Neutrophils
|
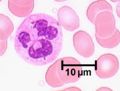
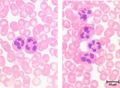
Neutrophils represent up to half of all leukocytes in the blood stream and are distinguished by their irregular multi-lobed nucleus and indistinct granular appearance. They are 10-12µm and circulate in the blood for minutes to hours (average 6-8 hours) and lasting for 1-2 days in tissue. Although the most abundant leukocyte in the blood the vast majority of neutrophils are found in the bone marrow (5x more). Neutrophils play a key role during bacterial infections and have both phagocytic and killing actions.
Neutrophils are called heterophils in birds, reptiles and some mammals.
Development
The neutrophil is a granulocyte and has a similar development to the other granulocytes. This process is called granulopoiesis and further details can be found here.
Granules
Three types of granules are present in neutrophils:
- Primary granules (azurophilic) are present in all granulocytes and contain myeloperoxidase which creates anti-bacterial compounds, acid hydrolases and defensins.
- Secondary granules (specific) are the most numerous type and contain complement activators and enzymes e.g. collagenases.
- Finally tertiary granules are either phosphatases or metalloproteinases with the later aiding movement through connective tissue.
Movement
Neutrophils are extremely motile and express a number of adhesion molecules on their surface which allows them to attach to the walls of capillaries.
Selection molecules expressed on the surface of neutrophil bind to receptors on the capillary endothelium causing a loose attachment. This allows the neutrophil to “roll” along the surface of capillaries. Stimulation by chemokines causes further attachment between the neutrophils intergrin molecules and associated receptors on the endothelium. Finally signalling molecules such as TNF and Il-1 cause the expression of ICAM-1 (inter-cellular adhesion molecule-1) and VCAM-1 (Vascular Cell adhesion molecule) on the neutrophil which causes firm attachment.
The neutrophil then exhibits amoeboid movement and can pass through holes in the capillary wall that are smaller than themselves (diapedesis). This is achieved by extending a small part of the cell (a pseudopodium) through the capillary. The rest of the neutrophils cytoplasm and contents then passes through. This process is assisted by the release of histamine and other vasodilators by other inflammatory cells.
Once within the tissue neutrophils respond to chemotactic substances such as cytokines or bacterial products. These attract the neutrophil to the area of damage/ infection. This process is called chemotaxis. Once neutrophils have entered tissue they do not return to the blood stream.
Actions
Neutrophils are the first inflammatory cells to enter damaged tissue from the blood after tissue damage has being caused. They are the predominant cell at 4 - 6 hours after the beginning of the inflammatory reaction, at 12 hours there are also substantial numbers of macrophages and at 24 hours there are as many neutrophils as macrophages.
Phagocytosis
The main role of the neutrophil is to engulf and destroy foreign material. They uptake this material via endocytosis and this surrounds the material in the neutrophil membrane forming a phagosome. Lysosomes inside the neutrophil then fuse with the phagosome and release their contents degrading the foreign material. Phagocytosing material shortens the lifespan of the neutrophil due to the build up of toxins both from the degraded bacteria etc. and also from its own lysosomes contents. Most neutrophils die after phagocytosing 5-25 bacteria and the dead neutrophils form pus.
Neutrophils do not always destroy engulfed particles and may transport engulfed particles to local lymph nodes to be dealt with by other host defence mechanisms. This means that acute inflammation in tissue is can be accompanied by similar acute inflammation in the lymph nodes.
Recognition
To function correctly neutrophils need to correctly identify material that is either foreign (non-self) or requires removal, such as damaged cells. They are able to recognise some foreign material directly but in other circumstances proteins (opsonins) that bind to bacteria and increase binding of the foreign material to the neutrophil.
Killing
This is either by oxygen dependant pathways of oxygen independent pathways.
Oxygen dependant killing requires the productions of reactive oxygen species that damage bacterial membranes. These species are generated during a burst of respiration following phagocytosis were increased amount of oxygen are used. Hydrochloric acid is also produced during this process.
Oxygen independent killing uses lysosomes, cathepsin (a protease) and other mechanisms. Lysozymes are particularly effective against gram positive bacteria as they hydrolyse the glycopeptides coats of the bacteria.
Interactions
Il-6, Il-8 and C5a are all chemoattractants for neutrophils.
In pathology
- Classically a cell involved in acute inflammation
- Liquefactive necrosis in the formation of pus
- Are pyrogenic (fever producing)
- Neutrophilia/Neutopenia