Dirofilaria immitis
| This article is still under construction. |
- May cause muscle ischaemia in dogs due to arteritis and thrombosis of external iliac arteries and their branches
- Dirofilaria immitis live in heart and pulmonary arteries of dogs and cats
Nematodes of Dogs - CANINE HEARTWORM
- Dirofilaria immitis is one of the most important causes of morbidity and mortality in dogs in many regions of the world that have a warm, humid climate, including parts of southern Europe, USA and Australia.
- The presenting signs are usually those of heart failure, but sudden collapse may occur in heavily infected dogs.
- The endemic zone for canine heartworm disease is spreading as people increasingly travel with their pets.
- Strains of D. immitis are adapting to cooler climates.
- It is not endemic in the UK, but more infected dogs are likely to be imported now that the quarantine regulations have been relaxed.
- It has a very long prepatent period, so clinical signs may not appear for many months after importation.
- Although primarily a canine parasite, cats and ferrets can become infected.
- Owners taking their pets into endemic regions require advice on how the disease can be prevented.
Dirofilaria immitis:
- a filarial worm
- females: up to 30cm long; males: up to 15cm long
- life-span 5-7years
- up to 250 worms may establish in the heart and pulmonary arteries
- produce microfilariae, not eggs.
Microfilariae:
- in peripheral circualtion
- periodicity - maximum numbers in blood evening/night
- greater than 300µm long
- life-span 2years
- present in approximately 60% of infected dogs
- microfilariae are absent from the circulating blood if:
- only immature worms present
- only one worm present
- only one sex
- microfilariae killed by immune response (in 15% of dogs)
- females sterilised by chemotherapy (e.g. ivermectin).
Intermediate hosts:
- many, but not all, species of mosquito.
Local Epidemiology:
- determined by feeding preferences of local species, and population density.
- up to 45% of non-protected dogs infected in some parts of USA.
In mosquito:
- microfilariae → L1 → L2 → infective L3
- this takes 1week at 30°C, or 4weeks at 18°C - there is no development below 14°C.
- when mosquito next feeds:
- L3 moves to mouthparts
- up to 12 L3 deposited on skin
- enter body via puncture wound.
In dog:
- larvae migrate through connective tissues and moult twice
- immature adults (L5) are 1-5cm long → caudal distal pulmonary arteries in 4months → diffuse eosinophilic reaction in lung parenchyma, then migrate back towards right ventricle
- start producing microfilariae 6-7months post-infection.
Zoonotic hazard:
- human infection can occur, but few cases are diagnosed
- this usually happens when a radio-opaque plaque is detected in the lung, and further investigation shows it to be caused by a trapped D. immitis larva.
Pathology
Worms produce:
- substances that are:
- antigenic
- immunomodulatory
- pharmacologically active.
Lesions are:
- not confined to the location of the worms
- also caused by shear stress of high blood flow.
Severity:
- not associated with the number of worms
- exacerbated by exercise (i.e. by high blood flow rate)
- sedentary dogs often asymptomatic - symptoms most commonly associated with racing greyhounds.
Acute prepatent disease:
- immature adult worms in caudal distal pulmonary arteries
- leads to intense diffuse eosinophilic reaction, which in turn leads to coughing.
Chronic disease:
- mature worms in right heart and pulmonary arteries
- endothelial swelling and sloughing
- increased permeability → inflammation → periarteritis
- platelets/white blood cells activated → thrombosis
- proliferation of smooth muscle, thickening of media:
→ impairment of blood flow
→ pulmonary hypertension
→ right ventricular strain
→ right ventricular hypertrophy and right-sided heart failure
- insufficient blood pumped through pulmonary capillary bed → insufficient preload for left ventricle.
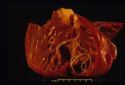
Post Caval Syndrome (Dirofilarial haemoglobinuria):
- can be acute or chronic
- heavy heartworm infestation:
- entangled clumps of worms → impaired closure of tricuspid valve → post-caval stagnation → hepatic congestion and hepatic failure
- this is accompanied by increased red blood cell fragility, haemolytic anaemia and haemolobinuria.
