Recognition and Description of Lesions
Jump to navigation
Jump to search
Introduction
- In order to make a veterinary diagnosis, it is essential to be able to recognise an abnormality.
- From the abnormality, we should be able to formulate an differential diagnosis before arriving at a diagnosis.
- The ability to scientifically and correctly communicate the nature of an abnormality allows
- Diagnoses to be made effectively.
- Easier communication between professionals.
Description of Lesions
- The very first stage in describing a lesion is to identify the species and tissue/ organ in which the lesion resides.
- The next stage is to describe "where" and "what" the lesion is; i.e. to describe the pathological changes present.
- Once the changes have been recognised and described, a diagnosis can be formulated.
Description of Pathological Changes
Where is the Lesion?
- Lesions may be decribed as:
- Focal
- This means the lesion involves only part of the tissue or organ.
- Focal lesions may be
- Solitary - one lesion only.
- Multifocal - more than one lesion is present.
- Multifocal lesions may "join-up" with each other- "multifocal to coalescing".
- Diffuse
- Diffuse lesions involve the whole organ or the whole of a specified area.
- Segmental
- When the lesion affects a portion of a tubular organ, for example the intestine
- Miliary
- Multiple small lesions.
- Focal
What is the Lesion?
- Several parameters are used to create a detailed description of a lesion.
- Size
- Size is outlined by giving linear measurements in 2 or 3 dimensions.
- It may also be useful to indicate how much of the organ or tissue is involved (i.e. as a percentage).
- Sometimes during a full PME it may be possible to also assess
- Weight of an organ or lesion.
- Must relate to something! For example, relate the weight of an organ to the weight of the animal as a whole.
- Volume of fluid
- Must again be relative.
- Weight of an organ or lesion.
- Shape
- Circular, oval, nodular and so on.
- The borders of the lesion can also be considered.
- Well or poorly defined/ demarcated
- Regular or irregular
- Smooth or ragged
- It is also possible to comment on the surface of the lesion
- E.g. flat, elevated, depressed, umbilicated, pedunclated, sessile.
- Colour
- Can use the primary colours plus grey, brown, black, white etc
- E.g. "reddish-brown"
- Is the colour seen light or dark?
- Does the lesion appear shiny or dull?
- Can use the primary colours plus grey, brown, black, white etc
- Consistency
- Determined by gentle and careful palpation.
- Described by:
- Type: soft, firm, hard
- Degree: slight, moderate, marked
- Cohesion: friable, elastic etc
- Different areas of a lesion may have different consistencies (e.g. the core may be softer).
- Odour
- Special features
- E.g. free fluid, blood, exudates etc.
- Appearance of the cut surface
- Consistency
- Amount of blood flowing from cut surface
- Any capsule and borders
- Description of the draining lymph node, if present.
- Describe as for the main lesion.
Interpretation of Lesions
- Following the recognition of a particular feature in the lesion, it is possible to make some interpretations of what is seen.
- Interpretation is not set in stone- each lesion varies and may be different to the generalisations made below.
Interpretation of Lesion Distribuution
- If lesions are evenly spread throughout an organ, it implies an infectious cause.
Interpretation Based on Lesion Shape
Raised Lesions
- Simplistically, a raised lesion implies that something has been gained.
Depressed Lesions
- Depressed lesions imply that something is missing or has been lost.
- For example:
Flat lesions
- The area is neither raised or depressed.
- Lesions are recognised by colour change.
- Flat lesions can imply an acute process.
- There has not yet been time for cells or fluid to accumulate, or for cells to be lost.
Demarcation
- In the case of neoplasms:
- Inflammatory lesions:
- Well demarcated lesions are often surrounded by fibrosis.
- Implies a chronic process.
- Poorly demarcated inflammatory lesions are often more acute.
- Well demarcated lesions are often surrounded by fibrosis.
Interpretation of Lesion Size
- Particularly important when submitting part of a lesion to a laboratory for histopathology.
- Assessing the proportion of the organ that is involved can be important in determining the functional significance of a lesion.
- For example, one small abscess in the liver is likely to be of no significance compared to complete hepatic fibrosis associated with chronic hepatitis affecting the whole organ.
Interpretation of Lesion Colour
- The normal colour of organs and tissues is a net result of the relative amounts of:
- Parenchyma
- Connective tissue
- Blood
- Fat
- Other pigments.
