Difference between revisions of "CNS Response to Injury - Pathology"
Jump to navigation
Jump to search
(Redirected page to Category:Central Nervous System - Response to Injury) |
|||
| (11 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
| − | # | + | {{toplink |
| + | |backcolour = E0EEEE | ||
| + | |linkpage = Nervous System - Pathology | ||
| + | |linktext =Nervous System | ||
| + | |maplink = Nervous System (Content Map) - Pathology | ||
| + | |pagetype =Pathology | ||
| + | }} | ||
| + | <br> | ||
| + | ==Introduction== | ||
| + | |||
| + | * The CNS is composed of two major cell types: | ||
| + | *# Neurons | ||
| + | *# Glial cells, which include: | ||
| + | *#* Astrocytes | ||
| + | *#* Oligodendrocytes | ||
| + | *#* Microglial cells | ||
| + | *#* Ependymal cells | ||
| + | *#* Choroid plexus epithelial cells | ||
| + | * The response to injury varies with the cell type injured. | ||
| + | |||
| + | ==Response of Neurons to Injury== | ||
| + | |||
| + | * Neurons are particularly vulnerable to injury, due to their: | ||
| + | ** High metabolic rate | ||
| + | ** Small capacity to store energy | ||
| + | ** Lack of regenerative ability | ||
| + | ** Axons being very dependent on the cell body. | ||
| + | *** Axons cannot make their own protein as they have no Nissl substance. | ||
| + | *** The cell body produces the axon's protein and disposes of its waste. | ||
| + | *** Death or damage of the cell body causes axon degeneration. | ||
| + | |||
| + | * There are four ways in which neurons may react to insult: | ||
| + | *# Acute Necrosis | ||
| + | *# Chromatolysis | ||
| + | *# Wallerian Degeneration | ||
| + | *# Vacuolation | ||
| + | |||
| + | ===Acute Necrosis=== | ||
| + | |||
| + | * Acute necrosis is the most common neuronal response to injury. | ||
| + | * Causes of actue necrosis include: | ||
| + | ** Ischaemia | ||
| + | *** Diminution of the blood supply causes a lack of nutrients and oxygen, inhibiting energy production. A decrease in the levels of ATP leads to: | ||
| + | ***# Failure of the Na<sup>+</sup>/K<sup>+</sup>pumps, causing cell swelling and an increase in extracellular potassium. | ||
| + | ***# Failure to generate NAD required for DNA repair. | ||
| + | ** Hypoxia | ||
| + | ** Hypoglycaemia | ||
| + | ** Toxins, such as lead and mercury | ||
| + | |||
| + | ====Laminar Cortical Necrosis==== | ||
| + | |||
| + | * Laminar cortical necrosis refers to the selective destruction of neurons in the deeper layers of the cerebral cortex. | ||
| + | ** These neurons are the most sensitive to hypoxia. | ||
| + | * The laminar cortical pattern of acute necrosis occurs in several instances: | ||
| + | *# Ischaemia | ||
| + | *#* For example, seizure-related ischaemia in dogs. | ||
| + | *# Polioencephalomalacia in ruminants | ||
| + | *#* Also called cerebrocortical necrosis or CCN. | ||
| + | *# Salt poisoning in swine | ||
| + | *# Lead poisoning in cattle | ||
| + | * It is most likely that gross changes will not be seen. When they are visible, changes may be apparent as: | ||
| + | ** Oedema | ||
| + | *** Causes brain swelling, flattened gyri and herniation | ||
| + | ** A thin, white, glistening line along the middle of the cortex. | ||
| + | *** In ruminants, this fluoresces with UV-light. | ||
| + | * Ultimately the cortex becomes necrotic and collapses. | ||
| + | |||
| + | [http://w3.vet.cornell.edu/nst/nst.asp?Fun=F_KSsrch&kw=POLIOENCEPHALOMALACIA View images courtesy of Cornell Veterinary Medicine] | ||
| + | |||
| + | ===Chromatolysis=== | ||
| + | |||
| + | * Chromatolysis is the cell body’s reaction to axonal insult. | ||
| + | * The cell body swells and the Nissl substance disperses. | ||
| + | ** Dispersal of the Nissl substance allows the cell body to produce proteins for rebuilding the axon. | ||
