulmonary capillary bed → insufficient preload for left ventricle. | ||
| − | + | '''Post Caval Syndrome (Dirofilarial haemoglobinuria)''': | |
| + | *can be acute or chronic | ||
| + | *heavy heartworm infestation: | ||
| + | **entangled clumps of worms → impaired closure of tricuspid valve → post-caval stagnation → hepatic congestion and hepatic failure | ||
| + | *this is accompanied by increased red blood cell fragility, haemolytic anaemia and haemolobinuria. | ||
==Treatment== | ==Treatment== | ||
| − | + | '''Chemotherapy''': | |
| + | *three treatment objectives needing different approaches: | ||
| − | + | 1) '''Adulticidal''' | |
| + | *risk that dead worms → thromboembolism → respiratory failure | ||
| + | *therefore, hospitalise and strict exercise restriction for at least 3weeks post-treatment | ||
| + | *organic arsenicals for adulticidal therapy: | ||
| + | **'''Thiacetarsamide''' (2.2mg/kg IV bid for 2days) - hepatotoxic; skin sloughing | ||
| + | **'''Melarsomine''' (2.5mg/kg IM sid for 2days) - generally safer, but greater risk of thromboembolism | ||
| − | + | NB - Ivermectin preventative doses over 16months reduces adult worm numbers | |
| − | + | 2) '''Microfilaricidal''' | |
| + | *start 3-6weeks after adulticidal therapy: | ||
| + | **'''Ivermectin''' (50µg/kg) | ||
| + | **'''Milbemycin oxime''' (0.5mg/kg) | ||
| + | NB - risk of reaction to dead microfilariae in sensitised animals (lethargy, retching, tachycardia, circulatory collapse) - observe for 8hours post-treatment | ||
| − | + | 3) '''Preventative (prophylactic)''' | |
| + | *objective = kill migrating L4 before they reach the heart | ||
| + | *monthly treatments are 100% effective and safe if used properly, but often fail because of inadequate owner compliance | ||
| + | *test for adult infection/microfilarie before start and annually thereafter: | ||
| + | **'''Ivermectin''' (6µg/kg monthly) - blocks maturation of larvae; these die only after several months | ||
| + | **'''Selamectin''' (6mg/kg monthly) | ||
| + | **'''Moxidectin''' (injectable formulation - 0.17mg/kg gives 6months protection) | ||
| + | **'''Milbemycin oxime''' (0.5mg/kg monthly) - care → kills microfilarie, therefore risk of reaction | ||
| + | **'''DEC (diethylcarbamazine)''' daily - care → kills microfilarie, therefore severe risk of reaction | ||
| − | ''' | + | '''Treatment of Post Caval Syndrome''': |
| − | + | *surgical removal with forceps via jugular vein | |
| − | + | *usually very successful, but: | |
| + | *do not crush or fragment worms | ||
| − | + | → massive release of antigen | |
| + | |||
| + | → cardiac failure and acute respiratory distress | ||
| − | + | → rapid death | |
| − | + | '''A typical therapy protocol''': | |
| − | |||
| − | |||
| − | + | 1) Pre-treatment evaluation | |
| − | + | 2) Adulticide: 4-6weeks restricted exercise | |
| − | + | 3) Microfilaricide: 3weeks after adulticide | |
| − | + | 4) Initiation of monthly preventative treatments | |
| − | |||
| + | 5) Check for microfilariae after 2weeks | ||
| − | + | 6) Check for adults (ELISA) 4-6months after adulticide, and before start of each subsequent mosquito season. | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| + | ==Prognosis== | ||
==Links== | ==Links== | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==References== | ==References== | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
[[Category:Filarioidea]] | [[Category:Filarioidea]] | ||
[[Category:Dog_Nematodes]] | [[Category:Dog_Nematodes]] | ||
[[Category:Cat_Nematodes]] | [[Category:Cat_Nematodes]] | ||
| − | [[Category: | + | [[Category:To_Do_-_Parasites]] |
| − | + | ||
| − | + | ||
[[Category:Respiratory Parasitic Infections]] | [[Category:Respiratory Parasitic Infections]] | ||
| − | + | [[Category:To_Do_-_Lizzie]] | |
| − | [[Category: | ||
| − | |||
Revision as of 18:07, 25 August 2010
| This article is still under construction. |
Description
Dirofilaria is a filarial worm. Female worms measure up to 30cm in length and males up to 15cm. The worms have a life-span of 5-7 years. Up to 250 worms may establish in the heart and pulmonary arteries of dogs and cats. Dirofilaria worms produce microfilariae, not eggs.