- Note that dark colours can obscure changes associated with light colours.
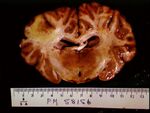
Red or red/ black
- This colouration is commonly seen with an increase in the amount of blood- may indicate
- Haemorrhage
- Significant haemorrhage is usually very dark, since the haemoglobin is depleted of oxygen.
- Congestion.
- Haemorrhage
- This colour change is most obvious in light coloured tissues due to the contrast in colour.
- Easily seen in e.g. brain and lung
- More difficult to see in e.g. spleen.
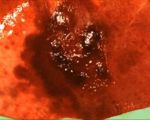
- If seen in a nodular lesion, the lesion may be
- A haematoma.
- A vascular lesion.
- An abscess with haemorrhage.
Black or Brown/ Black
- This pigmentation may be due to
- Melanin
- Exogenous carbon
- Putrefactive bacteria
- Haemosiderin.
- Examples
- If the lesion is a mass, consider a melanoma.
- A melanin-containing neoplasm.
- If the lesion is not raised, consider melanosis.
- A non-neoplastic accumulation of melanocytes.
- Common in pigmented breeds of sheep
- E.g. in tunica intima of aorta.
- Post-mortem change
- Hydrogen sulphide from gastro-intestinal bacteria can give black discolouration
- Known as pseudomelanosis
- Hydrogen sulphide from gastro-intestinal bacteria can give black discolouration
- Haemosiderosis (brown to golden brown).
- Implies old/ chronic congestion or haemorrhage.
- If the lesion is a mass, consider a melanoma.
Green
- Usually bile pigment.
- Often seen post mortem in areas of liver and intestine adjacent to the gall bladder.
- Some fungal pathogens also have a green - green/black colour.
- E.g of the respiratory tract.
Yellow
- A diffuse yellow colour may be caused by to icterus/ jaundice (due to bilirubin), or lipidosis.
- Yellow pigmentation can be given by:
- Fat
- Bile pigment (bilirubin)
- Fibrin
- Cellular exudates
- Neoplasms
White
- Similar causes as yellow pigmentation
- Exudates
- Neoplasia
- Also due to connective tissue
- Fibrous
- Cartilage
- Bone
Interpretation of Lesion Consistency
Fluid
- Fluid may be:
- Oedema
- Clear
- Serofibrinous
- Contains fibrin and implies inflammation
- Urine
- Clear
- Distinct odour
- Turbid fluid
- Cloudy
- Indicates cellular elements
- May be due to inflammation, lymphatic or neoplastic effusion.
- Blood
- Dark red.
- Recent haemorrhage into the body cavities is thick, and often contains clots.
- Serosanguinous fluid (blood tinged oedema) is often seen at necropsy.
- Is much thinner than haemorrhage, and does not contain clots.
- Oedema
- Fluid can also accumulate post-mortem.
Soft
- This is the normal consistency for many tissues
- Especially those with little stroma or which are loosely organised.
Firm
- This is normal in fluid-poor, cell-rich tissues.
- Many inflammatory or proliferative lesions will feel firm.
- Scar tissue will increase the firmness of an organ.
Hard
- Implies mineral density e.g. cartilage, bone, mineral salt deposition.
Differential Diagnosis
- In some cases, the diagnosis is straight-forward and based on the gross appearance of the lesion.
- E.g. trauma associated lesions such as a fractured femur or ruptured spleen.
- Some disease entities which have characteristic/ indicative lesions.
- The official term is "pathognomonic" lesions.
- For example:
- Muellerius capillaris and Dictyocaulus filaria (lungworm) infections in sheep
- Fascioliasis (liver fluke) in sheep and cattle.
- When the morphological appearance of a lesion is not pathognomonic, interpretation is more difficult.
- We must therefore consider what the reasonable options would be and how these different entities might be further differentiated.
- I.e. the differential diagnosis.
- We must therefore consider what the reasonable options would be and how these different entities might be further differentiated.
- An example: a solitary mass in an organ.
- Could be:
- Considering the categories for description of the lesion should allow a ‘most-likely’ identity to be reached, or at least a short list of possibilities to be made.
- Definitive diagnosis may sometimes require histology.