| + | * IT IS NOT A FORM OF NECROSIS. | ||
| + | ** It is an adaptive response to deal with the injury. | ||
| + | ** It can, however lead to necrosis. | ||
| + | * Seen, for example, in grass sickness in [[Hindgut Fermenters - Horse - Anatomy & Physiology|horses]] (equine dysautonomia). | ||
| + | |||
| + | [http://w3.vet.cornell.edu/nst/nst.asp?Fun=Display&imgID=13353 View images courtesy of Cornell Veterinary Medicine] | ||
| + | |||
| + | ===Wallerian Degeneration=== | ||
| + | |||
| + | * Wallerian degeneration is the axon’s reaction to insult. | ||
| + | * The axon and its myelin sheath degenerates distal to the point of injury. | ||
| + | * There are several causes of wallerian degeneration: | ||
| + | ** Axonal transection | ||
| + | *** This is the "classic" cause | ||
| + | ** Vascular causes | ||
| + | ** Inflamatory reactions | ||
| + | ** Toxic insult | ||
| + | ** As a sequel to neuronal cell death. | ||
| + | |||
| + | [http://w3.vet.cornell.edu/nst/nst.asp?Fun=F_KSsrch&kw=WALLERIAN View images courtesy of Cornell Veterinary Medicine] | ||
| + | |||
| + | ====The Process of Wallerian Degeneration==== | ||
| + | |||
| + | # '''Axonal Degeneration''' | ||
| + | #* Axonal injuries initially lead to acute axonal degeneration. | ||
| + | #** The proximal and distal ends separate within 30 minutes of injury. | ||
| + | #* Degeneration and swelling of the axolemma eventually leads to formation of bead-like particles. | ||
| + | #* After the membrane is degraded, the organelles and cytoskeleton disintegrate. | ||
| + | #** Larger axons require longer time for cytoskeleton degradation and thus take a longer time to degenerate. | ||
| + | # '''Myelin Clearance''' | ||
| + | #* Following axonal degeneration, myelin debris is cleared by phagocytosis. | ||
| + | #* Myelin clearance in the PNS is much faster and efficient that in the CNS. This is due to: | ||
| + | #** The actions of schwann cells in the PNS. | ||
| + | #** Differences in changes in the blood-brain barrier in each system. | ||
| + | #*** In the PNS, the permeability increases throughout the distal stump. | ||
| + | #*** Barrier disruption in CNS is limited to the site of injury. | ||
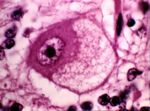
| + | # '''Regeneration''' [[Image:neuronalvacuolation1.jpg|thumb|right|150px|Neuronal vacuolation. Image courtesy of BioMed Archive]] | ||
| + | #* Regeneration is rapid in the PNS. | ||
| + | #** Schwann cells release growth factors to support regeneration. | ||
| + | #* CNS regeneration is much slower, and is almost absent in most species. | ||
| + | #** This is due to: | ||
| + | #*** Slow or absent phagocytosis | ||
| + | #*** Little or no axonal regeneration, because: | ||
| + | #**** Oligodendrocytes have little capacity for remyelination compared to Schwann cells. | ||
| + | #**** There is no basal lamina scaffold to support a new axonal sprout. | ||
| + | #**** The debris from central myelin inhibits axonal sprouting. | ||
| + | |||
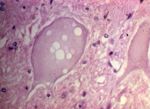
| + | ===Vacuolation=== | ||
| + | [[Image:neuronalvacuolation2.jpg|thumb|right|150px|Neuronal vacuolation. Image courtesy of BioMed Archive]] | ||
| + | * Vacuolation is the hallmark of transmissible spongiform encephalopathies. | ||
| + | ** For example, BSE and Scrapie. | ||
| + | * Vacuolation can also occur under other circumstances: | ||
| + | ** Artefact of fixation | ||
| + | ** Toxicoses | ||
| + | ** It may sometimes be a normal feature. | ||
| + | |||
| + | ==Glial Cell Response to Injury== | ||
| + | |||
| + | * The order of susceptibility of CNS cells to injury runs, from most to least susceptible: | ||
| + | *# Neurons | ||
| + | *# Oligodendroglia | ||
| + | *# Astrocytes | ||
| + | *# Microglia | ||
