Difference between revisions of "Vaccines"
Jump to navigation
Jump to search
| (157 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
| − | + | {{toplink | |
| − | == | + | |backcolour = FFE4E1 |
| − | Why | + | |linkpage =WikiBlood |
| + | |linktext =WIKIBLOOD | ||
| + | |thispagemap= Vaccines(Concept Map) - WikiBlood | ||
| + | |sublink1 =Immunology - WikiBlood | ||
| + | |subtext1 =IMMUNOLOGY | ||
| + | |pagetype =Blood | ||
| + | }} | ||
| + | |||
| + | ==Why Vaccinate?== | ||
| + | |||
*To protect against infectious diseases | *To protect against infectious diseases | ||
| − | |||
| − | |||
| − | |||
| − | + | *Where there is no effective treatment once infected | |
| + | **E.g. FeLV, FIV | ||
| − | + | *Where disease is life-threatening | |
| − | + | **E.g. Canine Parvovirus | |
| − | + | *To prevent the spread of disease | |
| + | **E.g. Rabies, FMDV | ||
| − | + | ==How do we vaccinate?== | |
| − | + | *Usually by subcutaneous injection for '''systemic''' protection ([[Immunoglobulin G - WikiBlood|IgG]]) | |
| − | *Usually by subcutaneous injection for '''systemic''' protection | ||
| − | |||
| − | == | + | *For '''mucosal''' immune response, intranasal administration is best ([[Immunoglobulin A - WikiBlood|IgA]]) |
| − | [[Image:Passive Immunisation.jpg|thumb|right| | + | |
| − | + | ==What do we vaccinate with?== | |
| + | [[Image:Passive Immunisation.jpg|thumb|right|150px|Passive Immunisation - Copyright nabrown RVC]] | ||
| + | '''Passive immunisation''' | ||
| + | *Administer antibodies | ||
| + | **Maternally-derived antibodies in colostrum | ||
| + | **Antiserum (artificial) | ||
| − | |||
*Immediate protection | *Immediate protection | ||
| − | + | *Short duration of action | |
| − | *Short duration of action | + | [[Image:Active Immunisation.jpg|thumb|right|150px|Active Immunisation - Copyright nabrown RVC]] |
| − | * | + | '''Active immunisation''' |
| − | * | + | *Administer antigen so the patient develops its own antibodies to protect against disease |
| + | **Living organisms | ||
| + | **Dead organisms | ||
| + | **Toxoids | ||
| + | **Subunit antigens | ||
| + | **DNA | ||
| − | + | *Delay in protection | |
| − | * | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| + | *Often needs two or more doses | ||
| − | + | *Long duration of action | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | == | + | ==What antigen(s) do we use in the vaccine?== |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | ===Whole Organism=== | |
| − | |||
| − | + | *Live attenuated organism | |
| − | * | + | **Virulent organisms cannot be used as vaccines as they would cause disease |
| − | * | + | **Virulence is reduced by growing the organism in altered conditions so that it is less able to replicate when introduced to the host and therefore less likely to cause disease |
| − | + | *Killed inactivated organism or toxin (toxoid) | |
| − | + | **Virulent and toxic organisms cannot be used as vaccines as they would cause disease | |
| − | + | **Organisms can be killed using radiation or chemicals so that they still possess the antigens to stimulate an immune response, but the organisms are unable to replicate inside the host | |
| − | + | **Toxins are inactivated to produce a toxoid which will still have the antigens needed to produce an immune response but will not be harmful to the host | |
| + | **Needs two doses | ||
| + | |||
| + | ===Subunit Vaccine (part of the organism)=== | ||
| + | *Purified protein | ||
| + | **From lysed organisms | ||
| − | + | *Recombinant or synthetic protein | |
| − | *The | + | **The gene for the antigen required is inserted into a virus vector or cloned into bacteria |
| − | * | + | **Small antigens, such as peptides can be synthetically produced |
| − | * | ||