Clinical signs:
- often sudden onset severe lethargy and weakness, but:
- signs variable, reflecting multiple system dysfunction - pulmonary circulation, heart, liver and kidneys:
- lung damage (severe pulmonary hypertension; thromboembolism)
- heart failure (right-sided congestive)
- therefore, not pathognomonic
- acute prepatent = coughing
- chronic = exercise intolerance, sometimes with ascites
- acute post caval syndrome = collapse (dyspnoea, pale mucous membranes or jaundice, haemoglobinuria)
Diagnosis:
- Physical examination:
- signs of heart disease
- lung involvement
- Radiography:
- enlargement of right heart, main pulmonary arteries; arteries in lung lobes with thickening and tortuosity; inflammation in surrounding tissues
- ECG:
- right axis deviation → deep S waves
- Echocardiography:
- if post caval syndrome suspected - right ventricular enlargement with worms in ventricle appearing as parallel lines.
Clinical pathology:
- needed alongside physical examination and other tests to determine treatment strategy and prognosis.
Parasite detection:
- methods for demonstrating microfilariae in blood:
- wet blood smear (okay for quick look, but insensitive) = D. immitis not progressively motile
- Knott's test = red blood cells lysed; stained sediment examined
- micropore filter = blood forced through; microfilariae held on filter; stained and examined
- antibody detection ELISA = not reliable in dogs, but it is the best for cats (although some false positives)
- antigen detection ELISA (using specific antigen from adult female worm) = reliable positives from 5-7months post-infection in dogs; although occasional false negatives occur → not useful for cats
- the immunochromatographic test (ICT) uses coloured gold colloidal particles tagged to monoclonal antibodies to visualise the presence of adult worm antigen - performance similar to antigen detection ELISA, but quicker and easier to do (but not as quantitative as some ELISAs are)
- operator error can give false positives, therefore best to confirm result with another test.
Chemotherapy:
- three treatment objectives needing different approaches:
1) Adulticidal
- risk that dead worms → thromboembolism → respiratory failure
- therefore, hospitalise and strict exercise restriction for at least 3weeks post-treatment
- organic arsenicals for adulticidal therapy:
- Thiacetarsamide (2.2mg/kg IV bid for 2days) - hepatotoxic; skin sloughing
- Melarsomine (2.5mg/kg IM sid for 2days) - generally safer, but greater risk of thromboembolism
NB - Ivermectin preventative doses over 16months reduces adult worm numbers
2) Microfilaricidal
- start 3-6weeks after adulticidal therapy:
- Ivermectin (50µg/kg)
- Milbemycin oxime (0.5mg/kg)
NB - risk of reaction to dead microfilariae in sensitised animals (lethargy, retching, tachycardia, circulatory collapse) - observe for 8hours post-treatment
3) Preventative (prophylactic)
- objective = kill migrating L4 before they reach the heart
- monthly treatments are 100% effective and safe if used properly, but often fail because of inadequate owner compliance
- test for adult infection/microfilarie before start and annually thereafter:
- Ivermectin (6µg/kg monthly) - blocks maturation of larvae; these die only after several months
- Selamectin (6mg/kg monthly)
- Moxidectin (injectable formulation - 0.17mg/kg gives 6months protection)
- Milbemycin oxime (0.5mg/kg monthly) - care → kills microfilarie, therefore risk of reaction
- DEC (diethylcarbamazine) daily - care → kills microfilarie, therefore severe risk of reaction
Treatment of Post Caval Syndrome:
- surgical removal with forceps via jugular vein
- usually very successful, but:
- do not crush or fragment worms
→ massive release of antigen
→ cardiac failure and acute respiratory distress
→ rapid death
A typical therapy protocol:
1) Pre-treatment evaluation
2) Adulticide: 4-6weeks restricted exercise
3) Microfilaricide: 3weeks after adulticide
4) Initiation of monthly preventative treatments
5) Check for microfilariae after 2weeks
6) Check for adults (ELISA) 4-6months after adulticide, and before start of each subsequent mosquito season.