Difference between revisions of "Equine Protozoal Myeloencephalitis"
| (85 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
| − | {{ | + | {{unfinished}} |
| − | |||
| − | |||
| − | |||
| − | ==Aetiology== | + | {| cellpadding="10" cellspacing="0" border="1" |
| − | EPM results from infection of the CNS by the apicomplexan parasite | + | | Also known as: |
| + | |'''EPM<br> | ||
| + | '''Equine protozoal myelitis<br> | ||
| + | '''Equine protozoal encephalomyelitis''' | ||
| + | |} | ||
| + | |||
| + | |||
| + | ====Description==== | ||
| + | A progressive, infectious,<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref>neurological disease of horses, endemic in the USA<ref name="EPM8">Gray, L.C, Magdesian, K.G, Sturges, B.K, Madigan, J.E (2001) Suspected protozoal myeloencephalitis in a two-month-old colt. ''Vet Rec'', 149:269-273.</ref> and only encountered elsewhere in imported equids.<ref name="EPM3">Vatistas, N, Mayhew, J (1995) Differential diagnosis of polyneuritis equi. ''In Practice'', Jan, 26-29.</ref> EPM is one of the most frequently diagnosed neurological conditions of the Western Hemisphere<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> and the principal differential for multifocal, asymmetric progressive central nervous system (CNS) disease.<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref> As it can resemble any neurological disorder, EPM must be considered in any horse with neurological signs if it resides in the Americas or if it has been imported from that area<ref name="EPM8">Gray, L.C, Magdesian, K.G, Sturges, B.K, Madigan, J.E (2001) Suspected protozoal myeloencephalitis in a two-month-old colt. ''Vet Rec'', 149:269-273.</ref><ref name="EPM9">DEFRA, The Animal Health Trust, The British Equine Veterinary Association (2009) Surveillance: Equine disease surveillance, April to June 2009, ''The Vet Rec'', Oct 24:489-492.</ref> The disease is not contagious.<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''', (Third edition), ''SUDZ Publishing'', 245-250.</ref> | ||
| + | |||
| + | ====Aetiology==== | ||
| + | EPM results from infection of the CNS by the apicomplexan parasite ''Sarcocystis neurona'' or, less frequently, its close relative ''Neospora hughesi''.<ref>Dubey, J.P, Lindsay, D.S, Saville, W.J, Reed, S.M, Granstrom, D.E, Speer, C.A (2001)A review of ''Sarcocystis neurona'' and equine protozoal myeloencephalitis (EPM). ''Vet Parasitol'', 95:89-131. In: Pusterla, N, Wilson, W.D, Conrad, P.A, Barr, B.C, Ferraro, G.L, Daft, B.M, Leutenegger, C.M (2006) Cytokine gene signatures in neural tissue of horses with equine protozoal myeloencephalitis or equine herpes type 1 myeloencephalopathy. ''Vet Rec'', Sep 9:''Papers & Articles''.</ref><ref>Wobeser, B.K, Godson, D.L, Rejmanek, D, Dowling, P (2009) Equine protozoal myeloencephalitis caused by ''Neospora hughesi'' in an adult horse in Saskatchewan. ''Can Vet J'', 50(8):851-3.</ref> These protozoans develop within neurons<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> causing immediate or inflammatory-mediated neuronal damage. The organisms migrate randomly through the brain and spinal cord causing asymmetrical lesions of grey and white matter and thus multifocal lower and upper motor neuron deficits.<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref> | ||
| + | |||
| + | ====Epidemiology==== | ||
| + | |||
| + | In endemic areas of the United States, around a quarter of referrals for equine neurological disease are attributed to EPM.<ref>Reed, S.M, Granstrom, D, Rivas, L.J, Saville, W.A, Moore, B.R, Mitten, L.A (1994) Results of cerebrospinal fluid analysis in 119 horses testing positive to the Western blot test on both serum and CSF to equine protozoal encephalomyelitis. In ''Proc Am Assoc Equine Pract'', Vancouver BC, AEEP, Lexington, KY, p199. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> According to the United States Department of Agriculture, the average incidence of the disease is 14 cases per 10,000 horses per year. However, the challenges of obtaining a definitive diagnosis may mean this figure is an underestimate.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> The disease has been identified in parts of Central and South America, southern Canada and across most of the USA..<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> EPM is noted occasionally in other countries, in horses that have been imported from the Americas.<ref>Pitel, P.H, Pronost, S, Gargala, G, Anrioud, D, Toquet, M-P, Foucher, N, Collobert-Laugier, C, Fortier, G, Ballet, J-J (2002) Detection of ''Sarcocystis neurona'' antibodies in French horses with neurological signs, ''Int J Parasitol'', 32:481-485. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref><ref>Goehring, L.S (2001) Sloet van Oldruitenborgh-Oosterbaan MM: Equine protozoal myeloencephalitis in the Netherlands? An overview, ''Tijdschr Diergeneeskd'', 126:346-351. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> It is likely that these animals underwent transportation carrying a silent but persistent infection. There have been reports of EPM in horses that have not travelled to or from endemic regions,<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> although cross-reacting antigens on the immunoblot test may explain this discrepancy. <ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | ||
| − | + | The route of infection remains unconfirmed,<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref> but there is an increased risk associated with a young age (1-4 years)<ref>Saville, W.J.A, Reed, S.M, Granstrom, D.E, Morley, P.S (1997) Some epidemiologic aspects of equine protozoal | |
| − | + | myeloencephalitis. ''Proceedings of the Annual Convention of the AAEP'', 43:6-7.</ref>and autumn months.<ref>NAHMS (2000): ''Equine protozoal myeloencephalitis in the US'', Ft Collins, CO, USDA:APHIS:VS, CEAH, National Animal Health Monitoring System. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> The reported age range for EPM cases is currently 2 months<ref name="EPM8">Gray, L.C, Magdesian, K.G, Sturges, B.K, Madigan, J.E (2001) Suspected protozoal myeloencephalitis in a two-month-old colt. ''Vet Rec'', 149:269-273.</ref> to 24 years.<ref>MacKay, R.J, Davis, S.W, Dubey, J.P (1992) Equine protozoal myeloencephalitis, ''Compend Contin Educ Pract Vet'', 14:1359-1367. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> Thoroughbreds, Standardbreds and Quarterhorses are most frequently affected across the US and Canada.<ref>Fayer, R, Mayhew, I.G, Baird, J.D, Dill, S.G, Foreman, J.H, Fox, J.C, Higgins, R.J Higgins, Reed, S.M, Ruoff, W.W, Sweeney, R.W, Tuttle, P (1990) Epidemiology of equine protozoal myeloencephalitis in North America based on histologically confirmed cases, ''J Vet Intern Med'', 4:54-57. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> This may relate to a breed predispostion or alternatively, managemental factors associated with these breeds.<ref>Boy, M.G, Galligan, D.T, Divers, T.J (1990) Protozoal encephalomyelitis in horses: 82 cases (1972-1986), ''J Am Vet Med Assoc'', 196:632-634. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> Showing, racing and stress<ref name="Saville">Saville, W.J, Reed, S.M, Morley, P.S, Granstrom, D.E, Kohn, C.W, Hinchcliff, K.W, Wittum, T.E (2000) Analysis of risk factors for the development of equine protozoal myeloencephalitis in horses. ''J Am Vet Med Assoc'', 217:1174-1180. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> have been linked to a greater risk of clinical disease.<ref>Saville, W.J.A, Reed, S.M, Morley, P.S (1999) Examination of risk factors for equine protozoal | |
