Difference between revisions of "Coagulation Tests"
| Line 11: | Line 11: | ||
===Disorders of Haemostasis=== | ===Disorders of Haemostasis=== | ||
| − | + | Abnormalities can develop in any of the components of haemostasis. Disorders of primary haemostasis include vessel defects (i.e. vasculitis), thrombocytopenia (due to decreased production or increased destruction) and abnormalities in platelet function (e.g. congenital defects, disseminated intravascular coagulation). These lead to the occurence of multiple minor bleeds and prolonged bleeding. For example, petechial or ecchymotic haemorrhages may be seen on the skin and mucous membranes, or ocular bleeds may arise. Generally, intact secondary haemostasis prevents major haemorrhage in disorders of primary haemostasis . | |
| − | + | When secondary haemostasis is abnormal, larger bleeds are frequently seen. Haemothroax, haemoperitoneum, or haemoarthrosis may occur, in addition to subcutaneous and intramuscular haemorrhages. Petechia and ecchymoses are not usually apparent, as intact primary haemostasis prevents minor capillary bleeding. | |
| − | |||
| − | |||
disroders of fibrinolysis may result in thrombus formation and loss of blood supply. The fomation of thrombi is promoted by: local endothelial injury (vascular damage), circulatory stasis and changed in anticoagulants or procoagulants, e.g. decreased ATIII. The most common mechanisms for AT deficiency are glomerular disease (AT is similar in size to albumin and is thus lost via the urine in glomerular diseasesP and accelarated consumption which occurs with disseminated intravascular coagulation or sepsis. | disroders of fibrinolysis may result in thrombus formation and loss of blood supply. The fomation of thrombi is promoted by: local endothelial injury (vascular damage), circulatory stasis and changed in anticoagulants or procoagulants, e.g. decreased ATIII. The most common mechanisms for AT deficiency are glomerular disease (AT is similar in size to albumin and is thus lost via the urine in glomerular diseasesP and accelarated consumption which occurs with disseminated intravascular coagulation or sepsis. | ||
Revision as of 11:11, 25 August 2010
Introduction
Haemostasis
Normally, haemostastis is maintained by three key events. The first stage, primary haemostasis, involves platelets and the blood vessels themselves. It is triggered by injury to a vessel, and platelets become activated, adhere to endothelial connective tissue and aggregate with other platelets. A fragile plug is thus formed which helps to stem haemorrhage from the vessel. Substances are released from platelets during primary haemostasis. Vasoactive compounds give vasoconstriction, and other mediators cause continued platelet activation and aggregation, as well as contraction of the platelet plug. Primary haemostasis ceases once defects in the vessels are sealed and bleeding stops.
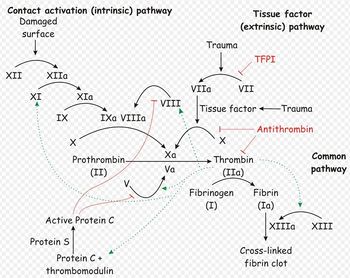
The platelet plug formed by primary haemostasis is fragile and must be reinforced in order to provide longer-term benefit. In secondary haemostasis, proteinaceous clotting factors interact in a cascade to produce fibrin to reinforce the clot. Two arms of the cascade are activated simultaneously to achieve coagulation: the intrinsic and extrinsic pathways. The intrinsic pathway is activated by contact with collagen due to vessel injury and involves the clotting factors XII, XI, IX and VIII. The extrinsic pathway is triggered by tissue injury and is effected via factor VII. These pathways progress independently before converging at the common pathway, which involves the factors X, V, II and I and ultimately results in the formation of fibrin from fibrinogen. Factors I, VII, IX and X are dependent upon vitamin K to become active.
The end product of haemostasis is a solid clot of fused platelets enclosed in a mesh of fibrin strands. It is important that uncontrolled, widespread clot formation is prevented, and so a fibrinolytic system exists to breakdown fibrin within blood clots. The two most important anticoagulants involved in fibrinolysis are antithrombin III (ATIII) and Protein C. The end products of fibinolysis are fibrin degratation products (FDPs).
Disorders of Haemostasis
Abnormalities can develop in any of the components of haemostasis. Disorders of primary haemostasis include vessel defects (i.e. vasculitis), thrombocytopenia (due to decreased production or increased destruction) and abnormalities in platelet function (e.g. congenital defects, disseminated intravascular coagulation). These lead to the occurence of multiple minor bleeds and prolonged bleeding. For example, petechial or ecchymotic haemorrhages may be seen on the skin and mucous membranes, or ocular bleeds may arise. Generally, intact secondary haemostasis prevents major haemorrhage in disorders of primary haemostasis .