| + | *# Endothelial cells | ||
| + | |||
| + | ===Astrocytes=== | ||
| + | |||
| + | * The response of astrocytes to insult include: | ||
| + | ** '''Necrosis''' | ||
| + | ** '''Astrocytosis''' | ||
| + | *** An increase in the number of astrocytes (i.e. astrocyte hyperplasia). | ||
| + | ** '''Astrogliosis''' | ||
| + | *** An increase in the size of astrocytes (i.e. astrocyte hypertrophy). | ||
| + | ** '''Gliosis''' | ||
| + | *** Formation of glial fibres. | ||
| + | *** This is a form of scarring in the CNS. | ||
| + | |||
| + | ===Oligodendrocytes=== | ||
| + | |||
| + | * Oligodendrocytes are prone to hypoxia and degeneration | ||
| + | * Oligodendrocytes proliferate around damaged neurons. | ||
| + | ** This is known as '''satellitosis'''. | ||
| + | * Death of oligodendrocytes causes demyelination. | ||
| + | |||
| + | ===Microglial Cells=== | ||
| + | |||
| + | * Microglial cells can respond in two ways to CNS injury. | ||
| + | *# They may phagocytose cell debris to transform to gitter cells. | ||
| + | *#* Gitter cells are large macrophages with foamy cytoplasm. [http://w3.vet.cornell.edu/nst/nst.asp?Fun=F_KSsrch&kw=GITTER View images courtesy of Cornell Veterinary Medicine] | ||
| + | *# They may form glial nodules. | ||
| + | *#* These are small nodules that occur notably in viral diseases. | ||
| + | |||
| + | ==General Responses to Injury== | ||
| + | |||
| + | ===Ischaemic Damage=== | ||
| + | |||
| + | * The CNS is particularly sensitive to ischaemia, because it has few energy reserves. | ||
| + | * The CNS is protected by its bony covering. | ||
| + | ** Despite offering protection, the covering also makes the CNS vulnerable to certain types of damage, for example: | ||
| + | *** Damage due to fractures and dislocation. | ||
| + | *** Damage due to raised intracranial pressure. | ||
| + | **** Raised intracranial stimulates a compensatory increase in blood flow, further raising intracranial pressure. This stimulates a further increase in blood flow, and the cycle continues until intracranial pressure is so high that blood flow is impeded. | ||
| + | ***** The result of this is '''ischaemia'''. | ||
| + | * Survival of any cell is dependent on having sufficient energy. | ||
| + | ** Ischaemia causes cell death by impeding energy supply to cells. | ||
| + | *** Cells directly affected by ischamia die rapidly. | ||
| + | **** For example, those suffering a failure of pefusion due to an infarct. | ||
| + | *** Neurons surrounding this area of complete and rapid cell death exist under sub-optimal conditions and die over a more prolonged period. | ||
| + | **** This area of gradual death is known as the '''lesion penumbra'''. | ||
| + | **** There are several mechanisms implicated in cell death in the penumbra: | ||
| + | ****# Increase in intracellular calcium | ||
| + | ****# Failure to control free radicals | ||
| + | ****# Generation of nitrogen species (e.g NO and ONOO) are the main damaging events. | ||
| + | |||
| + | ===Oedema=== | ||
| + | |||
| + | * There are three types of cerebral oedema: | ||
| + | *# '''Vasogenic oedema''' | ||
| + | *#* Vasogenic oedema follows vascular injury. | ||
| + | *#* Oedema fluid gathers outside of the cell. | ||
| + | *#* This is the most common variation of cerebral oedema. | ||
| + | *# '''Cytotoxic oedema''' | ||
| + | *#* Cytotoxic oedema is due to an energy deficit. | ||
| + | *#** The neuron can’t pump out sodium and water leading to swelling within the cell. | ||
| + | *# '''Interstitial oedema''' | ||
| + | *#* Associated with hydrocephalus. | ||
| + | *#* This type of cerebral oedema is of lesser importance. | ||
| + | * One serious consequence of oedema is that the increase in size leads to the brain trying to escape the skull. | ||