| + | myeloencephalitis. ''Proceedings of the Annual Convention of the AAEP'', 45:48-49.</ref> | ||
| − | + | Increasing age and environmental temperature have been associated with an increased seroprevalence of ''S. neurona''.<ref>Tillotson, K, McCue, P.M, Granstrom, D.E, Dargatz, D.A, Smith, M.O, Traub-Dargatz, J.L (1999) Seroprevalence of antibodies to ''Sarcocystis neurona'' in horses residing in northern Colorado, ''J Equine Vet Sci'', 19:122-126. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> Seroprevalence for this species is typically higher than for ''N. hughesi''.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref>Other risk factors for EPM include the presence of opossums, rats, mice and woodland, increased population density of humans and horses, bedding horses on shavings or wood chips and the use of purchased grain.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref>Case clustering may operate where all the risk factors occur, but the majority of cases appear in isolation.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | |
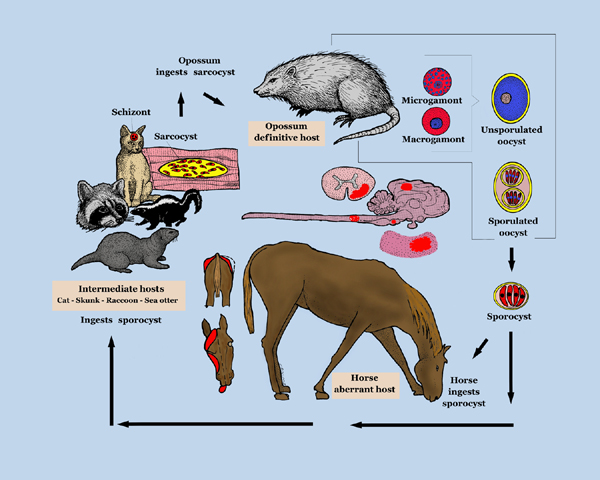
| − | ==Life Cycle== | + | ====Life Cycle==== |
[[Image:Equine_Protozoal_Myeloencephalitis_life_cycle.jpg|600px|thumb|centre|''' Life cycle diagram of ''Sarcocystis neurona''. Created by the ''Agricultural Research Service, the research agency of the United States Department of Agriculture'', July 2005. ''Sourced from the USDA Agricultural Research Service page on EPM/Sarcocystis neurona, located via WikiMedia Commons.'' ''']] | [[Image:Equine_Protozoal_Myeloencephalitis_life_cycle.jpg|600px|thumb|centre|''' Life cycle diagram of ''Sarcocystis neurona''. Created by the ''Agricultural Research Service, the research agency of the United States Department of Agriculture'', July 2005. ''Sourced from the USDA Agricultural Research Service page on EPM/Sarcocystis neurona, located via WikiMedia Commons.'' ''']] | ||
| − | + | The causative pathogen(s) have been isolated form species other than the horse including zebra, domestic cat, Canadian lynx, sea otter, straw-necked ibis, mink, raccoon and sunk. (Furr) | |
| − | == | + | ====Signalment==== |
| + | Mostly Standardbreds and Thoroughbreds aged 1-6years.<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref> Foal infection may be possible.<ref name="EPM8">Gray, L.C, Magdesian, K.G, Sturges, B.K, Madigan, J.E (2001) Suspected protozoal myeloencephalitis in a two-month-old colt. ''Vet Rec'', 149:269-273.</ref> | ||
| − | + | ====History==== | |
| + | Typically an insidious onset ataxia, but the presentation may be acute and severe. | ||
| − | The | + | ====Clinical Signs==== |
| + | The disease onset may be acute, peracute of chronic. The insidious onset is most typical and with such cases, the clinical examination may reveal a bright, alert horse bright perhaps with some focal muscle atrophy.(Furr)In all cases, the clinical signs are referable to diffuse focal and multifocal lesions of the white and grey matter of the spinal cord and brain (EPM3) | ||
| − | + | Spinal cord: | |
| − | + | *Ataxia and paresis | |
| + | |||
| + | Ataxia or paresis of one or more limbs: stumbling, falling, knuckling and toe dragging. | ||
| + | Sacrococcygeal involvement: mimics polyneuritis equi. | ||
| + | Cranial nerve signs: loss of tongue tone, loss of sensation to the face and unilateral facial paralysis. Brain involvement: dysphagia, circling, head tilt or recumbency(EPM3) | ||
| + | |||
| + | Signs: asymmetrical weakness, ataxia, vestibular disease (peripheral or central) peripheral neuropathy, ill-defined hindlimb lameness, asymmetric muscle atrophy. (Vetstream) | ||
| − | |||
| − | |||
| − | + | Spinal cord infection : | |
| − | + | *Ataxia and weakness (hindlimbs > forelimbs) - often asymmetrical. | |
| − | + | *Apparent lameness, particularly atypical or slight gait asymmetry of hindlimbs (not alleviated by local anesthesia). | |
| − | + | *Abnormal placing reactions. | |
| − | + | *Focal muscle atrophy (individual muscle grps (Pasq)- evident anywhere especially gluteal muscles - often asymmetrical. | |
| − | + | *Generalized muscle atrophy/loss of condition | |
| − | *Ataxia | + | Lesions of the brainstem, cerebrum or cerebellum are less frequently recognized: |
| − | + | Cranial nerve dysfunction (<5% of cases) - any can be affected: | |
| − | *Apparent lameness, particularly atypical or slight gait asymmetry of hindlimbs (not alleviated by local | + | *Atrophy of temporalis/masseter muscles (V) |
| − | *Abnormal placing reactions | + | *Dysphagia (V, VII, IX, X, XII) |
| − | *Focal muscle atrophy | + | *Abnormalities of facial (VII) and vestibulocochlear (VIII) nerves often observed together: |
| − | *Generalized muscle atrophy | + | *VIII - vestibular signs of nystagmus, head tilt, base-wide stance |
| − | + | *VII - muzzle deviation, ptosis, ear droop | |
| − | + | *Dorsal displacement of soft palate (IX, X) | |
| − | + | *Laryngeal hemiplegia (X) | |
| − | + | Severe cases may: | |
| − | + | *Inability to stand. | |
| − | + | *Inability to swallow. | |
| − | + | Infection of cerebrum, basal nuclei, cerebellum: | |
| − | + | Focal cerebral problems: | |
| − | + | *Seizures (may be the only clinical sign)(82 in Furr) | |
| − | + | *Abnormal EEG. | |
| − | |||
| − | |||
| − | *Atrophy of | ||
| − | * | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | *Dorsal displacement of | ||
| − | *Laryngeal hemiplegia (X) | ||
| − | |||
| − | * | ||
| − | |||
| − | * | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | *Seizures (may be the only clinical sign) | ||
| − | *Abnormal | ||
*Asymmetrical central blindness | *Asymmetrical central blindness | ||
| − | *Facial | + | *Facial hypalgesia |
*Cerebellar ataxia | *Cerebellar ataxia | ||
*Altered behavior | *Altered behavior | ||
*Depression | *Depression | ||
| − | *Narcolepsy-like syndrome | + | *Narcolepsy-like syndrome |
