Difference between revisions of "Avian Influenza"
| (8 intermediate revisions by 3 users not shown) | |||
| Line 4: | Line 4: | ||
== Introduction == | == Introduction == | ||
| − | Avian influenza (AI) is a notifiable disease. It is part of the [[Orthomyxoviridae]] family, possessing a single negative sense RNA strand. Within the influenza [[viruses|virus]] family there are 3 subtypes; A, B and C, with only A causing disease in birds. Type A can then be further subdivided based on the haemagglutinin (HA) and neuraminidase (N) envelope glycoproteins present, with subtype antigens H1-17 and N1-9. Each virus possesses one HA and one N antigen. Each isolate can then be further subdivided into viral lineages called clades. | + | Avian influenza (AI) is a notifiable disease. It is part of the [[Orthomyxoviridae]] family, possessing a single negative sense RNA strand. Within the influenza [[viruses|virus]] family there are 3 subtypes; A, B and C, with only A causing disease in birds. Type A can then be further subdivided based on the haemagglutinin (HA) and neuraminidase (N) envelope glycoproteins present, with subtype antigens H1-17 and N1-9. Each virus possesses one HA and one N antigen. Each isolate can then be further subdivided into viral lineages called clades <ref> Mahy, B.W.J., Meulen, V.T.(2007)''Topley & Wilson’s Microbiology and Microbial Infections Virology Vol. 1.'' Amer. Soc. for Microbiology; 10th edition </ref> |
| + | [[File: EM of influenza virus.jpg|right|200px|thumb|EM of influenza virus]] | ||
<br><br> | <br><br> | ||
| − | Influenza A viruses affecting birds are divided into two groups based of the severity of clinical disease; highly pathogenic avian influenza (HPAI) and low pathogenic avian influenza (LPAI). HPAI viruses are found within (though not all of) H5 and H7 subtypes. HPAI viruses are thought to be a result of mutations within an LPAI strain. HPAI is defined by the ability to infect and kill chickens using a standardized dose given intravenously (World Organization for Animal Health, 2006). The mutation occurs after the virus has moved from the wild bird host into the poultry population and may take days to months to occur. The longer the virus persists the more likely it is to adapt and mutate into a highly pathogenic strain, and once in poultry in can then spread to other species. | + | Influenza A viruses affecting birds are divided into two groups based of the severity of clinical disease; highly pathogenic avian influenza (HPAI) and low pathogenic avian influenza (LPAI). HPAI viruses are found within (though not all of) H5 and H7 subtypes. HPAI viruses are thought to be a result of mutations within an LPAI strain. HPAI is defined by the ability to infect and kill chickens using a standardized dose given intravenously (''World Organization for Animal Health, 2006''). The mutation occurs after the virus has moved from the wild bird host into the poultry population and may take days to months to occur. The longer the virus persists the more likely it is to adapt and mutate into a highly pathogenic strain, and once in poultry in can then spread to other species.<ref name="suarez"> Suarez, D.L. (2010), ''Avian influenza: our current understanding, Animal Health Research Reviews 11(1); 19–33''</ref> |
<br><br> | <br><br> | ||
| − | Initially AI cases were found to decrease as the ambient temperature increased but in 2009 cases were documented all year round with increased cases during the warmer months of the year. AI viruses can persist for long periods of time at low temperatures in water, and therefore can reinfect migratory water fowl in the spring and lead to further spread. Geographical separation of the virus can also increase independent evolution of the virus and potentially increase virulence. | + | Initially AI cases were found to decrease as the ambient temperature increased but in 2009 cases were documented all year round with increased cases during the warmer months of the year.<ref name="abdelwhab"> Abdelwhab, E.M., Hafez, H.M. (2011), ''An overview of the epidemic of highly pathogenic H5N1 avian influenza virus in Egypt: epidemiology and control challenges, Epidemiol. Infect. 139, 647–657''.</ref> AI viruses can persist for long periods of time at low temperatures in water, and therefore can reinfect migratory water fowl in the spring and lead to further spread. <ref> Zhang G, Shoham D, Gilichinsky D, Davydov S, Castello J.D., Rogers S.O. (2006), ''Evidence of influenza A virus RNA in Siberian lake ice. Journal of Virology 80: 12229–12235''.</ref> Geographical separation of the virus can also increase independent evolution of the virus and potentially increase virulence. |
<br><br> | <br><br> | ||
===AI Spread=== | ===AI Spread=== | ||