When secondary haemostasis is abnormal, larger bleeds are frequently seen. Haemothroax, haemoperitoneum, or haemoarthrosis may occur, in addition to subcutaneous and intramuscular haemorrhages. Petechia and ecchymoses are not usually apparent, as intact primary haemostasis prevents minor capillary bleeding.
disroders of fibrinolysis may result in thrombus formation and loss of blood supply. The fomation of thrombi is promoted by: local endothelial injury (vascular damage), circulatory stasis and changed in anticoagulants or procoagulants, e.g. decreased ATIII. The most common mechanisms for AT deficiency are glomerular disease (AT is similar in size to albumin and is thus lost via the urine in glomerular diseasesP and accelarated consumption which occurs with disseminated intravascular coagulation or sepsis.
Tests Evaluating Primary Haemostasis
Platelet Number
BMBT
Tests Evaluating Secondary Haemostasis
ACT
PT
(A)PTT
Definition
The aPTT measures the time necessary to generate fibrin from initiation of the intrinsic pathway (Figure 157.1). Activation of factor XII is accomplished with an external agent (e.g., kaolin) capable of activating factor XII without activating factor VII. Since platelet factors are necessary for the cascade to function normally, the test is performed in the presence of a phospholipid emulsion that takes the place of these factors. The classic partial thromboplastin time depends on contact with a glass tube for activation. Since this is considered a difficult variable to control, the "activated" test uses an external source of activation. Technique
Citrated plasma, an activating agent, and phospholipid are added together and incubated at 37°C. Calcium is added, and the time necessary for the clumping of kaolin is measured. The normal time is usually reported as less than 30 to 35 seconds depending on the technique used. In fact, there is a normal range of about 10 seconds (e.g., 25 to 35), and decreased values ("short") may also be abnormal. Basic Science
This test is abnormal in the presence of reduced quantities of factors XII, IX, XI, VIII, X, V, prothrombin, and fibrinogen (all integral parts of the "intrinsic" and "common" pathway. It is usually prolonged if a patient has less than approximately 30% normal activity. It can also be abnormal in the presence of a circulating inhibitor to any of the intrinsic pathway factors. The differentiation of inhibitors from factor depletion is important and can best be accomplished by a mixing study in which patient and normal plasma are combined in a 1:1 ratio and the test is repeated on the mixed sample. If the abnormal value is corrected completely, the problem is factor deficiency. If the result does not change or the abnormality is corrected only partially, an inhibitor is present. This difference stems from the above mentioned fact that the aPTT will be normal in the presence of 50% normal activity. Clinical Significance
The aPTT is a good screening test for inherited or acquired factor deficiencies. Inherited disorders including classic hemophilia A (factor VIII deficiency) and hemophilia B (factor IX deficiency, or Christmas disease) are well-known diseases in which the aPTT is prolonged. Other intrinsic and common pathway factors may also be congenitally absent. These conditions are rare but have been described for all factors. A number of kindreds with abnormalities of factor XII activation have been described. They are usually associated with a prolonged aPTT without clinical signs of bleeding. Acquired factor deficiency is common. Vitamin K deficiency, liver dysfunction, and iatrogenic anticoagulation with warfarin are most common. Factor depletion may also occur in the setting of disseminated intravascular coagulation (DIC), prolonged bleeding, and massive transfusion.
A prolonged aPTT that cannot be completely normalized with the addition of normal plasma can be explained only by the presence of a circulating inhibitor of coagulation. The presence of these inhibitors is almost always acquired, and their exact nature is not always apparent. From a clinical point of view, the most common inhibitors should be considered antithrombins. These compounds inhibit the activity of thrombin on the conversion of fibrinogen to fibrin (Figure 157.1). The two most common inhibitors are heparin, which acts through the naturally occurring protein antithrombin III (AT III), and fibrin degradation products (FDP), formed by the action of plasmin on the fibrin clot and usually present in elevated concentrations in DIC and primary fibrinolysis.
Other inhibitors appear to be antibodies. The easiest to understand is the antibody against factor VIII in patients with hemophilia A treated with factor VIII concentrate. Inhibitors against other factors have been described with a variety of diseases that follow a variable course. When characterized, they have been immunoglobulins.
A particular problem may be seen in patients suffering from systemic lupus erythematosus. These patients may present with a prolonged aPTT without evidence of bleeding. Some present with thrombosis. The abnormality cannot be corrected with normal plasma and has been referred to as the "lupus anticoagulant." This phenomenon does not represent an in vivo problem with the coagulation cascade. Rather, it is a laboratory abnormality caused by the presence of a serum constituent that interferes with the in vitro partial thromboplastin test.
Occasionally the reported value of the aPTT will be lower than normal. This "shortened" time may reflect the presence of increased levels of activated factors in context of a "hypercoagulable state." It is seen in some patients in the early stages of DIC but should not be considered diagnostic for that entity.