| − | + | Nerve damage/ataxia injuries to muscle tendons or ligaments: | |
| + | *Upward fixation of the patella | ||
| + | *Exertional rhabdomyolysis . | ||
| + | *Back pain. | ||
| + | *Gait abnormality. | ||
| + | Any gait abnormality in galloping/trotting race/dressage horses while in training which cannot be attributed to musculoskeletal abnormality may result from EPM and requires careful neurologic evaluation.(Vetstream) | ||
| − | + | Headshaking(EPM 7) | |
| − | + | Gait abnormality (peracute or acute) - 1 or all 4 limbs depending on where migrates, asymmetrical (because multifocal), ataxia, paresis & spasticity - knuckling, circumduction, crossing over, tetraparesis - areflexia, hyporeflexia (LMN) or hyperreflexia (UMN) depending on site of lesion, localized areas of sensory deficits, 'strip sweating' localized areas (dermatomes, sympathetic white matter tracts), cerebellar, brain stem (less common) or cerebral signs, cranial nn - head tilt, facial paralysis, circling, nystagmus, dysphagia, blindness with or without abnormal pupillary reflexes, untreated progressive to recumbency in 14days to 6mths (Pasq) | |
| − | + | The three characteristic 'As' of EPM (ataxia, asymmetry, atrophy) suggest multifocal or diffuse disease, but are not pathognomonic. It has been suggested that rapidly progressive presentations reflect brainstem lesions. Spinal cord signs are most commonly seen and may include: | |
| − | * | + | *asymmetric or symmetric paresis, spasticity and ataxia of one to four limbs |
| − | * | + | *focal or general muscle atrophy |
| − | * | + | *apparent lameness |
| − | * | + | *back pain |
| − | + | *loss of reflexes or cutaneous anaesthesia | |
| + | *abnormal menace response | ||
| + | Without treatment, progression to recumbency and death is likely. This deterioration may occur smoothly or spasmodically over hours to years. (Merck) | ||
| − | === | + | ====Diagnosis==== |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | === | + | ====Differential Diagnoses==== |
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | The protozoan can migrate to any region of the CNS<ref name="EPM8">Gray, L.C, Magdesian, K.G, Sturges, B.K, Madigan, J.E (2001) Suspected protozoal myeloencephalitis in a two-month-old colt. ''Vet Rec'', 149:269-273.</ref>, thus the differential list comprises almost all diseases of this system. | |
| − | |||
| − | |||
{| cellpadding="10" cellspacing="0" border="1" | {| cellpadding="10" cellspacing="0" border="1" | ||
| Line 116: | Line 111: | ||
|- | |- | ||
|Cervical vertebral malformation (CVM, cervical compressive myelopathy, cervical vertebral instability, cervical stenotic myelopathy, cervical spondylomyelopathy, Wobbler's syndrome). | |Cervical vertebral malformation (CVM, cervical compressive myelopathy, cervical vertebral instability, cervical stenotic myelopathy, cervical spondylomyelopathy, Wobbler's syndrome). | ||
| − | |Symmetrical gait deficits, worse in pelvic limbs<ref>Mayhew, I.G, deLahunta, A, Whitlock, R.H, Krook, L, Tasker, J.B (1978) Spinal cord disease in the horse, ''Cornell Vet'', 68(Suppl 8):110-120. In: Hahn, C.N (2010) ''Cervical Vertebral Malformation'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> with spasticity and dysmetria, good retention of strength, no muscle wasting.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> '''NB: can be concurrent with EPM'''.<ref name="Hahn">Hahn, C.N (2010) ''Cervical Vertebral Malformation'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | + | |Symmetrical gait deficits, worse in pelvic limbs<ref>Mayhew, I.G, deLahunta, A, Whitlock, R.H, Krook, L, Tasker, J.B (1978) Spinal cord disease in the horse, ''Cornell Vet'', 68(Suppl 8):110-120. In: Hahn, C.N (2010) ''Cervical Vertebral Malformation'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> with spasticity and dysmetria, good retention of strength, no muscle wasting.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> '''NB:can be concurrent with EPM'''.<ref name="Hahn">Hahn, C.N (2010) ''Cervical Vertebral Malformation'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> |
|Plain lateral radiography of C1 to T1<ref name="Hahn">Hahn, C.N (2010) ''Cervical Vertebral Malformation'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref>, myelography. <ref name="Seino">Seino, K.K (2010) ''Spinal Ataxia'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 3.</ref> | |Plain lateral radiography of C1 to T1<ref name="Hahn">Hahn, C.N (2010) ''Cervical Vertebral Malformation'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref>, myelography. <ref name="Seino">Seino, K.K (2010) ''Spinal Ataxia'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 3.</ref> | ||
|- | |- | ||
| − | + | |West Nile encephalitis | |
|Systemically ill, pyrexia. Difficult to differentiate if horse is afebrile and has no excessive muscle fasciculations.<ref name="Long">Long, M.T (2010) ''Flavivirus Encephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | |Systemically ill, pyrexia. Difficult to differentiate if horse is afebrile and has no excessive muscle fasciculations.<ref name="Long">Long, M.T (2010) ''Flavivirus Encephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | ||
| − | |Leukogram, CSF analysis, IgM capture ELISA, plaque reduction neutralization test (PRNT) | + | |Leukogram, CSF analysis, IgM capture ELISA, plaque reduction neutralization test (PRNT).<ref name="Seino">Seino, K.K (2010) ''Spinal Ataxia'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 3.</ref> |
|- | |- | ||
|[[Equine Togaviral Encephalitis|WEE]] | |[[Equine Togaviral Encephalitis|WEE]] | ||
| Line 135: | Line 130: | ||
|Leukogram, IgM ELISA<ref>Bertone, J.J (2010) ''Viral Encephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | |Leukogram, IgM ELISA<ref>Bertone, J.J (2010) ''Viral Encephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | ||
|- | |- | ||
| − | + | |Equine herpesvirus-1 myeloencephalopathy | |
| − | |Sudden onset and early stabilization of neurological signs, multiple horses affected, recent fever | + | |Sudden onset and early stabilization of neurological signs, multiple horses affected, recent fever, abortion.<ref>Wilson, W.D, Pusterla, N (2010) ''Equine Herpesvirus-1 Myeloencephalopathy'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> Dysuria not often seen in EPM.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> |
| − | |CSF analysis, | + | |CSF analysis, PCR<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref>, titres, virus isolation.<ref name="Seino">Seino, K.K (2010) ''Spinal Ataxia'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 3.</ref> |
|- | |- | ||
| − | | | + | |Rabies |
