Thrombosis may be due to:
- Endothelial injury.
- Altered blood flow E.g. abnormal stasis.
- Hypercoagulability.
Often associated with other disease processes for example Disseminated intravascular coagulation.
Commonly see posterior paralysis of cats with cardiomyopathy.
Spontaneous venous thrombosis is rare. Seen in cattle with traumatic reticulo-peritonitis in the caudal vena cava.
Description
Thrombosis is a localized or generalized intravascular clot formation. Thrombi form as the result of trauma or pathological processes affecting the blood vessel endothelium or disturbances to blood flow and/or blood composition. Some diseases such as infective endocarditis and heart worm increase the risk of thrombi formation.
Diagnosis
History & Clinical Signs
- Signs depend on the area affected and the size of the blocked vessel.
- Poor perfusion below affected area.
- Malfunction and necrosis of affected organs
Laboratory Findings
Abnormalities associated with lack of blood perfusion and/or pathological conditions.
Ultrasonography
- Blood stasis
- Visualization of a thrombus
Angiography
- May show lack of opacity in affected region
Treatment
-Treat underlying problem
-IV Fluids
-Anticoagulant (Heparin for short term treatment, Aspirin for long term treatment)
Prognosis
-Depends on underlying condition
From general pathology
Introduction
- A thrombus is a solid blood clot that forms within the vessels or heart during life.
- The process of thrombus formation is known as thrombosis.
- Thrombii may occur anywhere within the cardiovascular system.
Thrombosis
- The process usually begins with platelets becoming sticky.
- Adhere to each other and to the endothelium.
- This increased "stickiness" is induced by contact with:
- Collagen
- Basement membrane
- Damaged endothelial cells
- Bacteria
Appearance of a Thrombus
- A thrombus is a layered mass which is attached to the vessel wall.
- The composition of a thrombus consists of red blood cells, [[Neutrophils - WikiBlood|neutrophils]] and platelets bound together by fibrin.
- Thrombi take different appareance depending on whether they are arterial or venous.
- Arterial thrombi
- Tend to be pale and have a tail in the direction of blood flow.
- The high rate of blood flow sweeps red cells away - the thrombus is composed of mainly white cells, platelets and fibrin which are left behind.
- Tend to be pale and have a tail in the direction of blood flow.
- Venous thrombi
- Tend to be a darker red.
- The slow blood flow allows the clot to form quicker.
- Loosely arranged.
- Contains many red blood cells.
- Tend to be a darker red.
- Arterial thrombi
Causes of Thrombosis
- Thrombosis is caused by any condition that allows platelets to adhere to the endothelial wall.
Damage to the Vessel Wall
- When there is damage of the overlying endothelium, collagen is exposed and platelets will attach to this.
- The blood clotting process will occur, giving formation of an intraluminal blood clot.
- The process of formation occurs in phases giving a cross section of the clot a laminated appearance.
- The blood clotting process will occur, giving formation of an intraluminal blood clot.
- Vessel walls may be damaged in several ways:
- Trauma
- Localisation by colonies of bacteria
- Viral infection of endothelial cells
- Migration of parasites.
- Repeated puncture of the jugular vein is a common cause of serious or fatal thrombosis.
Changes in Normal Blood Flow
Stasis
- Stasis prevents coaglation factors being cleared by the liver and reticuloendothelial system.
- Coagulation factors build up, leading to clot formation.
- When stasis occurs in a vein, the thrombus forms behind the valve cusps.
- Quickly enlarges to fill the lumen.
Turbulence
- Turbulence disrupts the laminar flow.
- Platelets are brought into contact with the endothelial wall and may even damage the endothelium.
- Thrombi tend to form at arterial branches and venous junctions where there are eddy currents and local stasis.
Changes in Blood Composition
- An increase in the number and adhesiveness of platelets, or in plasma fibrin and clotting factors results in a hypercoagulateable state
- There may also be a decrease in the activity of the fibrinolyltic system.
- This may be caused by surgical or traumatic shock, or inflammation with toxaemia.
Types of Thrombosis
Arterial Thrombosis
- Although this is common in man, it is uncommon in domestic animals.
- A major problem in man associated with atherosclerotic vascular disease.
- When they do occur in animals, arterial thrombi are usually small lesions.
- However, these may be sited strategically, thereby causing problems.
Arteriosclerosis
- Seen in aged dogs and horses.
- Affect the coronary artery and other major arteries.
Verminous arteritis
- May occur with or without aneurysm.
