| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
|
|
Introduction
- Although the CNS is well protected, its defences against organisms that have already invaded are less well developed. This is due to:
- Minimal antibody production
- Cerebrospinal fluid providing a good culture medium for invading organisms.
- Inflammatory cell, antibody and drug entry to the CNS being impeded by the blood-brain barrier.
Classification of Inflammation
- CNS inflammation may manifest as encephalitis or meningitis.
- These often co-exist.
- The aetiology CNS inflammation may be:
- Infectious
- Bacteria
- Fungi
- Protozoa
- Viruses or non-infectious.
- Infectious agents vary geographically.
- Non-infectious
- No infectious cause can be found in 60% of meningitis cases.
- Infectious
- Inflammation may also be broadly classified based on the nature of the exudate present.
- Fibrinous
- Caused by bacteria infection (including Mycoplasma).
- Suppurative
- Caused by bacteria and fungi.
- Granulomatous
- Caused by bacteria or fungi.
- Lymphoplasmacytic
- Caused by viruses.
- Haemorrhagic
- This is rare.
- Usually associated with septicemia or infarcts.
- Fibrinous
Routes of Entry
- CNS inflammation is usually the result of infection.
- This may be caused by:
- Bacteria
- Fungi
- Protozoa
- Viruses
- This may be caused by:
- Organisms must first enter the CNS in order to establish infection.
- There are several routes of entry that allow this:
- Haematogenous entry
- This is the most common route.
- Entry via the peripheral nerves
- Organisms track within the axoplasm of axons.
- For example, Listeria monocytogenes.
- Penetrating trauma
- For example, dehorning wounds, skull fracture or tail docking.
- Direct spread of infection
- From the nasal cavity, middle ear or paranasal sinuses.
- Haematogenous entry
- There are several routes of entry that allow this:
Localisation of Infectious Organisms
- After entry, organisms may establish in one or more of four main areas:
- Epidural space
- Infection tends to manifest as abscess formation.
- Subdural space
- Manifests as abscess formation.
- Fairly uncommon.
- Leptomeninges
- Causes leptomeningitis, which may be:
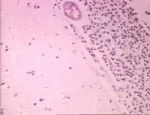
- Suppurative
- The most common form.
- Neutrophils are the predominant cell type.
- Caused by bacteria
- E.g. E. coli and Streptococcus
- There are often no gross lesions, but the brain may appear swollen and the meninges opaque.
- Usually results in death.
- Eosinophilic meningoencephalitis
- The classic example of this is porcine salt poisoning, when water has been restricted and the suddenly replenished.
- Perivascular eosinophilic cuffing is seen in the cerebrum and meninges.
- Lymphocytic
- Usually of viral origin.
- Granulomatous
- Caused by fungal diseases and Mycobacteriosis.
- Suppurative
- Causes leptomeningitis, which may be:
- CNS parenchyma
- Epidural space
Bacterial Infections
- Bacterial infections typically result in abscesses.
- These may be single or multiple depending on the route of entry, and vary in size.
- They contain a central, liquefied cavity.
- There are differences between cerebral abscesses and those occuring elsewhere.
- Encapsulation is slow.
- This is due to a lack of fibroblasts.
- There is therefore less collagen in the capsule.
- Astrocytic glial fibers are not as strong as collagen
- Encapsulation is slow.
- Other organisms may cause similar infections:
- Rickettsial organisms
- E.g. Ehrlichia
- Spirochates
- E.g. Leptospirosis
- Rickettsial organisms
Viral Infections
- Viral infections tend to reach the CNS by haematogenous spread and via peripheral nerves.
- There are three hallmark lesions of CNS viral infections:
- Neuronal necrosis
- Gliosis
- Vascular changes
- Several types of virus may cause inflammation in the CNS.
- Neurotropic, e.g.
- Rabies (rhabdovirus)
- Aujesky’s disease (herpesvirus)
- Visna (ovine lentivirus)
- Endotheliotropic, e.g.
- Infectious canine hepatitis (canine adenovirus)
- Classical swine fever (pestivirus)
- Equine herpesvirus type 1 (herpes)
- Pantropic
- Infectious canine distemper (morbillivirus)
- Infectious bovine rhinotracheitis (bovine herpesvirus type 1)
- Neurotropic, e.g.
- Other examples of viruses affecting the CNS:
- Distemper
- Parvovirus
- Parainfluenza
- Herpes
- FIP
- FIV
- FeLV
- Pseudorabies
- Rabies
Prion Diseases
- Prion diseases are also knowns as transmissible spongiform encephalopathies (TSEs).
- They are a group of fatal neurodegenerative diseases which occur in a number of species, including man.
- For example:
- BSE in cattle
- Scrapie in sheep
- Chronic wasting disease in elk
- CJD, Gerstmann-Sträussler-Scheinker disease (GSS), fatal familial insomnia (FFI) and kuru in man
- For example:
- TSEs have a long incubation period, making them difficult to diagnose.
Aetiology
- The aetiology of prion diseases is still highly controversial.
- However, an abnormal isoform of the host-encoded prion protein (PrP) is seen in the brains of affected animals.
- The normal host PrP changes its structure into the disease-associated form PrPSc.
- The abnormal proteint (PrPSc) accumulates as amyloid fibrils in nervous tissue.
- However, an abnormal isoform of the host-encoded prion protein (PrP) is seen in the brains of affected animals.
- The agent appears to be highly resistant.
Pathology
Gross
- Prion diseases cause NO GROSS LESIONS.
Hisological
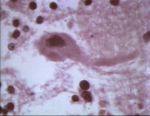
- TSEs typically cause what is known as the "microscopic triad":
- Spongiform change.
- Vacuolation of neurons.
- Particularly in nuclei.
- Astrogliosis
- Amyloid plaques
- These are not always seen.
- Spongiform change.
Non-Infectious Inflammatory Diseases
Granulomatous Meningoencephalitis (GME)
- An idiopathic CNS conditon
- May occur as:
- A disseminated disease
- A focal mass lesion
- A primary occular disease
- Brainstem signs are common, although the forebrain is primarily affected.
- May be incorrectly diagnosed as lymphoma.
- Changes are apparent in the CSF.
- There is usually a mononucloear pleocytosis.
- Sometimes only protein is elveated.
- Diffuse inflammatory changes or a mass lesion will be seen by advanced imaging.
- However, biopsy is required for a definative diagnosis.
- Life span is between 6 months and 1 year from diagnosis.
Treatment
- Immunosuppression:
- Corticosteroids
- Azathioprine
- Cycophosphamide
- Surgery
- This is only appropriate if there is a focal mass.
- Radiation therapy.
Pug Encephalitis
- A CNS idiopathic condition
- Affects pugs.
- Similar conditions are seen in yorkshire and maltese terriers.
- Officially known as necrotising meningoencephalitis of small dogs.
- Characterised by histological forebrain inflammation and necrosis.
- The disease is uniformly fatal.
- Corticosterid treatment has no effect.
Clinical Signs of CNS Inflammation
- Signs often reflect multiple levels of neurological involvement.
- Generalised forebrain signs are seen.
- Neck pain may be seen alone, or with other signs.
Diagnosis
- History, physical and neurological examination.
- Fundic examination may give clues as to whether a systemic infection is present.
- CSF examination may help define the problem.
Treatment
- Treatment is directed at a specific cause, if one can be found.
- If a cause cannot be found, trimethoprim, clindamycin or doxycycline plus or minus corticosteroids may be used.