| − | Wild birds (in particular aquatic birds) are the main reservoir for the virus, and hence are responsible for its continuous spread and maintenance, which is easy and quick. The migration of many wild birds across distances has led to long distance spread and the introduction of AI into other countries. Different species of wild birds have different genetic pools of virus and different susceptibilities. Most infection within Europe has been detected in dead wild birds. A majority of cases, especially in developing countries, have been the result of secondary spread within poultry, most of which is human mediated. Most AI viruses are well adapted to their host species, so when they infect a new species they replicate and transmit poorly. Domestic poultry (especially ducks) are reservoirs for HPAI, and, in some cases, birds can produce the virus for weeks with no clinical signs. | + | Wild birds (in particular aquatic birds) are the main reservoir for the virus, and hence are responsible for its continuous spread and maintenance, which is easy and quick. The migration of many wild birds across distances has led to long distance spread and the introduction of AI into other countries. Different species of wild birds have different genetic pools of virus and different susceptibilities. Most infection within Europe has been detected in dead wild birds. A majority of cases, especially in developing countries, have been the result of secondary spread within poultry, most of which is human mediated.<ref> Biosecurity for Highly Pathogenic Avian Influenza Issues and options (2008) FAO Animal Production and Health Paper No. 165 </ref> Most AI viruses are well adapted to their host species, so when they infect a new species they replicate and transmit poorly. Domestic poultry (especially ducks) are reservoirs for HPAI, and, in some cases, birds can produce the virus for weeks with no clinical signs. |
<br><br> | <br><br> | ||
| − | AI is spread by movement of birds, direct contact with respiratory secretions or faeces as well as via fomites (inanimate objects). AI can also be transmitted by eating uncooked infected bird products, including uncooked eggs. AI virus has been found on the surface of eggs but so far there has been no evidence of transmission to people by the consumption of egg products. The practice of manure spreading also increases the possibility of disease transmission. | + | AI is spread by movement of birds, direct contact with respiratory secretions or faeces as well as via fomites (inanimate objects). AI can also be transmitted by eating uncooked infected bird products, including uncooked eggs. AI virus has been found on the surface of eggs but so far there has been no evidence of transmission to people by the consumption of egg products.<ref> Diaro, M.D., Elelu, N., (2013) ''Knowledge and preventive practices related to Avian influenza among livestock farmers and poultry traders in Ikorodu, Lagos state, Nigeria, Journal of Public Health and Epidemiology, Vol. 5(4), 202-207, April'' </ref> The practice of manure spreading also increases the possibility of disease transmission. |
<br><br> | <br><br> | ||
===Recent Outbreaks=== | ===Recent Outbreaks=== | ||
| − | H5N1 is an HPAI strain that can persist in wild bird populations. In April 05 this strain caused high mortality in ducks and gulls in Qinghai Lake in China. Wild bird migration led to the virus being carried to Europe and Africa and over winter 2006 a large number of wild birds were found to be infected. Migratory birds in Egypt tested positive for H5N1 three months before the outbreak in poultry. The virus is thought to still be present in wild bird populations but at a lower level. This subtype proved harder to control due to the maintenance of infection within wild birds and the increased susceptibility of poultry to the strain (as shown by a low MID50, meaning that only a small amount of virus is needed to produce infection). | + | H5N1 is an HPAI strain that can persist in wild bird populations. In April 05 this strain caused high mortality in ducks and gulls in Qinghai Lake in China. Wild bird migration led to the virus being carried to Europe and Africa and over winter 2006 a large number of wild birds were found to be infected. Migratory birds in Egypt tested positive for H5N1 three months before the outbreak in poultry. The virus is thought to still be present in wild bird populations but at a lower level. This subtype proved harder to control due to the maintenance of infection within wild birds and the increased susceptibility of poultry to the strain (as shown by a low MID50, meaning that only a small amount of virus is needed to produce infection)<ref name="suarez"/> .H5N1 has spread to over 60 countries and is currently endemic in China, Egypt, Vietnam, India, Bangladesh and Indonesia.<ref name="spackman"> Spackman E., Swayne, D.E. (2013), ''Vaccination of gallinaceous poultry for H5N1 highly pathogenic avian influenza: Current questions and new technology, Virus Research, March 21st.''</ref> |