| − | + | *DNA coding for proteins (antigens) | |
| + | **Can be vaccinated directly into the host | ||
| − | + | ===Adjuvants=== | |
| − | + | *Used with vaccines containing inactivated organisms which alone only stimulate a weak immune response | |
| − | |||
| − | + | *Some create a depot of antigen at the injection site allowing a steady flow of antigen into the afferent lymph | |
| − | + | *Some stimulate the immune system to amplify the adaptive immune response to antigens | |
| + | **E.g. Pathogen-associated molecular patterns (PAMPs) | ||
| + | **E.g. PAMP-like adjuvants which assist naive T cell priming | ||
| − | + | *Different subtypes of T helper cells are stimulated by different adjuvants | |
| − | + | **E.g. Aluminium salts generate bias T helper II responses for '''antibody'''-mediated immunity | |
| + | **E.g. Killed mycobacteria generate IL-12 producing good '''cell'''-mediated immunity | ||
| − | + | ==Which type of vaccine is used for each disease?== | |
| − | |||
| − | |||
| − | + | *The life-cycle of the organisms needs to be understood to ascertain the best type of immune response for fighting the particular infection | |
| − | + | *A vaccine can be created to provide specific immunity which is best suited for fighting the specific infection | |
| − | |||
| − | |||
| − | == | + | ===Immunity to Virus Infection=== |
| − | |||
| − | |||
| − | + | *The virus life cycle consists of an extracellular phase, a replicative intracellular phase and another extracellular phase spreading viral particles to other cells to begin the life cycle again | |
| − | |||
| − | The virus life cycle consists of an extracellular phase, a replicative intracellular phase and another extracellular phase spreading viral particles to other cells to begin the life cycle again | ||
| − | Immunity for the extracellular phase requires neutralising | + | *Immunity for the extracellular phase requires neutralising '''antibody''' |
| − | * | + | **B cells needed |
| − | * | + | **T helper type II cells needed (for the MHC class II pathway) |
| − | *Live | + | **Live vaccine can be used |
| + | **Killed vaccine can be used | ||
| + | **Subunit vaccine can be used | ||
| − | Immunity for the intracellular phase requires | + | *Immunity for the intracellular phase requires '''CD8+ cytotoxic T cells''' |
| − | *Only live vaccine can be used to get into cells (entering via the endogenous pathway) | + | **MHC class I pathway |
| + | **Only live vaccine can be used to get into cells (entering via the endogenous pathway) | ||
===Immunity to Bacterial Infection=== | ===Immunity to Bacterial Infection=== | ||
| − | *Extracellular bacterial infection | + | *Extracellular bacterial infection need '''antibody''' production for opsonisation and to activate the complement pathways |
| − | * | + | **B cells needed |
| − | * | + | **T helper type II cells needed |
| − | Vesicular infections can only be cured by organisms being destroyed inside | + | *Vesicular infections can only be cured by organisms being destroyed inside '''macrophages''' |
| − | * | + | **T helper type I cells needed |
==When do we vaccinate?== | ==When do we vaccinate?== | ||
| − | |||
| − | |||
| − | |||
| − | * | + | *Usually when animals are young |
| − | * | + | *Breeding females so immunity is passed to offspring via the colostrum |
| + | **Protects neonates for the first 8-12 weeks of life | ||
| − | + | *Vaccination of young animals should be when the natural passive immunity decreases below the threshold for providing protection. Active immunity should then be stimulated so that the animal has constant protection. The vaccination should not be given too early, as the natural immunity can interfere with immunisation by binding and neutralising the vaccine antigens. | |
| − | |||