| + | ** This causes herniation of the brain tissue. | ||
| + | ** The most common site of herniation is at the foramen magnum. | ||
| + | *** The medulla is compressed at the site of the respiratory centres, leading to death. | ||
| + | |||
| + | ===Demyelination=== | ||
| + | |||
| + | * Demyelination is the loss of initially normal myelin from the axon. | ||
| + | * Demyelination may be primary or secondary. | ||
| + | |||
| + | ====Primary Demyelination==== | ||
| + | |||
| + | * Normally formed myelin is selectively destroyed; however, the axon remains intact. | ||
| + | * Causes of primary demyelination: | ||
| + | ** Toxins, such as hexachlorophene or triethyl tin. | ||
| + | ** Oedema | ||
| + | ** Immune-mediated demyelination | ||
| + | ** Infectious diseases, for example canine distemper or caprine arthritis/encephalitis. | ||
| + | |||
| + | ====Secondary Demyelination==== | ||
| + | |||
| + | * Myelin is lost following damage to the axon. | ||
| + | ** I.e. in [[CNS Response to Injury - Pathology#Wallerian Degeneration|wallerian degeneration]] | ||
| + | |||
| + | ===Vascular Diseases=== | ||
| + | |||
| + | * Vascular diseases can lead to complete or partial blockage of blood flow which leads to ischaemia. | ||
| + | ** Consequences of ischaemia depend on: | ||
| + | **# Duration and degree of ischaemia | ||
| + | **# Size and type of vessel involved | ||
| + | **# Susceptibility of the tissue to hypoxia | ||
| + | * Potential outcomes of vascular blockage include: | ||
| + | ** Infarct, and | ||
| + | ** Necrosis of tissue following obstruction of its blood supply. | ||
| + | * Causes include: | ||
| + | ** Thrombosis | ||
| + | *** Uncommon in animals but may be seen with DIC or sepsis. | ||
| + | ** Embolism. e.g. | ||
| + | *** Bone marrow emboli following trauma or fractures in dogs | ||
| + | *** Fibrocartilaginous embolic myelopathy | ||
| + | ** Vasculitis, e.g. | ||
| + | *** Hog cholera (pestivirus) | ||
| + | *** Malignant catarrhal fever (herpesvirus) | ||
| + | *** Oedema disease (angiopathy caused by E.coli toxin) | ||
| + | |||
| + | ===Malacia=== | ||
| + | |||
| + | * Malacia may be used: | ||
| + | ** As a gross term, meaning "softening" | ||
| + | ** As a microscopic term, meaning "necrosis" | ||
| + | * Malacia occurs in: | ||
| + | ** Infarcted tissue | ||
| + | ** Vascular injury, for example vasculitis. | ||
| + | ** Reduced blood flow or hypoxia, e.g. | ||
| + | *** Carbon monoxide poisoning, which alters hemoglobin function | ||
| + | *** Cyanide poisoning, which inhibits tissue respiration | ||
| + | |||
| + | ==Excitotoxicity== | ||
| + | |||
| + | * The term "excitotoxicity" is used to describe the process by which neurons are damaged by glutamate and other similar substances. | ||
| + | * Excitotoxicity results from the overactivation of excitatory receptor activation. | ||
| + | |||
| + | ===The Mechanism of Excitotoxicity=== | ||
| + | |||
| + | * '''Glutamate''' is the major excitatory transmitter in the brain and spinal cord. | ||
| + | ** There are four classes of postsynaptic glutamate receptors for glutamate. | ||
| + | *** The receptors are either: | ||
| + | **** Directly or indirectly associated with gated ion channels, '''OR''' | ||
| + | **** Activators of second messenger systems that result in release of calcium from intracellular stores. | ||
| + | *** The receptors are named according to their phamacological agonists: | ||
| + | **** '''NMDA receptor''' | ||
| + | ***** The NMDA receptor is directly linked to a gated ion channel. | ||
| + | ***** The ion channel is permeable to Ca<sup>++</sup>, as well as Na<sup>+</sup> and K<sup>+</sup>. | ||
| + | ***** The channel is also voltage dependent. | ||
| + | ****** It is blocked in the resting state by extracellular Mg<sup>++</sup>, which is removed when membrane is depolarised. | ||