<br><br> | <br><br> | ||
| − | The most recent cases reported in China on the 29th March 2013 involve the H7N9 subtype, which has been shown to be more virulent in people than poultry. Currently no animal outbreaks have been identified in the area surrounding the confirmed cases and only a small proportion of birds have tested positive for the virus; however 77% of those people infected have been exposed to poultry/swine (including live bird markets). Three family clusters of 2-3 cases each have been identified where limited human to human transmission may have occurred. | + | The most recent cases reported in China on the 29th March 2013 involve the H7N9 subtype, which has been shown to be more virulent in people than poultry. Currently no animal outbreaks have been identified in the area surrounding the confirmed cases and only a small proportion of birds have tested positive for the virus; however 77% of those people infected have been exposed to poultry/swine (including live bird markets). Three family clusters of 2-3 cases each have been identified where limited human to human transmission may have occurred.<ref> ''Centers for Disease Control and Prevention: Morbidity and Mortality Weekly Report, Emergence of Avian Influenza A(H7N9) Virus Causing Severe Human Illness — China, February–April 2013, May 10, 2013 / 62(18);366-371'' </ref> <ref name="Koopmans"> Koopmans, M., de Jong, M.D. (2013), ''Avian influenza A H7N9 in Zhejiang, China, The Lancet, 26th April 2013''.</ref> |
<br><br> | <br><br> | ||
| − | At the moment it is thought that H7N9 was transmitted from healthy poultry or swine to people either directly or through contaminated environments. As few H7N9 positive birds have been detected, this may indicate that the virus is widespread in poultry and is asymptomatic which could lead to silent spread of the virus. | + | At the moment it is thought that H7N9 was transmitted from healthy poultry or swine to people either directly or through contaminated environments.<ref> Qun Li, M.D., Lei Zhou, M.D., Minghao Zhou, Ph.D., Zhiping Chen, M.D., Furong Li, M.D., Huanyu Wu, M.D., Nijuan Xiang, M.D., Enfu Chen, M.P.H., Fenyang Tang, M.D., Dayan Wang, M.D., Ling Meng, M.D., Zhiheng Hong, M.D., Wenxiao Tu, M.D., Yang Cao, M.D., Leilei Li, Ph.D., Fan Ding, M.D., Bo Liu, M.D., Mei Wang, M.D., Rongheng Xie, M.D., Rongbao Gao, M.D., Xiaodan Li, M.D., Tian Bai, M.D., Shumei Zou, M.D., Jun He, M.D., Jiayu Hu, M.D., Yangting Xu, M.D., Chengliang Chai, M.D., Shiwen Wang, M.D., Yongjun Gao, M.D., Lianmei Jin, M.D., Yanping Zhang, M.D., Huiming Luo, M.D., Hongjie Yu, M.D., M.P.H., Lidong Gao, M.D., Xinghuo Pang, M.D., Guohua Liu, M.D., Yuelong Shu, Ph.D., Weizhong Yang, M.D., Timothy M. Uyeki, M.D., M.P.H., M.P.P., Yu Wang, M.D., Fan Wu, M.D., and Zijian Feng, M.D., M.P.H. (2013)''Preliminary Report: Epidemiology of the Avian Influenza A (H7N9) Outbreak in China, The New England Journal of Medicine, April 24th 2013'' </ref> As few H7N9 positive birds have been detected, this may indicate that the virus is widespread in poultry and is asymptomatic which could lead to silent spread of the virus. |
<br><br> | <br><br> | ||
| − | The complete virus is a recombination of three viruses found in Asia, H7 of the virus has been found to be closest to that found in domestic ducks in Zhejiang and the N9 closest to the wild bird strain in South Korea. Genetic changes have also been found that lead to increased virus binding and replication in mammalian respiratory cells and thus increased severity of infection. The virus has been shown to be weakly pathogenic in poultry and testing of different populations for H7N9 specific antibodies may be helpful in finding the source, though viruses with H7 HA may not trigger a strong antibody response. No cases have been reported outside of China. | + | The complete virus is a recombination of three viruses found in Asia, H7 of the virus has been found to be closest to that found in domestic ducks in Zhejiang and the N9 closest to the wild bird strain in South Korea. Genetic changes have also been found that lead to increased virus binding and replication in mammalian respiratory cells and thus increased severity of infection. The virus has been shown to be weakly pathogenic in poultry and testing of different populations for H7N9 specific antibodies may be helpful in finding the source, though viruses with H7 HA may not trigger a strong antibody response. No cases have been reported outside of China.<ref name="Koopmans"/> |
==Signalment== | ==Signalment== | ||
