LabFacts Histology
Making the most of your surgical biopsy submission
Our histology department is appealing for your clinical data. This means the information that should accompany your surgical biopsy submission form. As a general rule the smaller your submission the more clinical data we need to accompany it.
So, what to put on the submission form that accompanies a surgical biopsy?
- Please send one
- Signalment. Many lesions are age, sex and breed specific (and some are species specific)
- An outline of the location and distribution of the lesion along with lesion-specific clinical history
- Any other recent clinical findings
- Reference to any previous surgical biopsies or clinical tests
- Recent medication
We are always happy to discuss cases over the telephone or by email so please contact us if you would like to discuss a case and we are always interested in images of the lesion, as gross lesions, radiographs or ultrasound images. These can be sent with the submission or electronically to admin@nwlabs.co.uk. Don’t forget to put the patient’s name on them so we can match them to the submission when it arrives.
Emerging diseases
From a histology perspective we have a small but significant and increasing number of cases of more exotic diseases emerging. Two of the most common scenarios cutaneous Leishmaniasis and transmissible venereal tumour are described on the opposite page.
Cutaneous Leishmaniasis
This is an intracellular protozoal parasite which in endemic areas is transmitted by sandflies.
There are a number of species of Leishmania which cause infection in the dog. The most common cause is Leishmania infantum, which is primarily responsible for infection in humans. Leishmaniasis in dogs is often a combination of the cutaneous and visceral forms. It is most commonly found around the Mediterranean and Eastern Europe but has a worldwide distribution.
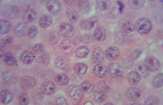
In our histology department we most commonly see canine Leishmaniasis in skin or lymph node biopsies with the diagnostic intracellular amastigotes best seen in lymph node cytology preparations. Two patterns of skin lesions are seen. The most common is a nonpruritic exfoliative dermatitis with alopecia, often observed around the eyes, muzzle and pinnae. Clinically it can resemble autoimmune disease, zinc responsive dermatosis or sebaceous adenitis. The nodular form of the disease is less common and thought to be associated with immunosuppression. It can resemble any form of granulomatous disease, including cutaneous lymphoma. The condition can also be associated with brittle nails. Skin biopsy is very important in differentiating these conditions. Biopsies should be taken from multiple areas of affected scaling skin or nodules . Lymph node or bone marrow cytology may also be helpful in establishing a diagnosis. In addition we can also detect Leishmania infection using immunofluorescent antibody or real-time PCR techniques so please see our price list or telephone our laboratory for more information.
Transmissible venereal tumour
This is an interesting and unusual tumour which is unique to the dog and is transmitted by spread of tumour cells from dog to dog. The tumour spreads rapidly where dogs roam freely or are in large breeding colonies. Despite extensive research the origin of these tumour cells is unknown. They most closely resemble canine leucocytes but they exhibit a different karyotype to canine cells. They present as nodular, often papillary, cutaneous masses which tend to ulcerate and become infected. They can present anywhere on the skin or mucosa, including the nose and oral cavity. They occur most commonly on the genitalia. They develop rapidly, initially. Growth then tends to decrease, indicative of a developing immune response. Many tumours spontaneously regress and dogs are then immune to further infection. However, in some dogs which are immunosuppressed, there can be development of multiple skin tumours as well as spread to lymph nodes and other organs in a manner similar to any other malignant tumour. Diagnosis is by surgical biopsy and histological examination.
Either of these conditions can develop months to years after the dog has been abroad, therefore a detailed history going back to puppyhood may be required. Also, with increasing travel abroad and ongoing climate change, we must be vigilant to these conditions becoming more prevalent in the UK.
Unusual biopsy specimens
Most biopsy specimens arrive at the histology laboratory in good order and can be easily orientated and sectioned, however some samples are not straightforward and can provide frustrating results. Here is a quick guide to some of the more common problems. As always, if you have any queries please call our office and they will be happy to direct you to a pathologist or member of the histology laboratory staff who can advise you. Please don’t forget to include the submission form indicating how many pots should be present, how many samples in each pot and biopsy sites, with as much signalment and history as possible.
Large specimens
All biopsies should be fixed in 10% neutral buffered formalin (NBF). Maximum tissue thickness to allow optimal penetration of NBF is 10mm.