|Rapid progression<ref name="Sommardahl">Sommardahl, C.S (2010) ''Rabies'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref>, behavioural alterations, depression, seizure, coma.<ref name="Long">Long, M.T (2010) ''Flavivirus Encephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | |Rapid progression<ref name="Sommardahl">Sommardahl, C.S (2010) ''Rabies'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref>, behavioural alterations, depression, seizure, coma.<ref name="Long">Long, M.T (2010) ''Flavivirus Encephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | ||
|Post-mortem fluorescent antibody testing of brain required for definitive diagnosis.<ref name="Sommardahl">Sommardahl, C.S (2010) ''Rabies'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | |Post-mortem fluorescent antibody testing of brain required for definitive diagnosis.<ref name="Sommardahl">Sommardahl, C.S (2010) ''Rabies'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | ||
| Line 157: | Line 152: | ||
|Bacterial meningoencephalitis | |Bacterial meningoencephalitis | ||
|Stiff neck.<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref> | |Stiff neck.<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref> | ||
| − | | | + | | |
|- | |- | ||
| − | |CNS abscessation due to | + | |CNS abscessation due to 'bastard strangles'<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> |
| − | |History of | + | |History of ''Streptococcus equi subsp. equi'' infection.<ref name="Byrne">Byrne, B. A (2010) ''Diseases of the Cerebellum'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> |
|CSF analysis (severe, suppurative inflammation), culture of CSF.<ref name="Byrne">Byrne, B. A (2010) ''Diseases of the Cerebellum'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | |CSF analysis (severe, suppurative inflammation), culture of CSF.<ref name="Byrne">Byrne, B. A (2010) ''Diseases of the Cerebellum'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | ||
|- | |- | ||
| Line 176: | Line 171: | ||
|- | |- | ||
|''Sorghum'' cystitis/ataxia<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref> | |''Sorghum'' cystitis/ataxia<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref> | ||
| − | |Posterior ataxia or paresis, cystitis, history of grazing ''Sorghum'' species<ref | + | |Posterior ataxia or paresis, cystitis, history of grazing ''Sorghum'' species<ref>Talcott, P (2010) ''Toxicoses causing signs relating to the urinary system'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 22.</ref> |
| − | |Demonstration of cystitis or pyelonephritis by laboratory methods, but not specific.<ref | + | |Demonstration of cystitis or pyelonephritis by laboratory methods, but not specific.<ref>Talcott, P (2010) ''Toxicoses causing signs relating to the urinary system'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 22.</ref> |
|} | |} | ||
| − | + | [[Image:Equine_Protozoal_Myeloencephalitis.jpg|600px|thumb|left|''' Sarcocystis neurona stages and lesions. | |
| − | |||
| − | [[Image:Equine_Protozoal_Myeloencephalitis.jpg|600px|thumb| | ||
(A). Cross section of spinal cord of horse with focal areas of discoloration (arrows) indicative of necrosis. Unstained. | (A). Cross section of spinal cord of horse with focal areas of discoloration (arrows) indicative of necrosis. Unstained. | ||
| Line 200: | Line 193: | ||
(H). An oocyst with two sporocysts each with banana-shaped sporozoites. Unstained. | (H). An oocyst with two sporocysts each with banana-shaped sporozoites. Unstained. | ||
Created by the ''Agricultural Research Service, the research agency of the United States Department of Agriculture'', July 2005. ''Sourced from the USDA Agricultural Research Service page on EPM/Sarcocystis neurona, located via WikiMedia Commons.'' ''']] | Created by the ''Agricultural Research Service, the research agency of the United States Department of Agriculture'', July 2005. ''Sourced from the USDA Agricultural Research Service page on EPM/Sarcocystis neurona, located via WikiMedia Commons.'' ''']] | ||
| − | + | ====Pathology==== | |
| − | ===Pathology=== | ||
Widespread lesions of the CNS are typically observed in horses.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | Widespread lesions of the CNS are typically observed in horses.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | ||
| − | ====Gross exam==== | + | =====Gross exam===== |
Lesions may be up to several centimetres across.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> They range from mild discolouration to multifocal areas of haemorrhage and/or malacia<ref name="Merck">Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial</ref> of the brain, spinal cord and less commonly, peripheral nerves.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | Lesions may be up to several centimetres across.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> They range from mild discolouration to multifocal areas of haemorrhage and/or malacia<ref name="Merck">Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial</ref> of the brain, spinal cord and less commonly, peripheral nerves.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | ||
| − | ====Histopathology==== | + | =====Histopathology===== |
Microscopically, both grey and white matter may be affected with focal to diffuse areas of nonsuppurative inflammation, necrosis and neuronal destruction. Perivascular infiltrates comprise lymphocytes, macrophages, plasma cells, giant cells, eosinophils and gitter cells.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> In around 25% of cases, schizonts or merozoites may be found in the neuronal cytoplasm.<ref name="Merck">Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial</ref> Less frequently, protozoa parasitize intravascular and tissue neutrophils and eosinophils, capillary endothelial cells and myelinated axons<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref><ref name="Merck">Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial</ref>. Free merozoites may be seen in necrotic regions. If organisms are absent, the diagnosis relies on recognition of the inflammatory changes described above.<ref name="Merck">Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial</ref> | Microscopically, both grey and white matter may be affected with focal to diffuse areas of nonsuppurative inflammation, necrosis and neuronal destruction. Perivascular infiltrates comprise lymphocytes, macrophages, plasma cells, giant cells, eosinophils and gitter cells.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> In around 25% of cases, schizonts or merozoites may be found in the neuronal cytoplasm.<ref name="Merck">Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial</ref> Less frequently, protozoa parasitize intravascular and tissue neutrophils and eosinophils, capillary endothelial cells and myelinated axons<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref><ref name="Merck">Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial</ref>. Free merozoites may be seen in necrotic regions. If organisms are absent, the diagnosis relies on recognition of the inflammatory changes described above.<ref name="Merck">Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial</ref> | ||