| − | There is a higher risk of LPAI on farms housing ducks, geese and game birds as compared to chickens, turkeys and indoor layer farms. This may be due to the rearing methods, as birds reared outside have a higher risk of coming into contact with wildfowl and thus becoming infected with LPAI. Contaminated drinking water, including water that wild birds have access to, increases the risk of infection, as does feeding uncooked meat and offal. Turkeys and ducks appear more susceptible to AI, as are many gallinaceous species. LPAI has been shown to be present in low levels in turkeys but HPAI rarely found, only five cases of HPAI since 1959 have been found to result primarily from turkeys. HPAI viruses are well adapted to poultry. Wild pigeons may not be as susceptible to AI as other wild birds. Psittacine birds are rarely affected and viruses found in ratites show a low level of virulence to chickens. The density of lamellae and feeding style within ducks has been shown to be associated with AI infection, suggesting feeding methods may have an effect on exposure to AI virus. AI has also been detected in asymptomatic swine and donkeys. | + | There is a higher risk of LPAI on farms housing ducks, geese and game birds as compared to chickens, turkeys and indoor layer farms. This may be due to the rearing methods, as birds reared outside have a higher risk of coming into contact with wildfowl and thus becoming infected with LPAI. Contaminated drinking water, including water that wild birds have access to, increases the risk of infection, as does feeding uncooked meat and offal. Turkeys and ducks appear more susceptible to AI <ref> Gonzales J.L., Stegeman, J.A., Koch, G., de Wit, S.J., Elbers, A.R.W.(2013), ''Rate of introduction of a low pathogenic avian influenza virus infection in different poultry production sectors in the Netherlands, Influenza and Other Respiratory Viruses Volume 7, Issue 1, pages 6–10, January 2013'' </ref>, as are many gallinaceous species. LPAI has been shown to be present in low levels in turkeys but HPAI rarely found, only five cases of HPAI since 1959 have been found to result primarily from turkeys. HPAI viruses are well adapted to poultry. Wild pigeons may not be as susceptible to AI as other wild birds. Psittacine birds are rarely affected and viruses found in ratites show a low level of virulence to chickens <ref> Alexander, D.J. (2000), ''A Review of avian influenza in different bird species, Veterinary Microbiology, Volume 74, Issues 1–2, 22 May 2000, Pages 3–13'' </ref> . The density of lamellae and feeding style within ducks has been shown to be associated with AI infection, suggesting feeding methods may have an effect on exposure to AI virus <ref> Hill N.J., Takekawa J.Y., Cardona C.J., Ackerman J.T., Schultz A.K., Spragens K.A. and Boyce W.M. (2010). ''Waterfowl ecology and avian influenza in California: do host traits inform us about viral occurrence?, Avian Diseases 54: 426–432.'' </ref>. AI has also been detected in asymptomatic swine and donkeys. |
== Clinical Signs == | == Clinical Signs == | ||
| Line 31: | Line 32: | ||
LPAI viruses cause milder disease, most commonly respiratory symptoms (e.g. rales, coughing) combined with reduced egg production and depression, though clinical signs can range from none to death. Other signs can include swelling of the infraorbital sinuses, pyrexia and loss of appetite. If other bacteria or viruses (e.g. ''[[Pasteurella species|Pasteurella spp]]'', [[Newcastle Disease Virus|Newcastle disease]], ''[[Mycoplasma gallisepticum|Mycoplasma spp]]'', ''[[Escherichia coli]]'') are present along with LPAI the consequences of infection can be more serious, often causing high mortality. The age, immune status and species of the infected bird can also have an impact on the severity of disease, as can the environment the bird is housed in. Many flocks are infected with LPAI every year and are only recognised due to seroconversion as the disease is asymptomatic. Most infections are transient due to lack of host adaptation, though some establish due to virus variation. | LPAI viruses cause milder disease, most commonly respiratory symptoms (e.g. rales, coughing) combined with reduced egg production and depression, though clinical signs can range from none to death. Other signs can include swelling of the infraorbital sinuses, pyrexia and loss of appetite. If other bacteria or viruses (e.g. ''[[Pasteurella species|Pasteurella spp]]'', [[Newcastle Disease Virus|Newcastle disease]], ''[[Mycoplasma gallisepticum|Mycoplasma spp]]'', ''[[Escherichia coli]]'') are present along with LPAI the consequences of infection can be more serious, often causing high mortality. The age, immune status and species of the infected bird can also have an impact on the severity of disease, as can the environment the bird is housed in. Many flocks are infected with LPAI every year and are only recognised due to seroconversion as the disease is asymptomatic. Most infections are transient due to lack of host adaptation, though some establish due to virus variation. | ||
