Small Animal Emergency and Critical Care Medicine Q&A 02
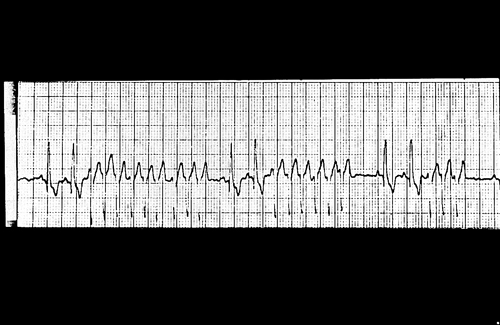
A three-year-old, spayed female Great Dane presented recumbent with abdominal distension. She received 4 liters of lactated Ringer’s solution i/v and remained recumbent with pale mucous membanes. She was decompressed with an orogastric tube. On auscultation, HR is rapid and pulses are barely palpable.
| Question | Answer | Article | |
| What is the ECG diagnosis (106; speed 25 mm/sec)? | Paroxysmal ventricular tachycardia at a ventricular rate of 300 bpm. |
Link to Article | |
| What interventions are necessary at this time | A slow intravenous bolus of lidocaine 2% (2–4 mg/kg) is given. This dose can be repeated if there is poor or no response. Once converted to sinus rhythm, an i/v continuous lidocaine infusion (50–75 μg/kg/minute) is given. Alternatively, a slow i/v procainamide bolus is given and a continuous infusion (11–40 μg/kg/minute) started after conversion. Bretyllium can be given i/v, allowing 20 minutes for the full effect. If, however, conversion to sinus rhythm is unsuccessful by medical intervention, electrical defibrillation (can start with 100 J) is an option as this can precede sustained ventricular tachycardia and fibrillation. |
Link to Article | |
| What are possible adverse reactions to drug treatment, and how should they be treated? | The risk of profound hypotension associated with too rapid infusion. Also, gastrointestinal side-effects may occur but are transient and eliminated at lower dosages. With lidocaine, increased dosage may cause ataxia or seizures which can be treated with i/v diazepam and discontinuation of the drug. |
Link to Article | |
| What are possible causes of this dog’s new problem, and what diagnostics would be indicated? | Causes include hypoxia, acid–base or electrolyte disturbances and myocardial irritability secondary to toxemia. Also, Great Danes are predisposed to dilated cardiomyopathy which may go undetected until a serious illness. Obtaining an arterial blood gas and eletrolytes (to include K+ and Mg++) and appropriate treatment to correct these abnormalities should precede surgical gastric repositioning. Chest radiographs and an echocardiogram should be included in the preoperative monitoring. |
Link to Article | |