Labrador cross with mass on antebrachium
Signalment:
- 7-year-old male neutered Labrador cross
Presenting sign:
- 7 x 5 cm firm mobile mass on the caudal aspect of the proximal antebrachium, which has grown over the past three months. Otherwise clinically well, with no evidence of lameness and no other history of illness. Physical exam is otherwise within normal limits.
1 |
What would be your next step? |
| Histopathology report |
|---|
| Gross pathology One pot is submitted:biopsy of the leg. A pece of pale tan resilient tissue measuring 7 x 5 x 5 mm. A representative section is placed in Cassette A. Histopathology This is a section of a tumour composed of sheets of neoplastic pleomorphic polyhedral to spindle cells with a mitotic index approximating 1-2 mitoses per high power field. They are accompanied by minimal collagen. The neoplastic cells have mild karyomegaly and nucleolar prominence together with abundant eosinophilic, vacuolated cytoplasm. Diagnosis Cutaneous soft-tissue sarcoma, grade 2. Comments This diagnosis is in keeping with the previous cytological findings. The minimal collagen and cytoplasmic vacuolation evident in this case raises the possibility of liposarcoma as a more specific diagnosis. In any case, this tumour is likely to be characterized by infiltrative local growth but negligible tendency for metastatic spread. |
2 |
Review the histopathology report. What do you understand about the behaviour of soft-tissue sarcomas (STS)? |
3 |
What is the metastatic rate of grade 2 STS? |
4 |
What is the metastatic rate of grade 1 STS? |
5 |
What is the metastatic rate of grade 3 STS? |
6 |
What would you choose to do next? |
7 |
You now know that the regional lymph node is not palpable, and the thoracic radiographs are unremarkable. You have adequately staged this tumour to stage I (primary site only). What can be expected with adequate treatment of this tumour? |
8 |
Haematology, biochemistry and urinalysis before surgery are within normal limits. What is your preferred option for treatment of the local tumour? |
9 |
Unfortunately radiation therapy is not available, and the clients refuse amputation. The specialist oncology surgeon plans the surgery to achieve the widest margins possible (deep and lateral), and then reconstructs the deficit with an axial pattern flap. What is an axial-pattern flap? |
10 |
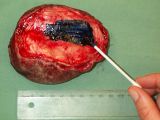
Which axial-pattern flap would be most appropriate to close this deficit (see photo)? |
11 |
You resect the tumour and send tissue for histopathology. How do you prepare the resected tissue so that the pathologist is best equipped to give the information you need? |
12 |
The margins are clear and the pathologist confirms your histological diagnosis of grade 2 STS: it is a haemangiopericytoma. What other tumours fit the STS category, characterized by similar biological behaviour? (Choose three of the following.) choice1= |
13 |
What next step do you propose? |
14 |
You recheck your patient frequently and after 12 months there is evidence of a 5 × 3-cm wide, fixed soft-tissue swelling along one area of the surgical suture line at the proximal lateral antebrachium and overlying the ventrolateral chest wall. You biopsy this swelling as a small wedge biopsy and this confirms local recurrence of tumour, this time as a grade 3 STS. You had warned the clients that amputation was your preferred treatment option due to the difficulty in attaining margins because of tumour size and location, and so they are disappointed but not unprepared. It was also explained to them that recurrent disease has a poorer prognosis than optimally treated first-time, curative intent surgery. What would you do next? |
15 |
Luckily, your thoracic radiographs are negative for pulmonary metastatic disease, and there is still no palpably enlarged regional lymph node. You have optimized this patient’s outcome by ensuring frequent rechecks. However, you need to treat the primary tumour. What is the commonest cause of death for dogs with subcutaneous STS? |
16 |
The clients are prepared for amputation, which your advanced imaging shows is most appropriate, as you will not be able to attain wide margins without it. You perform the amputation and succeed in attaining 3-cm margins around gross tumour, confirmed by the pathologist. You continue your frequent rechecks. Unfortunately, after 6 months there is evidence of two nodules in the caudal lung fields.Now it is optimal for you offer the clients doxorubicin chemotherapy. True or false? |
| This resource was adapted from North and Banks, Small Animal Oncology provided by Elsevier Health Sciences as part of the PublishOER Project. | 
|