<br><br> | <br><br> | ||
| − | By contrast, HPAI infection may only be recognised by sudden onset mortality within the flock, which can reach 100% within a couple of days. If the birds are still alive symptoms can include those of LPAI (though egg laying has often stopped) and excessive lacrimation, sinusitis, oedema of the head, subcutaneous haemorrhage, cyanosis of the skin (including comb and wattles), diarrhoea and occasional neurological signs. Severity of signs depends on the species and strain of the virus, for example some ducks infected with HPAI rarely showed clinical signs. | + | By contrast, HPAI infection may only be recognised by sudden onset mortality within the flock, which can reach 100% within a couple of days. If the birds are still alive symptoms can include those of LPAI (though egg laying has often stopped) and excessive lacrimation, sinusitis, oedema of the head, subcutaneous haemorrhage, cyanosis of the skin (including comb and wattles), diarrhoea and occasional neurological signs. Severity of signs depends on the species and strain of the virus, for example some ducks infected with HPAI rarely showed clinical signs.<ref name="alexander"> Alexander, D.J.(2008) , ''Avian Influenza – Diagnosis, Zoonoses and Public Health Volume 55, Issue 1, pages 16–23, February 2008'' </ref> |
== Diagnosis == | == Diagnosis == | ||
| − | Laboratory diagnosis is essential when dealing with suspected cases of AI due to the lack of classical clinical signs, zoonotic potential, and need to differentiate between HPAI and LPAI as well as the virus subtype. The diagnosis is based on isolation and characterisation of the virus. Tracheal/ cloacal swabs or faeces are taken from live birds and suspended in antibiotic solution before being inoculated into the allantoic cavity of 9-11 day old embroyanted chicks. Taking lower respiratory tract samples is important, as the virus may not be found in the upper respiratory tract. Faecal or organ samples from dead birds can also be used. Following incubation the allantoic fluid is tested for haemagglutination, a positive result (i.e. haemagglutination is present) indicating viral infection. An immunodiffusion test can be used to confirm the presence of influenza A virus, using antiserum to the nucleocapsid or matrix antigens. Polyclonal chicken antisera can be used to further identify the virus subtype by observing which specific antiserum inhibits the haemagglutinating activity of the virus (haemagglutination inhibition) | + | Laboratory diagnosis is essential when dealing with suspected cases of AI due to the lack of classical clinical signs, zoonotic potential, and need to differentiate between HPAI and LPAI as well as the virus subtype. The diagnosis is based on isolation and characterisation of the virus. Tracheal/ cloacal swabs or faeces are taken from live birds and suspended in antibiotic solution before being inoculated into the allantoic cavity of 9-11 day old embroyanted chicks. Taking lower respiratory tract samples is important, as the virus may not be found in the upper respiratory tract. Faecal or organ samples from dead birds can also be used. Following incubation the allantoic fluid is tested for haemagglutination, a positive result (i.e. haemagglutination is present) indicating viral infection. An immunodiffusion test can be used to confirm the presence of influenza A virus, using antiserum to the nucleocapsid or matrix antigens. Polyclonal chicken antisera can be used to further identify the virus subtype by observing which specific antiserum inhibits the haemagglutinating activity of the virus (haemagglutination inhibition)<ref name="alexander"/> |
<br><br> | <br><br> | ||
| − | Virulence assessment can be performed by injecting chickens with infective allantoic fluid and observing the presence/absence and severity of disease for 10 days. | + | Virulence assessment can be performed by injecting chickens with infective allantoic fluid and observing the presence/absence and severity of disease for 10 days.<ref name="alexander"/> |
<br><br> | <br><br> | ||
