Description
Tuberculosis in cattle is caused by Mycobacterium bovis. It is a chronic disease characterised by nodular lesions in any organ, although the respiratory system is most commonly affected. The nodules often become nectroic with a caseous centre.
Historically bovine TB was a major cuase of human TB, the government introduced
The pasturisation of milk was introduced which dramatically reduced transmission to humans and bovine Tb as a cuase of human disease is now very low indeed.
The disease is of serious economic importance to farmers becasue of the stringent testing and slaughter control measures which remain in place.
Signalment
Incidence of the disease has increased
Diagnosis
Clinical Signs
Laboratory Tests
Radiography
Pathology
Treatment
Prognosis
References
- Reside primarily within macrophages where they multiply and result in characteristic granulomatous inflammation (macrophages and giant cells, epithelioid cells)
- Cattle can be infected by inhalation of the organism or through milk
- The primary complex
- Describes the initial focus of infection at the portal of entry (lungs) plus involvement of regional lymph nodes
- 90% of cases exhibit the pulmonary form
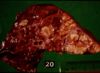
- Grossly:
- Small tubercles in dorsocaudal subpleural areas which progress to larger confluent areas of caseous necrosis
- Usually start at bronchio-alveolar junction an progress to the alveoli
- Caseous lesions, may calcify or be encapsulated
- Multiple foci may coalesce
- Ulcers in trachea and bronchi due to coughed up bacteria
- Spreads into pleura
- Microscopically:
- Typical granulomatous inflammation
- Epitheliod and giant cells at centre of tubercles
- Macrophages with ingested bacteria, forming epithelioid cells - large vesicular nuclei, abundant pale cytoplasm
- Giant cells, formed by fusion of macrophages, with multiple nuclei
- Narrow layer of lymphocytes, mononuclear cells and plasma cells at the periphery of the tubercle
- With time, peripheral fibroplasia and central necrosis develop
- If the infection is not contained in the primary complex described above, the mycobacteria can disseminate via lymphatics to other organs and lymph nodes
- This can allow the development of miliary tuberculosis, i.e. numerous small foci of infection in many organs/ tissues
- inhalation of Mycobacterium bovis most common via droplets
- some tubercle bacilli enter the lymph and travel to the bronchial or mediastinal nodes
- inhaled bacilli reach the alveoli, set up a focus of inflammation
- phagocytosed by alveolar macrophages
- two processes may develop if the animal has not encountered the organism before:
- - the organism may grow in the phagocytes as intracellular parasites
- - produces a nodule of parasitised swollen macrophages known as a tuburculous nodule or a tubercle granuloma
- - ultimately, macrophages are killed and infection spreads
- - the organism may be broken down and some antigens taken up by the immune system
- - cell mediated immune system produces cytotoxic T-lymphocytes
- - T-lymphocytes can attack and destroy cells harbouring bacilli
- - leads to type IV (delayedd type) hypesensitivity
- - 'caseous' or cheesy type of necrosis
- - if bacterium destroyed, further infection/disease is prevented
Sequelae
- chronicity
Tuberculosis pleurisy
- caseous lymph node ruptures
- results from extensive tissue necrosis
- - if located in lung alveoli, the follicle may rupture into a bronchus, causing spread of the disease to all the other lobules served by that bronchus
- - if the ensuing necrosis erodes the wall of a large pulmonary vessel, this ruptures into the lung and a fatal haemoptysis might follow