Equine Protozoal Myeloencephalitis
| This article is still under construction. |
| Also known as: | EPM Equine protozoal myelitis |
Description
A progressive, infectious,[1]neurological disease of horses, endemic in the USA[2] and only encountered elsewhere in imported equids.[3] EPM is one of the most frequently diagnosed neurological conditions of the Western Hemisphere[4] and the principal differential for multifocal, asymmetric progressive central nervous system (CNS) disease.[1] As it can resemble any neurological disorder, EPM must be considered in any horse with neurological signs if it resides in the Americas or if it has been imported from that area[2][5] The disease is not contagious.[1]
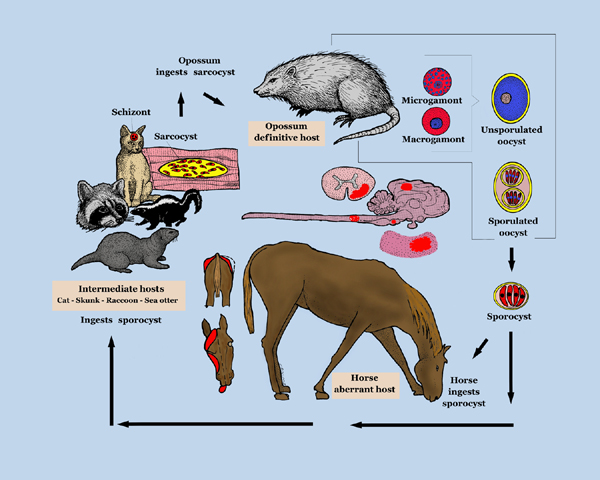
Aetiology
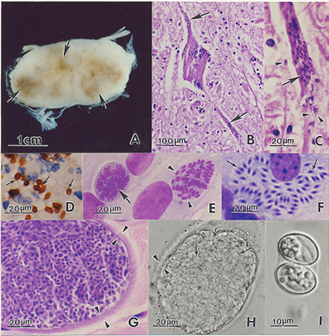
EPM results from infection of the CNS by the apicomplexan parasite Sarcocystis neurona or, less frequently, its close relative Neospora hughesi.[6][7] These protozoans develop within neurons[4] causing immediate or inflammatory-mediated neuronal damage. The organisms migrate randomly through the brain and spinal cord causing asymmetrical lesions of grey and white matter and thus multifocal lower and upper motor neuron deficits.[1]
Signalment
Mostly Standardbreds and Thoroughbreds aged 1-6years.[1] Foal infection may be possible.[2]
Differential Diagnoses
| cellpadding="10" cellspacing="0" border="1" | Differential | Differentiating signs | Tests to rule out |- | | | |- | | | |- | | | |- | | | |- | | | |- | | | |- | | | |- | | | |-
The disease may mimic almost any neurological disease because the parasite can localise in any region of the central nervous system (CNS).(EPM 8) Includes virtually all diseases of the CNS (Furr)
Cervical vertebral malformation (CVM, cervical compressive myeolpathy, Wobblers) (but symmetrical gait deficits, worse in pelvic limbs (3 in Hahn p603) with spasticity and dysmetria, good retention of strength, no muscle wasting (Furr)), standing plain lateral rads of C1 to T1 (Hahn in Furr), can be concurrent with EPM (Hahn) Infectious diseases of the CNS (systemically ill, pyrexia and changes in leukogram) WNV encephalitis - CSF abnormal, difficult if horse not febrile and no excessive muscle fasciculations, IgM capture ELISA EEE - CSF abnormal, abnormal motor function (Long), rapidly progressive (seino, p134) WEE – abnormal motor function (Long) VEE – IgM capture ELISA (Bertone) Equine herpesvirus-1 myeloencephalopathy – sudden onset and early stabilization of neuro signs, multiple horses affected, recent fever, abortion (14 in Wilson and Pusterla p615) dysuria not often seen in EPM , PCR (Furr) Rabies – rapid progression (Sommardahl), behavioural alterations, depression, seizure, coma (Long), post-mortem dx (Sommardahl) Multifocal disease, ataxia and muscle atrophy also found with: Polyneuritis equi – cranial nerve deficits peripheral with no change in attitude (6 p623 in Saville), differentiate by Western blot analysis of CSF(20 p623 in Saville) Equine degenerative myeloencephalopathy – symmetrical signs (Nout, p606) may get increased CSF CK (3 in Nout p608) and reduced serum Vitamin E concentrations but unreliable ante mortem dx Changes in leukogram and CSF seen with: Verminous encephalomyelitis – acute onset, CSF analysis (Jose-Cunilleras) Bacterial meningoencephalitis - stiff neck CNS abscessation (Furr)