Paired serum samples can be taken in order to identify seroconversion. One sample is taken in the acute phase of infection before antibodies are produced and another 2-3 weeks later. A fourfold increase in antibody levels (usually identified by haemagglutination inhibition) will show that infection with the virus has occurred. This can only provide a retrospective diagnosis but can be useful in identifying which flocks have been exposed to AI, especially in cases where it is an asymptomatic infection. | Paired serum samples can be taken in order to identify seroconversion. One sample is taken in the acute phase of infection before antibodies are produced and another 2-3 weeks later. A fourfold increase in antibody levels (usually identified by haemagglutination inhibition) will show that infection with the virus has occurred. This can only provide a retrospective diagnosis but can be useful in identifying which flocks have been exposed to AI, especially in cases where it is an asymptomatic infection. | ||
<br><br> | <br><br> | ||
Due to continual antigenic drift and shift specificity and sensitivity of diagnostics is a big problem. | Due to continual antigenic drift and shift specificity and sensitivity of diagnostics is a big problem. | ||
| + | |||
| + | ==Treatment== | ||
| + | There is no treatment for HPAI in birds, and all affected birds should be culled as well as any birds in contact with diseased stock. | ||
== Control == | == Control == | ||
| − | + | Within developed countries a combination of vaccination, culling, movement restrictions and disinfection are used. Once the disease is endemic it is harder to control. During the H5N1 outbreak in Egypt these methods were unsuccessful so mass vaccination (with inactivated H5 vaccines), surveillance and pre emptive culling of birds was carried out alongside the above methods. A problem was encountered with the disposal of carcasses post culling (both the speed of disposal and the methods used) which may have led to increased spread. Dead infected birds are often eaten by stray dogs and cats which can increase circulation of the virus. Since the 1st of July 2010 there has been a ban on selling live poultry in Egypt and only licensed slaughter houses are allowed to handle poultry.<ref name="abdelwhab"/> | |
| − | + | <br><br> | |
| − | + | The presence of live bird markets and live bird trade in many countries has made control of AI harder. Live bird markets can act as viral reservoirs to maintain and increase the spread of the disease, both through fomites and movement of infected birds. This increase in circulation can aid the development of more, potentially zoonotic, strains. Fragmenting the live bird market network through disinfecting both the market (daily) and the vehicles coming in and out would greatly reduce the spread. The concept of ‘rest days’ to limit spread has also been introduced in some areas. Previously a ban on live bird markets has only served to result in illegal bird markets, which have resulted in further spread of AI both due to the lack of knowledge of where these were taking place and the lack of control over biosecurity. Education of the local population plays a key role in the reduction of the spread of AI. Bioexclusion (excluding the virus) in farms and villages should be the aim, whereas biocontainment (containing the virus) should be the aim with markets. | |
| − | + | ===Vaccination=== | |
| − | + | Vaccination against AI is usually only used in order to help control an outbreak. A majority of the vaccines used are inactivated vaccines, though some are starting to use vectored vaccines. A reverse genetic engineered reassortant (rg) vaccine is also available. This vaccine has been updated twice due to changing field viruses.<ref name="spackman"/> | |
| − | + | <br><br> | |
| − | + | The duration of immunity from vaccination is largely unknown due to the logistical problems of studying this. Current studies vary from 12 weeks to 138 weeks with different vaccines. The effect of repeat dosing is also unclear, though dosing twice has shown an increase in immunity from 1 to 10 months.<ref name="spackman"/> | |
| − | + | <br><br> | |
| + | Within the commercial sector breeding birds and layers are usually the only birds vaccinated due to the high cost. Also, the addition of adjuvants (e.g. oil emulsion) requires a withdrawal time that is usually longer than the lifespan of a meat chicken thus meaning that, in most cases, it is economically unviable to vaccinate. Egypt has however vaccinated meat birds as part of a routine vaccination program. Hong Kong is the only place that has achieved national flock immunity.<ref name="spackman"/> In developing countries the vaccination rate within village poultry is too low to achieve population immunity, and proper vaccine storage is also a problem. | ||
| + | <br><br> | ||
| + | Suboptimal vaccination, and thus incomplete immunity, can lead to an increase in antigenic drift by increasing immune pressure exerted in hosts and can also increase the rate at which the virus is able to cross species. It could also lead to clinical symptoms being masked and thus increasing disease spread. Suboptimal immunity can occur through a number of ways: host immunosupression, vaccine spoilage, inadequate dosing, poor antigenic match between vaccine and virus, low vaccination uptake in the population or exposure to the virus before full immunity has developed. | ||