| − | == | + | ====Treatment==== |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | === | + | ====Prognosis==== |
| − | + | Depends on duration and severity of neurological signs<ref name="EPM3">Vatistas, N, Mayhew, J (1995) Differential diagnosis of polyneuritis equi. ''In Practice'', Jan, 26-29.</ref> but clinical resolution is more likely if the condition is diagnosed and treated early.<ref name="EPM8">Gray, L.C, Magdesian, K.G, Sturges, B.K, Madigan, J.E (2001) Suspected protozoal myeloencephalitis in a two-month-old colt. ''Vet Record'', 149:269-273.</ref> With standard therapy, involving 6-8months of ponazuzril or pyrimethamine-sulfadiazine (V), there is a recovery rate of around 25% and an improvement in 60-75% of cases.<ref>MacKay, R.J (2006) Equine protozoa myeloencephalitis: treatment, prognosis and prevention. ''Clin Tech Equine Pract'', 5:9-16. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> A good prognosis might be expected if there is an improvement in clinical signs within two weeks of commencing anti-protozoal and anti-inflammatory treatment (V). The prognosis will be guarded to poor<ref name="Pasq">Pasquini, C, Pasquini, S, Woods, P (2005) '''Guide to Equine Clinics Volume 1: Equine Medicine''' (Third edition), ''SUDZ Publishing'', 245-250.</ref> for a horse with severe irreversible neuronal damage or one that has not been diagnosed or treated appropriately (V). | |
| − | + | ====Prevention==== | |
| − | + | =====Prophylaxis===== | |
| − | + | A killed vaccine, developed using ''S.neurona'' merozoites, was conditionally licensed for use in horses.<ref>Saville, W.J.A, Reed, S.M, Dubey, J.P (2002) Prevention of equine protozoal myeloencephalitis | |
| − | + | (EPM). ''Proceedings of the Annual Convention of the AAEP'', 48:181-185.</ref> The vaccine proved to be ineffective in the prevention of EPM and has since been removed from the market.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> There is evidence to suggest that the antiprotozoal, ponazuril, may be useful prophylactically to reduce the incidence and severity of clinical signs.<ref>Furr, M, MacKenzie, H, Dubey, J.P (2006) Pretreatment of horses with ponazuril limits infection and neurologic signs resulting from S.neurona. ''J Parasitol'', 92:637-643. In: Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> Implementing such a regime prior to and during stressful events may be beneficial, although the cost is likely to be prohibitive.<ref name="Furr">Furr, M (2010) ''Equine protozoal myeloencephalitis'' in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) '''Equine Internal Medicine''' (Third Edition), ''Saunders'', Chapter 12.</ref> | |
| − | |||
| − | + | ====References==== | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | == | ||
<references/> | <references/> | ||
| − | |||
| − | |||
| − | |||
| − | [[Category: | + | [[Category:Tissue_Cyst_Forming_Coccidia]][[Category:Horse]] |
| − | [[Category: | + | [[Category:To_Do_-_Nina]] |
Revision as of 19:12, 19 July 2010
| This article is still under construction. |
| Also known as: | EPM Equine protozoal myelitis |
Description
A progressive, infectious,[1]neurological disease of horses, endemic in the USA[2] and only encountered elsewhere in imported equids.[3] EPM is one of the most frequently diagnosed neurological conditions of the Western Hemisphere[4] and the principal differential for multifocal, asymmetric progressive central nervous system (CNS) disease.[1] As it can resemble any neurological disorder, EPM must be considered in any horse with neurological signs if it resides in the Americas or if it has been imported from that area[2][5] The disease is not contagious.[1]
Aetiology
EPM results from infection of the CNS by the apicomplexan parasite Sarcocystis neurona or, less frequently, its close relative Neospora hughesi.[6][7] These protozoans develop within neurons[4] causing immediate or inflammatory-mediated neuronal damage. The organisms migrate randomly through the brain and spinal cord causing asymmetrical lesions of grey and white matter and thus multifocal lower and upper motor neuron deficits.[1]
Epidemiology
In endemic areas of the United States, around a quarter of referrals for equine neurological disease are attributed to EPM.[8] According to the United States Department of Agriculture, the average incidence of the disease is 14 cases per 10,000 horses per year. However, the challenges of obtaining a definitive diagnosis may mean this figure is an underestimate.[4] The disease has been identified in parts of Central and South America, southern Canada and across most of the USA..[4] EPM is noted occasionally in other countries, in horses that have been imported from the Americas.[9][10] It is likely that these animals underwent transportation carrying a silent but persistent infection. There have been reports of EPM in horses that have not travelled to or from endemic regions,[4] although cross-reacting antigens on the immunoblot test may explain this discrepancy. [4]
The route of infection remains unconfirmed,[1] but there is an increased risk associated with a young age (1-4 years)[11]and autumn months.[12] The reported age range for EPM cases is currently 2 months[2] to 24 years.[13] Thoroughbreds, Standardbreds and Quarterhorses are most frequently affected across the US and Canada.[14] This may relate to a breed predispostion or alternatively, managemental factors associated with these breeds.[15] Showing, racing and stress[16] have been linked to a greater risk of clinical disease.[17]
Increasing age and environmental temperature have been associated with an increased seroprevalence of S. neurona.[18] Seroprevalence for this species is typically higher than for N. hughesi.[4]Other risk factors for EPM include the presence of opossums, rats, mice and woodland, increased population density of humans and horses, bedding horses on shavings or wood chips and the use of purchased grain.[4]Case clustering may operate where all the risk factors occur, but the majority of cases appear in isolation.[4]
Life Cycle
The causative pathogen(s) have been isolated form species other than the horse including zebra, domestic cat, Canadian lynx, sea otter, straw-necked ibis, mink, raccoon and sunk. (Furr)
Signalment
Mostly Standardbreds and Thoroughbreds aged 1-6years.[1] Foal infection may be possible.[2]
History
Typically an insidious onset ataxia, but the presentation may be acute and severe.
