Difference between revisions of "Oesophageal Foreign Body"
TestStudent (talk | contribs) |
|||
| (15 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
| − | {{ | + | {{review}} |
| − | == | + | |
| − | + | {{cat}} | |
| + | {{dog}} | ||
| + | |||
| + | ==Typical Signalment== | ||
| + | *Any age group can be affected | ||
| + | *Can occur in cats or dogs | ||
| + | *Dogs more commonly affected due to their less discriminating eating habits | ||
| + | |||
| + | ==Description== | ||
| + | Almost anything can become lodged in the oesophagus. Objects with sharp points are very common and include: | ||
| + | *bones | ||
| + | *fish hooks | ||
| + | *needles | ||
| + | *sticks | ||
| + | *toys | ||
| − | + | The most common foreign bodies found in dogs are bones, bone fragments and coins. In cats play objects are most common. Many foreign objects are regurgitated or are transported through the gastrointestinal tract. Those that are too large to pass through the oesophagus remain lodged causing mechanical obstruction. | |
| − | + | Common sites of obstruction: | |
| + | *thoracic inlet | ||
| + | *base of the heart | ||
| + | *immediately in front of the diaphragm | ||
| − | + | The severity of oesophageal damage is dependent on the size, angularity or sharp pointedness of the foreign body as well as the duration of obstruction. | |
| − | |||
==Diagnosis== | ==Diagnosis== | ||
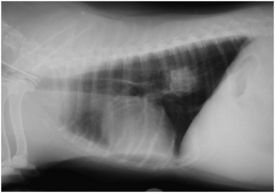
| − | [[Image:Oesophageal Foreign Body.jpg|thumb|right|275px| | + | [[Image:Oesophageal Foreign Body.jpg|thumb|right|275px|Oesophageal Foreign Body - Copyright David Walker RVC]] |
| + | |||
===Clinical Signs=== | ===Clinical Signs=== | ||
| − | + | ||
| − | * | + | include: |
| − | * | + | *history of foreign body ingestion |
| − | * | + | *regurgitation (acute onset) |
| − | [[Image:Oesophageal Foreign Body Endoscopy.png|thumb|right|200px|Oesophageal | + | *retching |
| + | *salivation | ||
| + | *odynophagia | ||
| + | *dysphagia | ||
| + | *ptyalism | ||
| + | *anorexia | ||
| + | *tachypnoea | ||
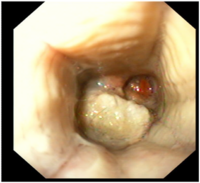
| + | [[Image:Oesophageal Foreign Body Endoscopy.png|thumb|right|200px|Oesophageal Foreign Body Endoscopy - Copyright David Walker RVC]] | ||
===Diagnostic Imaging=== | ===Diagnostic Imaging=== | ||
| − | + | Palpation of the cervical oesophagus can occasionally reveal a foreign body but a definitive diagnosis usually requires radiography. | |
| − | + | ||
| − | + | Plain thoracic radiographs reveal oesophageal foreign bodies that are radiodense. Poultry bones or other items that are less radiodense may be more difficult to visualise. | |
| − | |||
| − | + | It is important to look for signs of oesophageal perforation such as pneumothorax, pleural effusion and fluid in the mediastinum. | |
| + | |||
| + | Contrast radiography is rarely necessary but may be used to identify radiolucent foreign objects. Contrast agents must be used with caution if there is suspicion of oesophageal perforation. | ||
| + | |||
| + | Oesophagoscopy can be used to provide a definitive diagnosis of an oesophageal foreign body. | ||
| − | |||
==Treatment== | ==Treatment== | ||
| − | + | Oseophageal foreign bodies should be removed promptly to reduce the incidence of mucosal damage, ulceration and perforation. | |
| − | |||
| − | + | Endoscopic removal with grasping forceps is the method of choice for removing foreign bodies unless: | |
| + | #The object is too firmly lodged to pull free, or | ||
| + | #Radiographs suggest perforation | ||
| + | Thoracotomy is required in these cases. | ||
| − | If | + | If the object too large to be safely removed through the mouth it may be possible to push it into the stomach followed by surgical removal via a gastrotomy. |
| − | |||
| − | + | Treatment post foreign object removal may include: | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | *withdrawal of oral food for 24-48hrs | |
| + | *inspection of the oesophageal mucosa to assess for any damage. | ||
| + | *thoracic radiographs to look for pneumothorax caused by oesophageal perforation. | ||
| + | *[[Antibiotics|antibiotic therapy]]. | ||
| + | *administration of [[Gastroprotective Drugs|gastroprotective drugs]] such as H<sub>2</sub> receptor antagonists or proton pump inhibitors. | ||
| + | *[[Drugs Acting on the Intestines|prokinetic agents]]. | ||
| + | *gastrotomy feeding tube. | ||
==Prognosis== | ==Prognosis== | ||