| + | ***** I.e. both glutamate and depolarisation are needed to open the channel. | ||
| + | **** '''AMPA receptor''' | ||
| + | ***** The AMPA receptor is directly linked to a gated ion channel. | ||
| + | ***** The channel is permeable to Na<sup>+</sup> and K<sup>+</sup> but NOT to divalent cations. | ||
| + | ***** The receptor binds the glutamate agonist, AMPA, but is not affected by NMDA. | ||
| + | ***** The receptor probably underlies fast excitatory transmission at glutamatergic synapses. | ||
| + | **** '''Kainate receptor''' | ||
| + | ***** Kainate receptors work in the same way as AMPA receptors, and also contribute to fast excitatory transmission. | ||
| + | **** '''mGluR''', the '''metabotropic receptor''' | ||
| + | ***** Metabotropic receptors are indirectly linked to a channel permeable to Na<sup>+</sup> and K<sup>+</sup>. | ||
| + | ***** They also activate a phoshoinositide-linked second messenger system, leading to mobilisation of intra-cellular Ca<sup>++</sup> stores. | ||
| + | ***** The physiological role ot mGluR is not understood. | ||
| + | |||
| + | * Under normal circumstances, a series of glutamate transporters rapidly clear glutamate from the extracellular space. | ||
| + | ** Some of these transporters are neuronal; others are found on astrocytes. | ||
| + | * This normal homeostatic mechanism fails under a variety of conditions, such as ischaemia and glucose deprivation. | ||
| + | ** This results in a rise in extracellular glutamate, causing activation of the neuronal glutamate receptors. | ||
| + | * Two distinct events of excitiotoxicity arise from glutamate receptor activation: | ||
| + | *# The depolarisation caused mediates an influx of Na<sup>+</sup>, Cl<sup>-</sup> and water. This give '''acute neuronal swelling''', which is reversible. | ||
| + | *# There is a '''rise in intracellular Ca<sup>++</sup>'''. | ||
| + | *#* This is due to: | ||
| + | *#** Excessive direct Ca<sup>++</sup> influx via the NMDA receptor-linked channels | ||
| + | *#** Ca<sup>++</sup> influx through voltage gated calcium channels following depolarisation of the neuron via non-NDMA receptors | ||
| + | *#** Release of Ca<sup>++</sup> from intracellular stores. | ||
| + | *#* The rise in neuronal intracellular Ca<sup>2+</sup> serves to: | ||
| + | *#** Uncouple mitochondrial electron transport and activate nitric oxide synthase and phospholipase A, leading to generation of reactive oxygen and nitrogen species which damage the neurone. | ||
| + | *#** Activats a number of enzymes, including phospholipases, endonucleases, and proteases. | ||
| + | *#*** These enzymes go on to damage cell structures such as components of the cytoskeleton, membrane, and DNA. | ||
| + | * Excitotoxicity is, therefore, a cause of acute neuron death. | ||
Revision as of 09:33, 5 September 2008
|
|
Introduction
- The CNS is composed of two major cell types:
- Neurons
- Glial cells, which include:
- Astrocytes
- Oligodendrocytes
- Microglial cells
- Ependymal cells
- Choroid plexus epithelial cells
- The response to injury varies with the cell type injured.
Response of Neurons to Injury
- Neurons are particularly vulnerable to injury, due to their:
- High metabolic rate
- Small capacity to store energy
- Lack of regenerative ability
- Axons being very dependent on the cell body.
- Axons cannot make their own protein as they have no Nissl substance.
- The cell body produces the axon's protein and disposes of its waste.
- Death or damage of the cell body causes axon degeneration.
- There are four ways in which neurons may react to insult:
- Acute Necrosis
- Chromatolysis
- Wallerian Degeneration
- Vacuolation
Acute Necrosis
- Acute necrosis is the most common neuronal response to injury.