Clinical Signs
The disease onset may be acute, peracute of chronic. The insidious onset is most typical and with such cases, the clinical examination may reveal a bright, alert horse bright perhaps with some focal muscle atrophy.(Furr)In all cases, the clinical signs are referable to diffuse focal and multifocal lesions of the white and grey matter of the spinal cord and brain (EPM3)
Spinal cord:
- Ataxia and paresis
Ataxia or paresis of one or more limbs: stumbling, falling, knuckling and toe dragging. Sacrococcygeal involvement: mimics polyneuritis equi. Cranial nerve signs: loss of tongue tone, loss of sensation to the face and unilateral facial paralysis. Brain involvement: dysphagia, circling, head tilt or recumbency(EPM3)
Signs: asymmetrical weakness, ataxia, vestibular disease (peripheral or central) peripheral neuropathy, ill-defined hindlimb lameness, asymmetric muscle atrophy. (Vetstream)
Spinal cord infection :
- Ataxia and weakness (hindlimbs > forelimbs) - often asymmetrical.
- Apparent lameness, particularly atypical or slight gait asymmetry of hindlimbs (not alleviated by local anesthesia).
- Abnormal placing reactions.
- Focal muscle atrophy (individual muscle grps (Pasq)- evident anywhere especially gluteal muscles - often asymmetrical.
- Generalized muscle atrophy/loss of condition
Lesions of the brainstem, cerebrum or cerebellum are less frequently recognized: Cranial nerve dysfunction (<5% of cases) - any can be affected:
- Atrophy of temporalis/masseter muscles (V)
- Dysphagia (V, VII, IX, X, XII)
- Abnormalities of facial (VII) and vestibulocochlear (VIII) nerves often observed together:
- VIII - vestibular signs of nystagmus, head tilt, base-wide stance
- VII - muzzle deviation, ptosis, ear droop
- Dorsal displacement of soft palate (IX, X)
- Laryngeal hemiplegia (X)
Severe cases may:
- Inability to stand.
- Inability to swallow.
Infection of cerebrum, basal nuclei, cerebellum: Focal cerebral problems:
- Seizures (may be the only clinical sign)(82 in Furr)
- Abnormal EEG.
- Asymmetrical central blindness
- Facial hypalgesia
- Cerebellar ataxia
- Altered behavior
- Depression
- Narcolepsy-like syndrome
Nerve damage/ataxia injuries to muscle tendons or ligaments:
- Upward fixation of the patella
- Exertional rhabdomyolysis .
- Back pain.
- Gait abnormality.
Any gait abnormality in galloping/trotting race/dressage horses while in training which cannot be attributed to musculoskeletal abnormality may result from EPM and requires careful neurologic evaluation.(Vetstream)
Headshaking(EPM 7)
Gait abnormality (peracute or acute) - 1 or all 4 limbs depending on where migrates, asymmetrical (because multifocal), ataxia, paresis & spasticity - knuckling, circumduction, crossing over, tetraparesis - areflexia, hyporeflexia (LMN) or hyperreflexia (UMN) depending on site of lesion, localized areas of sensory deficits, 'strip sweating' localized areas (dermatomes, sympathetic white matter tracts), cerebellar, brain stem (less common) or cerebral signs, cranial nn - head tilt, facial paralysis, circling, nystagmus, dysphagia, blindness with or without abnormal pupillary reflexes, untreated progressive to recumbency in 14days to 6mths (Pasq)
The three characteristic 'As' of EPM (ataxia, asymmetry, atrophy) suggest multifocal or diffuse disease, but are not pathognomonic. It has been suggested that rapidly progressive presentations reflect brainstem lesions. Spinal cord signs are most commonly seen and may include:
- asymmetric or symmetric paresis, spasticity and ataxia of one to four limbs
- focal or general muscle atrophy
- apparent lameness
- back pain
- loss of reflexes or cutaneous anaesthesia
- abnormal menace response
Without treatment, progression to recumbency and death is likely. This deterioration may occur smoothly or spasmodically over hours to years. (Merck)
Diagnosis
Differential Diagnoses
The protozoan can migrate to any region of the CNS[2], thus the differential list comprises almost all diseases of this system.