| − | * | + | *2 vaccines are usually given to allow for differences between neonates as the point where natural immunity decreases and active immunity needs to be stimulated, will differ between littermates and between different animals |
| − | + | ===Dog Vaccinations=== | |
| − | + | '''Diseases covered by Vaccination''' | |
| − | |||
| − | |||
| − | *[[ | + | *Canine [[Parvoviridae|Parvovirus]] |
| − | * | + | *Canine Distemper |
| − | * | + | *Canine Infectious Hepatitis |
| − | |||
| − | |||
| − | + | *Leptospirosis | |
| − | + | *Canine Parainfluenza virus | |
| − | |||
| − | |||
| − | * | + | *Kennel Cough |
| − | * | + | *Rabies |
| − | + | '''When to Vaccinate''' | |
| − | * | + | *Puppies are usually first vaccinated between 6 to 8 weeks of age |
| + | **A second vaccination is needed 2 weeks later | ||
| − | * | + | *Adult dogs need booster vaccination regularly (depending on the specific vaccination) |
| − | + | ===Cat Vaccinations=== | |
| − | |||
| − | |||
| − | |||
'''Diseases covered by Vaccination''' | '''Diseases covered by Vaccination''' | ||
| − | * | + | *Feline Infectious Enteritis |
| − | *[[ | + | *Feline Infectious Respiratory Disease 'Cat Flu' |
| + | **Feline [[Herpesviridae|Herpesvirus]] | ||
| + | **Feline [[Caliciviridae|Calicivirus]] | ||
| − | + | *Feline Leukaemia virus | |
| − | |||
| − | + | *Feline Infectious Viraemia virus | |
| − | |||
| − | * | ||
| − | * | + | *Feline Chlamydophilosis |
| − | + | '''When to Vaccinate''' | |
| − | * | + | *Kittens are usually vaccinated around 9 weeks old |
| + | **A second vaccination is needed 3 weeks later | ||
| − | * | + | *Adult cats need booster vaccination regularly (depending on the specific vaccination) |
| − | + | ===Rabbit Vaccinations=== | |
| − | + | '''Diseases covered by Vaccination''' | |
| − | + | *Viral Haemorrhagic Disease | |
| − | |||
| − | |||
| − | [ | + | *[[Poxviruses#Leporipoxviruses|Myxomatosis]] |
| − | + | '''When to Vaccinate''' | |
| − | [ | + | *Rabbits can be vaccinated against [[Poxviruses#Leporipoxviruses|Myxomatosis]] from 6 weeks of age |
| − | + | *HVD from 2½ to 3 months of age | |
| − | + | *Booster vaccinations are given every 12 months. In areas at high risk of myxomatosis, it is recommended to give myxomatosis boosters at six-monthly intervals. | |
| − | |||
==Links== | ==Links== | ||
| − | |||
| − | |||
| − | + | *[[Clinical Case 3|Myxomatosis Clinical Case]] | |
| + | |||
| + | *[[Viruses|Viruses A to Z]] | ||
| − | + | ==Creators== | |
| − | |||
| − | + | [[Natalie Brown]] | |
| − | |||
| − | |||
| − | < | + | <big><center>[[Immunology - WikiBlood|'''BACK TO IMMUNOLOGY''']]</center></big> |
| − | + | <big><center>[[Host invasion by microorganisms - WikiBlood|'''BACK TO HOST INVASION BY MICROORGANISMS''']]</center></big> | |
| − | [[ | ||
Revision as of 19:31, 4 September 2008
|
|
Why Vaccinate?
- To protect against infectious diseases
- Where there is no effective treatment once infected
- E.g. FeLV, FIV
- Where disease is life-threatening
- E.g. Canine Parvovirus
- To prevent the spread of disease
- E.g. Rabies, FMDV
How do we vaccinate?
- Usually by subcutaneous injection for systemic protection (IgG)
- For mucosal immune response, intranasal administration is best (IgA)
What do we vaccinate with?
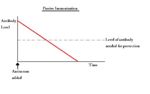
Passive immunisation
- Administer antibodies
- Maternally-derived antibodies in colostrum
- Antiserum (artificial)
- Immediate protection
- Short duration of action
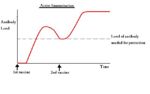
Active immunisation
- Administer antigen so the patient develops its own antibodies to protect against disease
- Living organisms
- Dead organisms
- Toxoids
- Subunit antigens
- DNA
- Delay in protection
- Often needs two or more doses
- Long duration of action
What antigen(s) do we use in the vaccine?