Microfilariae:
- in peripheral circualtion
- periodicity - maximum numbers in blood evening/night
- greater than 300µm long
- life-span 2years
- present in approximately 60% of infected dogs
- microfilariae are absent from the circulating blood if:
- only immature worms present
- only one worm present
- only one sex
- microfilariae killed by immune response (in 15% of dogs)
- females sterilised by chemotherapy (e.g. ivermectin).
Intermediate hosts:
- many, but not all, species of mosquito.
Local Epidemiology:
- determined by feeding preferences of local species, and population density.
- up to 45% of non-protected dogs infected in some parts of USA.
In mosquito:
- microfilariae → L1 → L2 → infective L3
- this takes 1week at 30°C, or 4weeks at 18°C - there is no development below 14°C.
- when mosquito next feeds:
- L3 moves to mouthparts
- up to 12 L3 deposited on skin
- enter body via puncture wound.
Zoonotic hazard:
- human infection can occur, but few cases are diagnosed
- this usually happens when a radio-opaque plaque is detected in the lung, and further investigation shows it to be caused by a trapped D. immitis larva.
Feline Heartworm Disease
- A canine parasite - see under Dog Nematodes for life-cycle etc.
- Cats are abnormal hosts, and so D. immitis is not very infective for cats.
- Nevertheless, feline infection is common (up to 25%) in some heavily endemic areas.
- But only small numbers of adult worms (1-3) establish.
- The prepatent period is longer (approximately 8months) than in the dog.
- Few, if any, microfilariae are produced (<20% of cases positive).
- The life-span of the worm is shorter (2-3years).
- However: one dead adult → acute pulmonary crisis (thromboembolism).
- Lung pathology similar to dog, but little heart pathology.
- Coughing starts 4-6months post-infection.
- Antibody-detection ELISA used for diagnosis, but false positives occur (antigen ELISA cannot be used as antigen rarely expressed in cats).
- There is no licensed adulticidal therapy, and treatment may be fatal for the cat as well as the worm.
- Ivermectin or selamectin can be used for prevention.
Signalment
Diagnosis
Diagnosis:
- Physical examination:
- signs of heart disease
- lung involvement
- Radiography:
- enlargement of right heart, main pulmonary arteries; arteries in lung lobes with thickening and tortuosity; inflammation in surrounding tissues
- ECG:
- right axis deviation → deep S waves
- Echocardiography:
- if post caval syndrome suspected - right ventricular enlargement with worms in ventricle appearing as parallel lines.
Clinical pathology:
- needed alongside physical examination and other tests to determine treatment strategy and prognosis.
Parasite detection:
- methods for demonstrating microfilariae in blood:
- wet blood smear (okay for quick look, but insensitive) = D. immitis not progressively motile
- Knott's test = red blood cells lysed; stained sediment examined
- micropore filter = blood forced through; microfilariae held on filter; stained and examined
- antibody detection ELISA = not reliable in dogs, but it is the best for cats (although some false positives)
- antigen detection ELISA (using specific antigen from adult female worm) = reliable positives from 5-7months post-infection in dogs; although occasional false negatives occur → not useful for cats
- the immunochromatographic test (ICT) uses coloured gold colloidal particles tagged to monoclonal antibodies to visualise the presence of adult worm antigen - performance similar to antigen detection ELISA, but quicker and easier to do (but not as quantitative as some ELISAs are)
- operator error can give false positives, therefore best to confirm result with another test.