| Differential | Differentiating signs | Tests to rule out |
| Cervical vertebral malformation (CVM, cervical compressive myelopathy, cervical vertebral instability, cervical stenotic myelopathy, cervical spondylomyelopathy, Wobbler's syndrome). | Symmetrical gait deficits, worse in pelvic limbs[19] with spasticity and dysmetria, good retention of strength, no muscle wasting.[4] NB:can be concurrent with EPM.[20] | Plain lateral radiography of C1 to T1[20], myelography. [21] |
| West Nile encephalitis | Systemically ill, pyrexia. Difficult to differentiate if horse is afebrile and has no excessive muscle fasciculations.[22] | Leukogram, CSF analysis, IgM capture ELISA, plaque reduction neutralization test (PRNT).[21] |
| WEE | Systemically ill, pyrexia, abnormal motor function.[22] | Leukogram, ELISA, titres, virus isolation.[21] |
| EEE | Systemically ill, pyrexia, abnormal motor function[22], rapidly progressive.[21] | Leukogram, CSF analysis, ELISA, titres, virus isolation.[21] |
| VEE | Systemically ill, pyrexia. | Leukogram, IgM ELISA[23] |
| Equine herpesvirus-1 myeloencephalopathy | Sudden onset and early stabilization of neurological signs, multiple horses affected, recent fever, abortion.[24] Dysuria not often seen in EPM.[4] | CSF analysis, PCR[4], titres, virus isolation.[21] |
| Rabies | Rapid progression[25], behavioural alterations, depression, seizure, coma.[22] | Post-mortem fluorescent antibody testing of brain required for definitive diagnosis.[25] |
| Polyneuritis equi (previously cauda equina neuritis) | Cranial nerve deficits are peripheral with no change in attitude.[26] | Western blot analysis of CSF.[27] |
| Equine degenerative myeloencephalopathy | Symmetrical signs.[28] | May get increased CSF creatinine kinase (CK)[29] and reduced serum Vitamin E concentrations but these are unreliable for ante mortem diagnosis.[28] |
| Verminous encephalomyelitis | Acute onset. | CSF analysis.[30] |
| Bacterial meningoencephalitis | Stiff neck.[1] | |
| CNS abscessation due to 'bastard strangles'[4] | History of Streptococcus equi subsp. equi infection.[31] | CSF analysis (severe, suppurative inflammation), culture of CSF.[31] |
| Spinal trauma[1] | History (usually acute onset neurological signs), usually solitary lesion localised by neurological exam.[32] | Radiography, myelography, CT, MRI, nuclear scintigraphy, ultrasound, CSF analysis, nerve conduction velocities, EMG, transcranial magnetic stimulation.[33] |
| Occipito-atlanto-axial malformation (OAAM) | Deficits develop before 6mths in Arabian horse.[34] | Radiography.[21] |
| Spinal tumor | Signs can usually be localized to one region of the CNS. | CT, MRI. Definitive diagnosis requires cytology, biopsy, histopathology or CSF analysis.[35] |
| Sorghum cystitis/ataxia[1] | Posterior ataxia or paresis, cystitis, history of grazing Sorghum species[36] | Demonstration of cystitis or pyelonephritis by laboratory methods, but not specific.[37] |
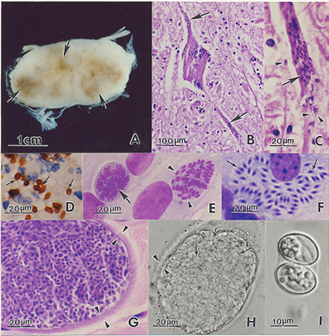
Pathology
Widespread lesions of the CNS are typically observed in horses.[4]
Gross exam
Lesions may be up to several centimetres across.[4] They range from mild discolouration to multifocal areas of haemorrhage and/or malacia[38] of the brain, spinal cord and less commonly, peripheral nerves.[4]
Histopathology
Microscopically, both grey and white matter may be affected with focal to diffuse areas of nonsuppurative inflammation, necrosis and neuronal destruction. Perivascular infiltrates comprise lymphocytes, macrophages, plasma cells, giant cells, eosinophils and gitter cells.[4] In around 25% of cases, schizonts or merozoites may be found in the neuronal cytoplasm.[38] Less frequently, protozoa parasitize intravascular and tissue neutrophils and eosinophils, capillary endothelial cells and myelinated axons[4][38]. Free merozoites may be seen in necrotic regions. If organisms are absent, the diagnosis relies on recognition of the inflammatory changes described above.[38]
Treatment
Prognosis
Depends on duration and severity of neurological signs[3] but clinical resolution is more likely if the condition is diagnosed and treated early.[2] With standard therapy, involving 6-8months of ponazuzril or pyrimethamine-sulfadiazine (V), there is a recovery rate of around 25% and an improvement in 60-75% of cases.[39] A good prognosis might be expected if there is an improvement in clinical signs within two weeks of commencing anti-protozoal and anti-inflammatory treatment (V). The prognosis will be guarded to poor[1] for a horse with severe irreversible neuronal damage or one that has not been diagnosed or treated appropriately (V).
Prevention
Prophylaxis
A killed vaccine, developed using S.neurona merozoites, was conditionally licensed for use in horses.[40] The vaccine proved to be ineffective in the prevention of EPM and has since been removed from the market.[4] There is evidence to suggest that the antiprotozoal, ponazuril, may be useful prophylactically to reduce the incidence and severity of clinical signs.[41] Implementing such a regime prior to and during stressful events may be beneficial, although the cost is likely to be prohibitive.[4]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Pasquini, C, Pasquini, S, Woods, P (2005) Guide to Equine Clinics Volume 1: Equine Medicine (Third edition), SUDZ Publishing, 245-250. Cite error: Invalid
<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content Cite error: Invalid<ref>tag; name "Pasq" defined multiple times with different content - ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Gray, L.C, Magdesian, K.G, Sturges, B.K, Madigan, J.E (2001) Suspected protozoal myeloencephalitis in a two-month-old colt. Vet Rec, 149:269-273. Cite error: Invalid
<ref>tag; name "EPM8" defined multiple times with different content - ↑ 3.0 3.1 Vatistas, N, Mayhew, J (1995) Differential diagnosis of polyneuritis equi. In Practice, Jan, 26-29.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ DEFRA, The Animal Health Trust, The British Equine Veterinary Association (2009) Surveillance: Equine disease surveillance, April to June 2009, The Vet Rec, Oct 24:489-492.
- ↑ Dubey, J.P, Lindsay, D.S, Saville, W.J, Reed, S.M, Granstrom, D.E, Speer, C.A (2001)A review of Sarcocystis neurona and equine protozoal myeloencephalitis (EPM). Vet Parasitol, 95:89-131. In: Pusterla, N, Wilson, W.D, Conrad, P.A, Barr, B.C, Ferraro, G.L, Daft, B.M, Leutenegger, C.M (2006) Cytokine gene signatures in neural tissue of horses with equine protozoal myeloencephalitis or equine herpes type 1 myeloencephalopathy. Vet Rec, Sep 9:Papers & Articles.
- ↑ Wobeser, B.K, Godson, D.L, Rejmanek, D, Dowling, P (2009) Equine protozoal myeloencephalitis caused by Neospora hughesi in an adult horse in Saskatchewan. Can Vet J, 50(8):851-3.