- Causes of actue necrosis include:
- Ischaemia
- Diminution of the blood supply causes a lack of nutrients and oxygen, inhibiting energy production. A decrease in the levels of ATP leads to:
- Failure of the Na+/K+pumps, causing cell swelling and an increase in extracellular potassium.
- Failure to generate NAD required for DNA repair.
- Diminution of the blood supply causes a lack of nutrients and oxygen, inhibiting energy production. A decrease in the levels of ATP leads to:
- Hypoxia
- Hypoglycaemia
- Toxins, such as lead and mercury
- Ischaemia
Laminar Cortical Necrosis
- Laminar cortical necrosis refers to the selective destruction of neurons in the deeper layers of the cerebral cortex.
- These neurons are the most sensitive to hypoxia.
- The laminar cortical pattern of acute necrosis occurs in several instances:
- Ischaemia
- For example, seizure-related ischaemia in dogs.
- Polioencephalomalacia in ruminants
- Also called cerebrocortical necrosis or CCN.
- Salt poisoning in swine
- Lead poisoning in cattle
- Ischaemia
- It is most likely that gross changes will not be seen. When they are visible, changes may be apparent as:
- Oedema
- Causes brain swelling, flattened gyri and herniation
- A thin, white, glistening line along the middle of the cortex.
- In ruminants, this fluoresces with UV-light.
- Oedema
- Ultimately the cortex becomes necrotic and collapses.
View images courtesy of Cornell Veterinary Medicine
Chromatolysis
- Chromatolysis is the cell body’s reaction to axonal insult.
- The cell body swells and the Nissl substance disperses.
- Dispersal of the Nissl substance allows the cell body to produce proteins for rebuilding the axon.
- IT IS NOT A FORM OF NECROSIS.
- It is an adaptive response to deal with the injury.
- It can, however lead to necrosis.
- Seen, for example, in grass sickness in horses (equine dysautonomia).
View images courtesy of Cornell Veterinary Medicine
Wallerian Degeneration
- Wallerian degeneration is the axon’s reaction to insult.
- The axon and its myelin sheath degenerates distal to the point of injury.
- There are several causes of wallerian degeneration:
- Axonal transection
- This is the "classic" cause
- Vascular causes
- Inflamatory reactions
- Toxic insult
- As a sequel to neuronal cell death.
- Axonal transection
View images courtesy of Cornell Veterinary Medicine
The Process of Wallerian Degeneration
- Axonal Degeneration
- Axonal injuries initially lead to acute axonal degeneration.
- The proximal and distal ends separate within 30 minutes of injury.
- Degeneration and swelling of the axolemma eventually leads to formation of bead-like particles.
- After the membrane is degraded, the organelles and cytoskeleton disintegrate.
- Larger axons require longer time for cytoskeleton degradation and thus take a longer time to degenerate.
- Axonal injuries initially lead to acute axonal degeneration.
- Myelin Clearance
- Following axonal degeneration, myelin debris is cleared by phagocytosis.
- Myelin clearance in the PNS is much faster and efficient that in the CNS. This is due to:
- The actions of schwann cells in the PNS.
- Differences in changes in the blood-brain barrier in each system.
- In the PNS, the permeability increases throughout the distal stump.
- Barrier disruption in CNS is limited to the site of injury.
- Regeneration
- Regeneration is rapid in the PNS.
- Schwann cells release growth factors to support regeneration.
- CNS regeneration is much slower, and is almost absent in most species.
- This is due to:
- Slow or absent phagocytosis
- Little or no axonal regeneration, because:
- Oligodendrocytes have little capacity for remyelination compared to Schwann cells.
- There is no basal lamina scaffold to support a new axonal sprout.
- The debris from central myelin inhibits axonal sprouting.
- This is due to:
- Regeneration is rapid in the PNS.
Vacuolation
- Vacuolation is the hallmark of transmissible spongiform encephalopathies.
- For example, BSE and Scrapie.
- Vacuolation can also occur under other circumstances:
- Artefact of fixation
- Toxicoses
- It may sometimes be a normal feature.