- Seen in horses as a result of Strongylus vulgaris infestation.
- Affects the root of cranial mesenteric artery, renal artery and aorta.
- Results from larval migration in vessel walls.
Iliac thrombosis
- Seen in cats in the UK.
- Often referred to as "saddle embolus".
- Associated with cardio-myopathy and atrial thrombosis.
Cardiac Thrombosis
- Cardiac thrombosis is usually valvular, but can occasionally be mural.
Farm Species
- In farm animals, and rarely in the horse, infective/ inflammatory thrombosis occurs.
- Known as endocarditis.
Dogs and Horse
- Cardiac thrombosis is generally of degenerative/ non-infectious cause.
- Endocarditis may occur, though uncommonly.
- There are important effects of cardiac thrombosis.
- Distortion of valve cusps leads to mechanical effects.
- Ineffective closeure gives leakage (incompetence).
- Distortion and enlargement of the valves by the thrombus mas fuves narrowing of the valve outflow (stenosis).
- These effects lead to progressive inefficiency of cardiac pumping.
- Causes general venous congestion, oedema and circulatory failure.
- Emboli are disseminated from the thrombus mass.
- If the lesion is on the left side of the heart, emboli are disseminated systemically.
- Become trapped in the capilarry beds, e.g. of the kidney and spleen.
- Blockage leads to local ischaemic necrosis.
- Become trapped in the capilarry beds, e.g. of the kidney and spleen.
- If the lesion is on the right side of the heart, there is pulmonary dissemination.
- If the lesion is on the left side of the heart, emboli are disseminated systemically.
- Distortion of valve cusps leads to mechanical effects.
Atrial Thrombosis
- Uncommon.
- Seen rarely in cats and dogs.
- Results from stasis in atrial appendages.
Venous Thrombosis
- Venous thrombosis is a fairly common type of thrombus in the veterinary species.
- This is because:
- Veins are relatively thin-walled.
- Are therefore more susceptible to distortion, inflammatory damage and iatrogenic vene puncture damage.
- Veins have relatively slower blood flow rates.
- Cell aggregates tend to persist more readily.
- Veins are relatively thin-walled.
- This is because:
- Most venous thrombosis in domestic animals results from :
- Extension of inflammatory reactions.
- Erosion/disruption caused by malignant tumours.
- Pressure from adjacent space-occupying masses.
- Vene puncture damage.
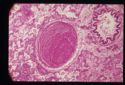
Capillary Thrombosis
- These are microthrombi.
- Only appreciable histologically.
- Formation may be:
- Localised
- Associated with acute local inflammation.
- Not very significant unless strategically sited.
- Generalised
- May be seen in terminal disease as a reflection of vascular failure.
- Often associated with shock syndromes as part of disseminated intravascular coagulation.
- Clinically very significant.
- Localised
Evolution of a Thrombus
- If the animal survives the immediate effects of a thrombus, the thrombus may evolve in one of the following ways:
- The thrombus may gradually enlarge and eventually cause total obstruction of a vessel.
- The thrombus may be completely removed by fibrinolytic activity.
- Fibrinolysis is a very active process - clots are usually removed within a few days of formation.
- Blood flow is crucial to the process of fibrinolysis.
- An occlusive thrombus may prevent the necessary enzymes from reaching the clot.
- To overcome occlusion, contraction of fresh clots under the influence of thrombasthenin (released by platelets) forms a slit-like channel beside the thrombus.
- The blood that then flows past may completely dissolve the clot.
- Organisation
- A thrombus acts as a foreign body, causing an inflammatory response in the underlying blood vessel or heart wall.
- The external surface of the thrombus quickly becomes covered by endothelium.
- Is excluded from the clotting mechanism.
- Neutrophils invade the mass and may digest the centre.
- Occasionally, subsequent invasion by bacteria may lead to to purulent inflammation.
- Normally, fibroblasts and capillary buds follow the [[Neutrophils - WikiBlood|neutrophils]] into the thrombus and a fibrous vascularised connective tissue forms.
- Capillaries channels anastomose to produce vessels that traverse the thrombus and re-establish blood flow.
- This is known as canalisation of a thrombus.
- Fibrous tissue matures and contracts, eventually causing the thrombus to become incorporated into the vessel wall as a fibrous lump.
- Capillaries channels anastomose to produce vessels that traverse the thrombus and re-establish blood flow.
- A piece of the thrombus may break off and form an embolus.