- ↑ Reed, S.M, Granstrom, D, Rivas, L.J, Saville, W.A, Moore, B.R, Mitten, L.A (1994) Results of cerebrospinal fluid analysis in 119 horses testing positive to the Western blot test on both serum and CSF to equine protozoal encephalomyelitis. In Proc Am Assoc Equine Pract, Vancouver BC, AEEP, Lexington, KY, p199. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Pitel, P.H, Pronost, S, Gargala, G, Anrioud, D, Toquet, M-P, Foucher, N, Collobert-Laugier, C, Fortier, G, Ballet, J-J (2002) Detection of Sarcocystis neurona antibodies in French horses with neurological signs, Int J Parasitol, 32:481-485. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Goehring, L.S (2001) Sloet van Oldruitenborgh-Oosterbaan MM: Equine protozoal myeloencephalitis in the Netherlands? An overview, Tijdschr Diergeneeskd, 126:346-351. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Saville, W.J.A, Reed, S.M, Granstrom, D.E, Morley, P.S (1997) Some epidemiologic aspects of equine protozoal myeloencephalitis. Proceedings of the Annual Convention of the AAEP, 43:6-7.
- ↑ NAHMS (2000): Equine protozoal myeloencephalitis in the US, Ft Collins, CO, USDA:APHIS:VS, CEAH, National Animal Health Monitoring System. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ MacKay, R.J, Davis, S.W, Dubey, J.P (1992) Equine protozoal myeloencephalitis, Compend Contin Educ Pract Vet, 14:1359-1367. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Fayer, R, Mayhew, I.G, Baird, J.D, Dill, S.G, Foreman, J.H, Fox, J.C, Higgins, R.J Higgins, Reed, S.M, Ruoff, W.W, Sweeney, R.W, Tuttle, P (1990) Epidemiology of equine protozoal myeloencephalitis in North America based on histologically confirmed cases, J Vet Intern Med, 4:54-57. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Boy, M.G, Galligan, D.T, Divers, T.J (1990) Protozoal encephalomyelitis in horses: 82 cases (1972-1986), J Am Vet Med Assoc, 196:632-634. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Saville, W.J, Reed, S.M, Morley, P.S, Granstrom, D.E, Kohn, C.W, Hinchcliff, K.W, Wittum, T.E (2000) Analysis of risk factors for the development of equine protozoal myeloencephalitis in horses. J Am Vet Med Assoc, 217:1174-1180. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Saville, W.J.A, Reed, S.M, Morley, P.S (1999) Examination of risk factors for equine protozoal myeloencephalitis. Proceedings of the Annual Convention of the AAEP, 45:48-49.
- ↑ Tillotson, K, McCue, P.M, Granstrom, D.E, Dargatz, D.A, Smith, M.O, Traub-Dargatz, J.L (1999) Seroprevalence of antibodies to Sarcocystis neurona in horses residing in northern Colorado, J Equine Vet Sci, 19:122-126. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Mayhew, I.G, deLahunta, A, Whitlock, R.H, Krook, L, Tasker, J.B (1978) Spinal cord disease in the horse, Cornell Vet, 68(Suppl 8):110-120. In: Hahn, C.N (2010) Cervical Vertebral Malformation in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 20.0 20.1 Hahn, C.N (2010) Cervical Vertebral Malformation in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 Seino, K.K (2010) Spinal Ataxia in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 3.
- ↑ 22.0 22.1 22.2 22.3 Long, M.T (2010) Flavivirus Encephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Bertone, J.J (2010) Viral Encephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Wilson, W.D, Pusterla, N (2010) Equine Herpesvirus-1 Myeloencephalopathy in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 25.0 25.1 Sommardahl, C.S (2010) Rabies in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Scaratt, W.K, Jortner, B.S (1985) Neuritis of the cauda equina in a yearling filly. Compend Contin Educ Pract Vet, 7:S197-S202. In: Saville, W.J (2010) Polyneuritis equi in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Granstrom, D.E, Dubey, J.P, Giles, R.C (1994) Equine protozoal myeloencephalitis: biology and epidemiology. In Nakajima, H, Plowright, W, editors: Refereed Proceedings, Newmarket, England, R & W Publications. In: Saville, W.J (2010) Polyneuritis equi in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 28.0 28.1 Nout, Y.S (2010) Equine Degenerative Myeloencephalopathy in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Mayhew, I.G, deLahunta, A, Whitlock, R.H, Krook, L, Tasker, J.B (1978) Spinal cord disease in the horse, Cornell Vet, 68(Suppl 8):1-207. In: Nout, Y.S (2010) Equine Degenerative Myeloencephalopathy in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Jose-Cunilleras, E (2010) Verminous Encephalomyelitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ 31.0 31.1 Byrne, B. A (2010) Diseases of the Cerebellum in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Smith, P.M, Jeffery, N.D (2005) Spinal shock - comparative aspects and clinical relevance. J Vet Intern Med, 19:788-793. In: Nout, Y.S (2010) Central Nervous System Trauma in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Nout, Y.S (2010) Central Nervous System Trauma in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Watson, A.G, Mayhew, I.G (1986) Familial congenital occipitoatlantoaxial malformation (OAAM) in the Arabian horse. Spine, 11:334-339. In: Seino, K.K (2010) Spinal Ataxia in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 3.
- ↑ Sellon, D.C (2010) Miscellaneous Neurologic Disorders in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Talcott, P (2010) Toxicoses causing signs relating to the urinary system in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 22.
- ↑ Talcott, P (2010) Toxicoses causing signs relating to the urinary system in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 22.
- ↑ 38.0 38.1 38.2 38.3 Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial
- ↑ MacKay, R.J (2006) Equine protozoa myeloencephalitis: treatment, prognosis and prevention. Clin Tech Equine Pract, 5:9-16. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.
- ↑ Saville, W.J.A, Reed, S.M, Dubey, J.P (2002) Prevention of equine protozoal myeloencephalitis (EPM). Proceedings of the Annual Convention of the AAEP, 48:181-185.
- ↑ Furr, M, MacKenzie, H, Dubey, J.P (2006) Pretreatment of horses with ponazuril limits infection and neurologic signs resulting from S.neurona. J Parasitol, 92:637-643. In: Furr, M (2010) Equine protozoal myeloencephalitis in Reed, S.M, Bayly, W.M. and Sellon, D.C (2010) Equine Internal Medicine (Third Edition), Saunders, Chapter 12.