Several options:
- Take multiple representative samples of up to 10mm from different areas of the lesion. We will examine up to 4 specimens for the same price
- If you want to send the whole sample you can slice through the tissue using parallel slices which do not quite reach the bottom of the sample. This means that we can reconstruct the sample in the lab and orientate it better. Such samples really need to be fixed in 20x the volume of NBF
- If the quantity of NBF required is too large and costly the sample can be sliced and fixed in NBF for 24 hours at your practice before being transferred to NBF-soaked paper towel, double bagged in zip lock plastic bags (without NBF) and sent to our laboratory
Margins
- The outer surface can be inked, using surgical ink, to outline the margins. Allow the ink to begin to dry before immersing in NBF. Rinsing the inked sample in a weak acetic acid solution prior to fixing has been found to help the ink to stay on the sample
- Margins can be tagged using different colours, lengths or numbers of sutures. Please do not under any circumstance use needles to mark margins. This is a safety issue for our laboratory staff
- If submitting separate biopsies please submit in separately labelled pots. Tissues can shrink, change texture and colour when fixed, making it very difficult to differentiate multiple tissues from the same pot
Small or friable specimens
Small or friable specimens such as endoscopic samples, punch biopsies and needle core biopsies are best placed in cell safe or screen cassettes which we can supply on request. Please pre-soak the cassettes in NBF before putting the sample inside. This helps to prevent the tissue sticking to the foam material inside. Pre-labelling the cassettes using a number 2 pencil before immersion in NBF means that multiple cassettes can be placed in the same pot. Samples can be fixed free in NBF; however, although we endeavour to sieve these samples, inevitably some fragments can be left behind – particularly if they are placed in the same pot as larger biopsies. Submission on gauze or card can cause samples to rip when removing for processing.
A single line drawn along the centre of skin punch biopsies in the direction of hair growth prior to biopsy can greatly assist us when orientating these samples.
Eyes
Enucleated eyes can be submitted whole in 10% NBF. There is no need to section the eye or inject the fixative as this causes significant artefactual damage.
Bone
Bone biopsies can be difficult to obtain and frustrating to interpret. This is because of the high risk of fracture during the biopsy procedure and, histologically, due to the presence of large quantities of reactive periosteum in most lesions, regardless of pathogenesis. A diagnosis of reactive hyperplasia is often of little clinical help. To try to alleviate this frustration it is useful to take as large a sample as possible and/or to take multiple biopsies with some from the centre of the lesion (which we don’t often ask for). This is more likely to demonstrate the true lesion rather than reactive hyperplasia. Multiple biopsies reduce the risk of obtaining only haemorrhage or necrotic tissue. Fixation in 10% NBF is adequate for routine diagnostic biopsies.
Claws
Claws need to be softened and phalangeal bone needs to be decalcified, so biopsies from claws and digits will take longer to report. The digital site is naturally very restrictive, therefore any expansile mass will cause similar clinical signs; abnormal nail growth, swelling, pain, lameness and lysis of the third phalanx. For this reason, amputation of one or more phalanges is the biopsy technique of choice. This includes inflammatory conditions of the nail bed, such as lupoid onychitis. Punch biopsy techniques have been described, however these can be very difficult to orientate in the lab and can result clinically in permanent disfigurement of the claw. If possible, an affected dew claw can be sacrificed. In most cases we will issue a preliminary report based on a soft tissue biopsy taken in the histology laboratory. In many cases this may reveal a definitive diagnosis, however in some cases we may need to wait for the final decalcified or softened sections before concluding the diagnosis or to establish excision margins.
Sampling lesions for osteosarcoma
When sampling suspicious bone lesions there are a number of methods which may be employed. All require a general anaesthetic and the sample should be radiograph guided. In each case the centre of the lesion should be sampled as peripheral tissue is often simply reactive.
Samples for cytological evaluation need to be taken aggressively in order to cause cell exfoliation and achieve a good cell yield for interpretation. Even with very good samples it can be difficult to differentiate these masses completely from plasmacytoma (multiple myeloma) and histiocytic sarcoma on the basis of cytology alone.
As a result the most commonly submitted histological samples are Jamshidi needle biopsies but owners should be warned even these can be non diagnostic. In order to increase the chance of getting a diagnosis three good solid samples should be the minimum submitted and the samples should be taken again from the centre of the lesion as identified by radiography. The risk of pathological fracture using this technique is very low and should fracture occur, it was likely to happen regardless of any interventional method.