| − | Animals with oesophageal foreign bodies without perforation carry a good prognosis. Those with oesophageal perforation carry a guarded prognosis depending on the degree of thoracic contamination. | + | Animals with oesophageal foreign bodies without perforation carry a good prognosis. Those with oesophageal perforation carry a guarded prognosis depending on the degree of thoracic contamination. |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==References== | ==References== | ||
| Line 61: | Line 81: | ||
*Hall, E.J, Simpson, J.W. and Williams, D.A. (2005) '''BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition)''' ''BSAVA'' | *Hall, E.J, Simpson, J.W. and Williams, D.A. (2005) '''BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition)''' ''BSAVA'' | ||
| − | *Merck & Co (2008) '''The Merck Veterinary Manual''' | + | *Merck & Co (2008) '''The Merck Veterinary Manual''' |
*Nelson, R.W. and Couto, C.G. (2009) '''Small Animal Internal Medicine (Fourth Edition)''' ''Mosby Elsevier''. | *Nelson, R.W. and Couto, C.G. (2009) '''Small Animal Internal Medicine (Fourth Edition)''' ''Mosby Elsevier''. | ||
| − | + | [[Category:Oesophagus_-_Pathology]][[Category:To_Do_-_Clinical]] | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | [[Category:Oesophagus_-_Pathology]] | ||
| − | [[Category: | ||
| − | |||
Revision as of 11:37, 28 June 2010
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
Typical Signalment
- Any age group can be affected
- Can occur in cats or dogs
- Dogs more commonly affected due to their less discriminating eating habits
Description
Almost anything can become lodged in the oesophagus. Objects with sharp points are very common and include:
- bones
- fish hooks
- needles
- sticks
- toys
The most common foreign bodies found in dogs are bones, bone fragments and coins. In cats play objects are most common. Many foreign objects are regurgitated or are transported through the gastrointestinal tract. Those that are too large to pass through the oesophagus remain lodged causing mechanical obstruction.
Common sites of obstruction:
- thoracic inlet
- base of the heart
- immediately in front of the diaphragm
The severity of oesophageal damage is dependent on the size, angularity or sharp pointedness of the foreign body as well as the duration of obstruction.
Diagnosis
Clinical Signs
include:
- history of foreign body ingestion
- regurgitation (acute onset)
- retching
- salivation
- odynophagia
- dysphagia
- ptyalism
- anorexia
- tachypnoea
Diagnostic Imaging
Palpation of the cervical oesophagus can occasionally reveal a foreign body but a definitive diagnosis usually requires radiography.
Plain thoracic radiographs reveal oesophageal foreign bodies that are radiodense. Poultry bones or other items that are less radiodense may be more difficult to visualise.
It is important to look for signs of oesophageal perforation such as pneumothorax, pleural effusion and fluid in the mediastinum.
Contrast radiography is rarely necessary but may be used to identify radiolucent foreign objects. Contrast agents must be used with caution if there is suspicion of oesophageal perforation.
Oesophagoscopy can be used to provide a definitive diagnosis of an oesophageal foreign body.
Treatment
Oseophageal foreign bodies should be removed promptly to reduce the incidence of mucosal damage, ulceration and perforation.
Endoscopic removal with grasping forceps is the method of choice for removing foreign bodies unless:
- The object is too firmly lodged to pull free, or
- Radiographs suggest perforation
Thoracotomy is required in these cases.
If the object too large to be safely removed through the mouth it may be possible to push it into the stomach followed by surgical removal via a gastrotomy.
Treatment post foreign object removal may include:
- withdrawal of oral food for 24-48hrs
- inspection of the oesophageal mucosa to assess for any damage.
- thoracic radiographs to look for pneumothorax caused by oesophageal perforation.
- antibiotic therapy.
- administration of gastroprotective drugs such as H2 receptor antagonists or proton pump inhibitors.
- prokinetic agents.
- gastrotomy feeding tube.
Prognosis
Animals with oesophageal foreign bodies without perforation carry a good prognosis. Those with oesophageal perforation carry a guarded prognosis depending on the degree of thoracic contamination.
References
- Hall, E.J, Simpson, J.W. and Williams, D.A. (2005) BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition) BSAVA
- Merck & Co (2008) The Merck Veterinary Manual
- Nelson, R.W. and Couto, C.G. (2009) Small Animal Internal Medicine (Fourth Edition) Mosby Elsevier.