Clinical Signs
Clinical signs:
- often sudden onset severe lethargy and weakness, but:
- signs variable, reflecting multiple system dysfunction - pulmonary circulation, heart, liver and kidneys:
- lung damage (severe pulmonary hypertension; thromboembolism)
- heart failure (right-sided congestive)
- therefore, not pathognomonic
- acute prepatent = coughing
- chronic = exercise intolerance, sometimes with ascites
- acute post caval syndrome = collapse (dyspnoea, pale mucous membranes or jaundice, haemoglobinuria)
Diagnostic Imaging
Laboratory Tests
Pathology
Worms produce:
- substances that are:
- antigenic
- immunomodulatory
- pharmacologically active.
Lesions are:
- not confined to the location of the worms
- also caused by shear stress of high blood flow.
Severity:
- not associated with the number of worms
- exacerbated by exercise (i.e. by high blood flow rate)
- sedentary dogs often asymptomatic - symptoms most commonly associated with racing greyhounds.
Acute prepatent disease:
- immature adult worms in caudal distal pulmonary arteries
- leads to intense diffuse eosinophilic reaction, which in turn leads to coughing.
Chronic disease:
- mature worms in right heart and pulmonary arteries
- endothelial swelling and sloughing
- increased permeability → inflammation → periarteritis
- platelets/white blood cells activated → thrombosis
- proliferation of smooth muscle, thickening of media:
→ impairment of blood flow
→ pulmonary hypertension
→ right ventricular strain
→ right ventricular hypertrophy and right-sided heart failure
- insufficient blood pumped through pulmonary capillary bed → insufficient preload for left ventricle.
Post Caval Syndrome (Dirofilarial haemoglobinuria):
- can be acute or chronic
- heavy heartworm infestation:
- entangled clumps of worms → impaired closure of tricuspid valve → post-caval stagnation → hepatic congestion and hepatic failure
- this is accompanied by increased red blood cell fragility, haemolytic anaemia and haemolobinuria.
Treatment
Chemotherapy:
- three treatment objectives needing different approaches:
1) Adulticidal
- risk that dead worms → thromboembolism → respiratory failure
- therefore, hospitalise and strict exercise restriction for at least 3weeks post-treatment
- organic arsenicals for adulticidal therapy:
- Thiacetarsamide (2.2mg/kg IV bid for 2days) - hepatotoxic; skin sloughing
- Melarsomine (2.5mg/kg IM sid for 2days) - generally safer, but greater risk of thromboembolism
NB - Ivermectin preventative doses over 16months reduces adult worm numbers
2) Microfilaricidal
- start 3-6weeks after adulticidal therapy:
- Ivermectin (50µg/kg)
- Milbemycin oxime (0.5mg/kg)
NB - risk of reaction to dead microfilariae in sensitised animals (lethargy, retching, tachycardia, circulatory collapse) - observe for 8hours post-treatment
3) Preventative (prophylactic)
- objective = kill migrating L4 before they reach the heart
- monthly treatments are 100% effective and safe if used properly, but often fail because of inadequate owner compliance
- test for adult infection/microfilarie before start and annually thereafter:
- Ivermectin (6µg/kg monthly) - blocks maturation of larvae; these die only after several months
- Selamectin (6mg/kg monthly)
- Moxidectin (injectable formulation - 0.17mg/kg gives 6months protection)
- Milbemycin oxime (0.5mg/kg monthly) - care → kills microfilarie, therefore risk of reaction
- DEC (diethylcarbamazine) daily - care → kills microfilarie, therefore severe risk of reaction
Treatment of Post Caval Syndrome:
- surgical removal with forceps via jugular vein
- usually very successful, but:
- do not crush or fragment worms
→ massive release of antigen
→ cardiac failure and acute respiratory distress
→ rapid death
A typical therapy protocol:
1) Pre-treatment evaluation
2) Adulticide: 4-6weeks restricted exercise
3) Microfilaricide: 3weeks after adulticide
4) Initiation of monthly preventative treatments
5) Check for microfilariae after 2weeks
6) Check for adults (ELISA) 4-6months after adulticide, and before start of each subsequent mosquito season.