Ideally the larger the sample the more likely it is to be representative of the underlying lesion although the risk of pathological fracture is increased. Again samples should be taken from the centre of the lesion. While this type of sample is unlikely to be non diagnostic chondroblastic osteosarcomas and chondrosarcomas appear very similar in small section and the sub type of osteosarcoma may not be truly represented in the wedge sample submitted. While in many cases this is not prognostically significant, telangiectatic osteosarcomas are much more aggressive with a poorer short term prognosis than any other sub types.
After excisional surgery the entire tumour should be assessed for definitive diagnosis before considering chemotherapy. This may be submitted within an entire limb or a reduced sample including the tumour portion of the bone only. Both of these must be formalin fixed in an adequate volume of formalin (ten times the tissue volume) for a minimum of 24 hours (formalin penetrates at a rate of 1cm every 24 hours so larger samples will require longer). Once fixed, samples may then be wrapped in formalin soaked tissue/swabs and double wrapped in thick plastic bags to prevent leakage.
Immunohistochemistry in tumour diagnosis
Increasingly general practitioners are faced with a histology report which suggests they use immunohistochemistry to further classify their tumour. Many of you must ask yourselves “Why hasn’t malignant melanoma (for example) always been malignant melanoma? Of course the answer is “Yes” but not all tumours previously diagnosed as malignant melanoma were in fact of melanocyte origin. With the development of immunohistochemical markers retrospective studies have shown that tumours were previously misclassified on the basis of H&E exam alone.
Although there are still clear indicators of a tumours origin, in many cases those masses that exhibit multiple conflicting features, or are so poorly differentiated that no typical features are present, can only be further diagnosed with the use of immunohistochemical means. In addition, some markedly reactive lesions, particularly those of lymphocytic origin, can mimic neoplasia and immunophenotyping may help to differentiate between reactive and neoplastic change.
Why has the use of immunohistochemistry increased?
Many of you will remember a time when immunohistochemistry was a test rarely recommended. This was in part due to the limited availability of antibodies for accurate tumour identification but also due to the limitations and costs of veterinary oncology. For many owners, hearing their animal has cancer is very distressing and for some the thought (and expense) of chemotherapy or radiotherapy is more than they wish to consider. However, with an increasing numbers of insured pets, and rapid advances in veterinary oncology, survival times for even some of the most aggressive cancers have been greatly improved. The increasing range of chemotherapeutics available for our patients makes an accurate diagnosis imperative; if the most up to date advice regarding the prognosis and possibilities of further treatment are to be provided to the owner.
How does it work?
Immunohistochemistry (IHC) is the process of detecting ‘tissue antigens’ using target antibodies, in histological sections. In the case of tumours the ‘antigens’ are typically structural proteins inherent to the specific cell of origin for example, cytokeratins in carcinomas. The antibodies bind specifically to these antigens and the subsequent antibody-antigen complex is then visualised, typically by means of a conjugated enzyme, such as peroxidase, that can catalyse a colour producing reaction. Alternatively a fluorophore, such as fluorescein or rhodamine, can be used to label the antibody. The sections are then examined microscopically and the neoplastic cells can be identified by means of positive or negative staining.
Do I need to submit special samples?
Immunohistochemistry is performed on fixed paraffin embedded tissue sections identical to those examined in H&E staining for routine histopathology. We can send the blocks of tissue you have already submitted for immunohistochemical staining, in most cases no additional tissue is required.
What are the limitations?
Although there are a large number of commercially available antibodies, the time and costs of processing an individual antibody are huge and many are prohibitively expensive. As a result, many published antibodies are, as of yet, only available in research establishments. However, the approach we use offers a diverse range, which should cover the majority of the neoplastic lesions encountered in practice. We always endeavour to offer our clients the best advice we can when it comes to ancillary testing; if there is a potentially relevant antibody you have encountered in your reading, which is not listed in our price list, we will try endeavour to source this for you. Antibodies we routinely offer are detailed in our current price list. We are here to offer help and advice on the most appropriate test or tests for your particular case. Please contact us to discuss your options.
Please visit www.nwlabs.co.uk or see our current price list for more information