Difference between revisions of "Degenerative Mitral Valve Disease"
| Line 1: | Line 1: | ||
{{unfinished}} | {{unfinished}} | ||
| − | Also known as: '''''MVD — Mitral Valve Disease — Mitral insufficiency — Mitral endocardiosis — Myxomatous Mitral Valve Disease (MMVD)''''' | + | Also known as: '''''MVD — Mitral Valve Disease — Mitral insufficiency — Mitral endocardiosis — Myxomatous Mitral Valve Disease (MMVD) - Endocardiosis''''' |
==Introduction== | ==Introduction== | ||
Revision as of 15:21, 16 November 2010
| This article is still under construction. |
Also known as: MVD — Mitral Valve Disease — Mitral insufficiency — Mitral endocardiosis — Myxomatous Mitral Valve Disease (MMVD) - Endocardiosis
Introduction
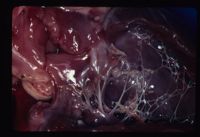
Mitral valve dysplasia is a congenital malformation or degeneration of the mitral valve leaflets and its supporting structures (chordae tendinae, papillary muscles, valvular leaflets, annulus) resulting in valvular regurgitation (insufficiency). It is common in dogs and cats and rare in other species.
Chronic mitral regurgitation leads to volume overload of the left heart, which results in dilatation (eccentric hypertrophy) of the left ventricle and atrium. When mitral regurgitation is severe, cardiac output decreases, which results in signs of left sided cardiac failure (LCHF) and pulmonary venous congestion. Dilatation of the left-sided chambers predisposes affected animals to arrhythmias. In some cases, malformation of the mitral valve complex causes a degree of valvular stenosis as well as insufficiency.
In advanced cases, signs of right sided congestive heart failure may follow due to an increased pressure load on the right ventricle as a result of long standing pulmonary congestion.
Signalment
Typically in middle aged to older small breed dogs. Genetically predisposed breeds include Cavalier King Charles Spaniel, Bull Terriers, German Shepherds, and Great Danes.
Diagnosis
History
Animals may remain asymtomatic for years. Typical reported signs include exercise intolerance and dyspnoea as a result of reduced cardiac output and a ventilation perfusion mismatch due to pulmonary oedema. A progressive cough often during rest or recumbancy is frequently seen and needs to be distinguished from primary respiratory disease. Sudden death is possible due to a left atrial tear or advanced pulmonary oedema.
Clinical Signs
- Left apical systollic murmur
- Left sided congestive heart failure
- Resting Tacchycardia
- Pale Mucous membranes
- Prolonged Capillary refill time (CRT)
- Prolonged Jugular filling time
- Pulmonary crackles / evidence of pulmonary oedema
- Cool extremities
- Loss of sinus arrhythmia
- Cardiac arrhythmias e.g. Atrial fibrillation, Atrial premature complexes
Diagnostic imaging
Radiography
Left Lateral, right lateral and ventrodorsal views of the thorax are needed. The key radiographic signs associated with mitral valve dysplasia and resulting left sided congestive heart failure are cardiomegaly, pulmonary venous congestion (enlarged pulmonary arteries and veins) and pulomary oedema. Cardiomegaly may lead to dorsal displacement of the trachea.
Evidence of Right sided congestive heart failure maybe evident in severe cases e.g. distended caudal vena cava, hepatomegaly, ascites, pleural effusions.
Echocardiography
Evidence of left atrial and left venrticular enlargement is visible on echocardiography. The 'fractional shortening' is also increased which is measured as the percentage change in the left ventricular diameter during systole and is used as a measure of systollic function. It is also possible to see structural changes in the valve leaflets in some cases. The regurgitant jet of blood can be detected using colour doppler and evidence of turbulent flow.
Electrocardiogram (ECG)
A resting ECG trace may show evidence of an enlarge left atrium (Wide P Wave), an enlarged left ventricle (Tall R wave, wide QRS complex, shift of mean electrical axis to the left) and rhythm disturbances such as sinus tacchycardia, atrial fibrillation, atrial premature complexes and atrial Tacchycardia.
Laboratory Tests
Pro-brain natriuretic peptide (N-BNP) is a newly described cardiac hormone considered to be an effective marker of severity and prognosis of acute coronary syndromes and congestive heart failure. Circulating levels of the hormone increase in peripheral blood with increased myocardial stress. Commercial assays are not currently available.
Treatment
No treatment is recommended prior to the onset of heart failure. Once there is evidence of congestive heart failure, treatment is aimed at its management through a combination of drugs.
The aims of treatment are to:
1. Reduce Preload
- Diuretics to reduce circulating fluid volume (Frusemide, Benzofluazide, Spironolactone, Amiloride)
- Vasodilators to reduce venous return (Nitrates, ACE inhibitors, Alpha antagonists)
2. Reduce Afterload
- Vasodilators to decrease systemic vascular resistance
- ACE inhibitors e.g. Enalapril, Benzapril, Imidopril ,
- Pimobendan
- Calcium channel blockers e.g. Amlodipine
- Nitrates e.g. Nitroprusside
- Vasodilators to decrease systemic vascular resistance
3. Enhance Systolic function
- Positive Inotropes to increase cardiac contractility and increase cardiac output.
- Pimobendan
- Digoxin
- Dobutamine
- Xanthines
- Positive Inotropes to increase cardiac contractility and increase cardiac output.
4. Improve Diastolic function
- Negative Chronotropes to increase the length of diastole (digoxin, atenolol)
- Calcium channel blockers to improve relaxation (amlodipine)
5. Control cardiac arrhythmias using anti-arrhythmic drugs
Prognosis
Mitral Valve Dysplasia can remain asymptomatic for many years (average 4 years). Once congestive heart failure has developed, the progression of the diseae can be monitored by the severity of the clinical signs (cough, exercise intolerance) and radiographically looking at caridac size, the degree of pulmonary oedema and the size of the left atrium. Cardiac size can be measured objectively using the Vertebral Heart Score method. Mean survival of 200-300 days once in overt cardiac failure with standard treatment protocols.
Literature Search
References
- Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition) Merial
- Nelson, R.W. and Couto, C.G. (2009) Small Animal Internal Medicine (Fourth Edition) Mosby Elsevier.
- Tilley, L.P. and Smith, F.W.K.(2004)The 5-minute Veterinary Consult (Third edition) Lippincott, Williams & Wilkins.
- Tilley,L.P., Smith, F.W.K, Oyama, M., Sleeper, M. (2007) Manual of Canine and Feline Cardiology Saunders.