Whole Organism
- Live attenuated organism
- Virulent organisms cannot be used as vaccines as they would cause disease
- Virulence is reduced by growing the organism in altered conditions so that it is less able to replicate when introduced to the host and therefore less likely to cause disease
- Killed inactivated organism or toxin (toxoid)
- Virulent and toxic organisms cannot be used as vaccines as they would cause disease
- Organisms can be killed using radiation or chemicals so that they still possess the antigens to stimulate an immune response, but the organisms are unable to replicate inside the host
- Toxins are inactivated to produce a toxoid which will still have the antigens needed to produce an immune response but will not be harmful to the host
- Needs two doses
Subunit Vaccine (part of the organism)
- Purified protein
- From lysed organisms
- Recombinant or synthetic protein
- The gene for the antigen required is inserted into a virus vector or cloned into bacteria
- Small antigens, such as peptides can be synthetically produced
- DNA coding for proteins (antigens)
- Can be vaccinated directly into the host
Adjuvants
- Used with vaccines containing inactivated organisms which alone only stimulate a weak immune response
- Some create a depot of antigen at the injection site allowing a steady flow of antigen into the afferent lymph
- Some stimulate the immune system to amplify the adaptive immune response to antigens
- E.g. Pathogen-associated molecular patterns (PAMPs)
- E.g. PAMP-like adjuvants which assist naive T cell priming
- Different subtypes of T helper cells are stimulated by different adjuvants
- E.g. Aluminium salts generate bias T helper II responses for antibody-mediated immunity
- E.g. Killed mycobacteria generate IL-12 producing good cell-mediated immunity
Which type of vaccine is used for each disease?
- The life-cycle of the organisms needs to be understood to ascertain the best type of immune response for fighting the particular infection
- A vaccine can be created to provide specific immunity which is best suited for fighting the specific infection
Immunity to Virus Infection
- The virus life cycle consists of an extracellular phase, a replicative intracellular phase and another extracellular phase spreading viral particles to other cells to begin the life cycle again
- Immunity for the extracellular phase requires neutralising antibody
- B cells needed
- T helper type II cells needed (for the MHC class II pathway)
- Live vaccine can be used
- Killed vaccine can be used
- Subunit vaccine can be used
- Immunity for the intracellular phase requires CD8+ cytotoxic T cells
- MHC class I pathway
- Only live vaccine can be used to get into cells (entering via the endogenous pathway)
Immunity to Bacterial Infection
- Extracellular bacterial infection need antibody production for opsonisation and to activate the complement pathways
- B cells needed
- T helper type II cells needed
- Vesicular infections can only be cured by organisms being destroyed inside macrophages
- T helper type I cells needed
When do we vaccinate?
- Usually when animals are young
- Breeding females so immunity is passed to offspring via the colostrum
- Protects neonates for the first 8-12 weeks of life
- Vaccination of young animals should be when the natural passive immunity decreases below the threshold for providing protection. Active immunity should then be stimulated so that the animal has constant protection. The vaccination should not be given too early, as the natural immunity can interfere with immunisation by binding and neutralising the vaccine antigens.
- 2 vaccines are usually given to allow for differences between neonates as the point where natural immunity decreases and active immunity needs to be stimulated, will differ between littermates and between different animals
Dog Vaccinations
Diseases covered by Vaccination
- Canine Parvovirus
- Canine Distemper
- Canine Infectious Hepatitis
- Leptospirosis
- Canine Parainfluenza virus
- Kennel Cough
- Rabies
When to Vaccinate
- Puppies are usually first vaccinated between 6 to 8 weeks of age
- A second vaccination is needed 2 weeks later
- Adult dogs need booster vaccination regularly (depending on the specific vaccination)
Cat Vaccinations
Diseases covered by Vaccination
- Feline Infectious Enteritis
- Feline Infectious Respiratory Disease 'Cat Flu'
- Feline Herpesvirus
- Feline Calicivirus
- Feline Leukaemia virus
- Feline Infectious Viraemia virus
- Feline Chlamydophilosis
When to Vaccinate
- Kittens are usually vaccinated around 9 weeks old
- A second vaccination is needed 3 weeks later
- Adult cats need booster vaccination regularly (depending on the specific vaccination)
Rabbit Vaccinations
Diseases covered by Vaccination
- Viral Haemorrhagic Disease
When to Vaccinate
- Rabbits can be vaccinated against Myxomatosis from 6 weeks of age
- HVD from 2½ to 3 months of age
- Booster vaccinations are given every 12 months. In areas at high risk of myxomatosis, it is recommended to give myxomatosis boosters at six-monthly intervals.