Labrador cross with mass on antebrachium
Signalment:
- 7-year-old male neutered Labrador cross
Presenting sign:
- 7 x 5 cm firm mobile mass on the caudal aspect of the proximal antebrachium, which has grown over the past three months. Otherwise clinically well, with no evidence of lameness and no other history of illness. Physical exam is otherwise within normal limits.
100 |
|
1 |
What would be your next step? |
| Histopathology report |
|---|
| Gross pathology One pot is submitted:biopsy of the leg. A pece of pale tan resilient tissue measuring 7 x 5 x 5 mm. A representative section is placed in Cassette A. Histopathology This is a section of a tumour composed of sheets of neoplastic pleomorphic polyhedral to spindle cells with a mitotic index approximating 1-2 mitoses per high power field. They are accompanied by minimal collagen. The neoplastic cells have mild karyomegaly and nucleolar prominence together with abundant eosinophilic, vacuolated cytoplasm. Diagnosis Cutaneous soft-tissue sarcoma, grade 2. Comments This diagnosis is in keeping with the previous cytological findings. The minimal collagen and cytoplasmic vacuolation evident in this case raises the possibility of liposarcoma as a more specific diagnosis. In any case, this tumour is likely to be characterized by infiltrative local growth but negligible tendency for metastatic spread. |
2 |
Review the histopathology report. What do you understand about the behaviour of soft-tissue sarcomas (STS)? |
3 |
What is the metastatic rate of grade 2 STS? |
4 |
What is the metastatic rate of grade 1 STS? |
5 |
What is the metastatic rate of grade 3 STS? |
6 |
What would you choose to do next? |
7 |
You now know that the regional lymph node is not palpable, and the thoracic radiographs are unremarkable. You have adequately staged this tumour to stage I (primary site only). What can be expected with adequate treatment of this tumour? |
8 |
Haematology, biochemistry and urinalysis before surgery are within normal limits. What is your preferred option for treatment of the local tumour? |
9 |
Unfortunately radiation therapy is not available, and the clients refuse amputation. The specialist oncology surgeon plans the surgery to achieve the widest margins possible (deep and lateral), and then reconstructs the deficit with an axial pattern flap. What is an axial-pattern flap? |
10 |
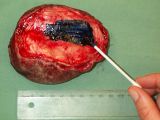
Which axial-pattern flap would be most appropriate to close this deficit (see photo)? |
11 |
You resect the tumour and send tissue for histopathology. How do you prepare the resected tissue so that the pathologist is best equipped to give the information you need? |
12 |
The margins are clear and the pathologist confirms your histological diagnosis of grade 2 STS: it is a haemangiopericytoma. What other tumours fit the STS category, characterized by similar biological behaviour? (Choose three of the following.) choice1= |
13 |
|