Glial Cell Response to Injury
- The order of susceptibility of CNS cells to injury runs, from most to least susceptible:
- Neurons
- Oligodendroglia
- Astrocytes
- Microglia
- Endothelial cells
Astrocytes
- The response of astrocytes to insult include:
- Necrosis
- Astrocytosis
- An increase in the number of astrocytes (i.e. astrocyte hyperplasia).
- Astrogliosis
- An increase in the size of astrocytes (i.e. astrocyte hypertrophy).
- Gliosis
- Formation of glial fibres.
- This is a form of scarring in the CNS.
Oligodendrocytes
- Oligodendrocytes are prone to hypoxia and degeneration
- Oligodendrocytes proliferate around damaged neurons.
- This is known as satellitosis.
- Death of oligodendrocytes causes demyelination.
Microglial Cells
- Microglial cells can respond in two ways to CNS injury.
- They may phagocytose cell debris to transform to gitter cells.
- Gitter cells are large macrophages with foamy cytoplasm. View images courtesy of Cornell Veterinary Medicine
- They may form glial nodules.
- These are small nodules that occur notably in viral diseases.
- They may phagocytose cell debris to transform to gitter cells.
General Responses to Injury
Ischaemic Damage
- The CNS is particularly sensitive to ischaemia, because it has few energy reserves.
- The CNS is protected by its bony covering.
- Despite offering protection, the covering also makes the CNS vulnerable to certain types of damage, for example:
- Damage due to fractures and dislocation.
- Damage due to raised intracranial pressure.
- Raised intracranial stimulates a compensatory increase in blood flow, further raising intracranial pressure. This stimulates a further increase in blood flow, and the cycle continues until intracranial pressure is so high that blood flow is impeded.
- The result of this is ischaemia.
- Raised intracranial stimulates a compensatory increase in blood flow, further raising intracranial pressure. This stimulates a further increase in blood flow, and the cycle continues until intracranial pressure is so high that blood flow is impeded.
- Despite offering protection, the covering also makes the CNS vulnerable to certain types of damage, for example:
- Survival of any cell is dependent on having sufficient energy.
- Ischaemia causes cell death by impeding energy supply to cells.
- Cells directly affected by ischamia die rapidly.
- For example, those suffering a failure of pefusion due to an infarct.
- Neurons surrounding this area of complete and rapid cell death exist under sub-optimal conditions and die over a more prolonged period.
- This area of gradual death is known as the lesion penumbra.
- There are several mechanisms implicated in cell death in the penumbra:
- Increase in intracellular calcium
- Failure to control free radicals
- Generation of nitrogen species (e.g NO and ONOO) are the main damaging events.
- Cells directly affected by ischamia die rapidly.
- Ischaemia causes cell death by impeding energy supply to cells.
Oedema
- There are three types of cerebral oedema:
- Vasogenic oedema
- Vasogenic oedema follows vascular injury.
- Oedema fluid gathers outside of the cell.
- This is the most common variation of cerebral oedema.
- Cytotoxic oedema
- Cytotoxic oedema is due to an energy deficit.
- The neuron can’t pump out sodium and water leading to swelling within the cell.
- Cytotoxic oedema is due to an energy deficit.
- Interstitial oedema
- Associated with hydrocephalus.
- This type of cerebral oedema is of lesser importance.
- Vasogenic oedema
- One serious consequence of oedema is that the increase in size leads to the brain trying to escape the skull.
- This causes herniation of the brain tissue.
- The most common site of herniation is at the foramen magnum.
- The medulla is compressed at the site of the respiratory centres, leading to death.
Demyelination
- Demyelination is the loss of initially normal myelin from the axon.
- Demyelination may be primary or secondary.
Primary Demyelination
- Normally formed myelin is selectively destroyed; however, the axon remains intact.
- Causes of primary demyelination:
- Toxins, such as hexachlorophene or triethyl tin.
- Oedema
- Immune-mediated demyelination
- Infectious diseases, for example canine distemper or caprine arthritis/encephalitis.
Secondary Demyelination
- Myelin is lost following damage to the axon.
- I.e. in wallerian degeneration
Vascular Diseases
- Vascular diseases can lead to complete or partial blockage of blood flow which leads to ischaemia.