Spinal trauma (Pasq) – hx (usually acute onest nuero signs), usually spolitary lesion loclaised by neuro exa (71 p589) rads, myelography, CT, MRI, nuclear scintigraphy, CSF analysis, nerve conduction velocities, EMG, transcranial magnetic stimulation (p590) Occipito-atlanto-axial malformation – deficits develop before 6mths (7,12, Seino) Cauda equina neuritis
Spinal tumors – CT, MRI, definitive dx requires cytology, biopsy, histopathology, CSF analysis (Sellon) Sorghum cystitis/ataxia (Pasq) – posterior ataxia or paresis, cystitis, hx of grazing Sorghum species (Talcott, ch22)
Prognosis
Depends on duration and severity of neurological signs[3] but clinical resolution is more likely if the condition is diagnosed and treated early.[2] With standard therapy, involving 6-8months of ponazuzril or pyrimethamine-sulfadiazine (V), there is a recovery rate of around 25% and an improvement in 60-75% of cases.[8] A good prognosis might be expected if there is an improvement in clinical signs within two weeks of commencing anti-protozoal and anti-inflammatory treatment (V). The prognosis will be guarded to poor[1] for a horse with severe irreversible neuronal damage or one that has not been diagnosed or treated appropriately (V).
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Pasquini, C, Pasquini, S, Woods, P (2005) Guide to Equine Clinics Volume 1: Equine Medicine (Third edition), SUDZ Publishing, 245-250. Cite error: Invalid
<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content - ↑ 2.0 2.1 2.2 2.3 Gray, L.C, Magdesian, K.G, Sturges, B.K, Madigan, J.E (2001) Suspected protozoal myeloencephalitis in a two-month-old colt. Vet Record, 149:269-273.
- ↑ 3.0 3.1 Vatistas, N, Mayhew, J (1995) Differential diagnosis of polyneuritis equi. In Practice, Jan, 26-29.
- ↑ 4.0 4.1 Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ DEFRA, The Animal Health Trust, The British Equine Veterinary Association (2009) Surveillance: Equine disease surveillance, April to June 2009, The Vet Record, Oct 24:489-492.
- ↑ Dubey, J.P, Lindsay, D.S, Saville, W.J, Reed, S.M, Granstrom, D.E, Speer, C.A (2001)A review of Sarcocystis neurona and equine protozoal myeloencephalitis (EPM). Vet Parasitol, 95:89-131. In: Pusterla, N, Wilson, W.D, Conrad, P.A, Barr, B.C, Ferraro, G.L, Daft, B.M, Leutenegger, C.M (2006) Cytokine gene signatures in neural tissue of horses with equine protozoal myeloencephalitis or equine herpes type 1 myeloencephalopathy. The Vet Record, Sep 9:Papers & Articles.
- ↑ Wobeser, B.K, Godson, D.L, Rejmanek, D, Dowling, P (2009) Equine protozoal myeloencephalitis caused by Neospora hughesi in an adult horse in Saskatchewan. Can Vet J, 50(8):851-3.
- ↑ MacKay, R.J (2006) Equine protozoa myeloencephalitis: treatment, prognosis and prevention. Clin Tech Equine Pract, 5:9-16. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.