- Consequences of ischaemia depend on:
- Duration and degree of ischaemia
- Size and type of vessel involved
- Susceptibility of the tissue to hypoxia
- Consequences of ischaemia depend on:
- Potential outcomes of vascular blockage include:
- Infarct, and
- Necrosis of tissue following obstruction of its blood supply.
- Causes include:
- Thrombosis
- Uncommon in animals but may be seen with DIC or sepsis.
- Embolism. e.g.
- Bone marrow emboli following trauma or fractures in dogs
- Fibrocartilaginous embolic myelopathy
- Vasculitis, e.g.
- Hog cholera (pestivirus)
- Malignant catarrhal fever (herpesvirus)
- Oedema disease (angiopathy caused by E.coli toxin)
- Thrombosis
Malacia
- Malacia may be used:
- As a gross term, meaning "softening"
- As a microscopic term, meaning "necrosis"
- Malacia occurs in:
- Infarcted tissue
- Vascular injury, for example vasculitis.
- Reduced blood flow or hypoxia, e.g.
- Carbon monoxide poisoning, which alters hemoglobin function
- Cyanide poisoning, which inhibits tissue respiration
Excitotoxicity
- The term "excitotoxicity" is used to describe the process by which neurons are damaged by glutamate and other similar substances.
- Excitotoxicity results from the overactivation of excitatory receptor activation.
The Mechanism of Excitotoxicity
- Glutamate is the major excitatory transmitter in the brain and spinal cord.
- There are four classes of postsynaptic glutamate receptors for glutamate.
- The receptors are either:
- Directly or indirectly associated with gated ion channels, OR
- Activators of second messenger systems that result in release of calcium from intracellular stores.
- The receptors are named according to their phamacological agonists:
- NMDA receptor
- The NMDA receptor is directly linked to a gated ion channel.
- The ion channel is permeable to Ca++, as well as Na+ and K+.
- The channel is also voltage dependent.
- It is blocked in the resting state by extracellular Mg++, which is removed when membrane is depolarised.
- I.e. both glutamate and depolarisation are needed to open the channel.
- AMPA receptor
- The AMPA receptor is directly linked to a gated ion channel.
- The channel is permeable to Na+ and K+ but NOT to divalent cations.
- The receptor binds the glutamate agonist, AMPA, but is not affected by NMDA.
- The receptor probably underlies fast excitatory transmission at glutamatergic synapses.
- Kainate receptor
- Kainate receptors work in the same way as AMPA receptors, and also contribute to fast excitatory transmission.
- mGluR, the metabotropic receptor
- Metabotropic receptors are indirectly linked to a channel permeable to Na+ and K+.
- They also activate a phoshoinositide-linked second messenger system, leading to mobilisation of intra-cellular Ca++ stores.
- The physiological role ot mGluR is not understood.
- NMDA receptor
- The receptors are either:
- There are four classes of postsynaptic glutamate receptors for glutamate.
- Under normal circumstances, a series of glutamate transporters rapidly clear glutamate from the extracellular space.
- Some of these transporters are neuronal; others are found on astrocytes.
- This normal homeostatic mechanism fails under a variety of conditions, such as ischaemia and glucose deprivation.
- This results in a rise in extracellular glutamate, causing activation of the neuronal glutamate receptors.
- Two distinct events of excitiotoxicity arise from glutamate receptor activation:
- The depolarisation caused mediates an influx of Na+, Cl- and water. This give acute neuronal swelling, which is reversible.
- There is a rise in intracellular Ca++.
- This is due to:
- Excessive direct Ca++ influx via the NMDA receptor-linked channels
- Ca++ influx through voltage gated calcium channels following depolarisation of the neuron via non-NDMA receptors
- Release of Ca++ from intracellular stores.
- The rise in neuronal intracellular Ca2+ serves to:
- Uncouple mitochondrial electron transport and activate nitric oxide synthase and phospholipase A, leading to generation of reactive oxygen and nitrogen species which damage the neurone.
- Activats a number of enzymes, including phospholipases, endonucleases, and proteases.
- These enzymes go on to damage cell structures such as components of the cytoskeleton, membrane, and DNA.
- This is due to:
- Excitotoxicity is, therefore, a cause of acute neuron death.