| + | <br><br> | ||
| + | AI vaccines are constantly being updated to cover for new strains of AI due to antigenic drift. Vaccines are currently being developed that target the M2 protein, which is conserved among different subtypes of virus. Subunit vaccines are being developed but the cost would inhibit use in poultry and there is a lack of data on whether it would provide protection in chickens.<ref name="spackman"/> | ||
| + | <br><br> | ||
| + | rNDV (recombinant Newcastle Disease virus) vaccines may offer a solution to the labour intensive administration of traditional vaccines in that they can be administered through drinking water. NDV vaccination is routine worldwide, and NDV replicates in the same tissues as AI therefore can confer better immunity at smaller doses than would otherwise be required. NDV will also replicate in chickens and turkeys. However, maternal antibodies to the vector will interfere with immunity. Fowl poxvirus vectored vaccines are licensed for use in the US and have been used in China and Mexico.<ref name="spackman"/> | ||
| + | <br><br> | ||
| + | HI tests can be used post vaccination to monitor the immune response, though HI tests used after vaccination in Egypt showed the antibodies produced by the vaccine to have no cross reactivity with field antigens. Serum from vaccinated birds from one strain found in Egypt showed no reaction with other H5 based antigens of vaccine strains found in Egypt, thus showing the importance of using the correct field antigens present when developing vaccines. Monoclonal antibody ELISA tests based on the H5N1 Asian strain did not detect the Egyptian variant either.<ref name="abdelwhab"/> | ||
| + | <br><br> | ||
| + | Inactivated vaccinations have played an important role in H9 control in China, though AI still persists in chicken populations, even those that have been vaccinated, due to genetic variation. Vaccination of poultry can decrease disease and virus shedding if birds become infected, and can also lead to an increase in the amount of virus needed to infect vaccinated birds. | ||
| + | <br><br> | ||
| + | Within the countries that have endemic H5N1 Bangladesh and India are the only countries not to have vaccination programs, though Bangladesh is in the process of developing a program.<ref name="spackman"/> | ||
| + | <br><br> | ||
| + | A majority of the vaccine research being performed is related to human vaccines due to the public health risks associated with AI. DNA vaccines are currently being developed, though due to cost and the need for multiple doses to be individually administered it is unlikely they will be used in poultry. | ||
| + | <br><br> | ||
| + | The development of DIVA system (differentiating infected from vaccinated animals) is currently an important focus of research due to trade and political issues. | ||
== References == | == References == | ||
| − | + | <references /> | |
| − | + | <br><br> | |
| − | + | [http://www.oie.int/en/animal-health-in-the-world/web-portal-on-avian-influenza/ OIE Avian Influenza] accessed June 23, 2013 | |
| − | + | <br><br> | |
| − | + | SH Lu, XH Xi, YF Zheng, Y Cao, XN Liu, HZ Lu (2013) ''Analysis of the clinical characteristics and treatment of two patients with avian influenza virus (H7N9). Bioscience trends, 2013 ;7(2):109-112.'' | |
| − | + | <br><br> | |
| − | + | [http://www.defra.gov.uk/animal-diseases/a-z/bird-flu/ DEFRA Avian Influenza] accessed June 23, 2013 | |
| − | + | <br><br> | |
| − | + | Fournié, G., Guitian, J., Desvaux, S., Cuong, V.C., Dung, D.H., Pfeiffer, D.U., Mangtani, P., Ghani, A.C.(2013), ''Interventions for avian influenza A (H5N1) risk management in live bird market networks, PNAS, May 6, 2013, doi: 10.1073/pnas.1220815110'' | |
| − | + | <br><br> | |
| + | Chen R.A., Lai H.Z., Li L., Liu Y.P., Pan W.L., Zhang W.Y., Xu J.H., He D.S., Tang Z.X.(2013), ''Genetic variation and phylogenetic analysis of hemagglutinin genes of H9 avian influenza viruses isolated in China during 2010-2012. Vet Microbiol. 2013 Apr 12'' | ||
| Line 70: | Line 92: | ||
{{OpenPages}} | {{OpenPages}} | ||
| − | [[Category:Orthomyxoviridae]] [[Category:Avian_Viruses]] [[Category:Respiratory Diseases - Birds]][[Category:Alimentary Diseases - Birds]][[Category:Neurological Diseases - Birds]][[Category:Expert_Review - Bird]] | + | [[Category:Orthomyxoviridae]] [[Category:Avian_Viruses]] [[Category:Respiratory Diseases - Birds]][[Category:Alimentary Diseases - Birds]][[Category:Neurological Diseases - Birds]][[Category:Expert_Review - Bird]][[Category:One Health]] |
Latest revision as of 14:27, 2 July 2013
Also know as: Fowl Plague
Introduction
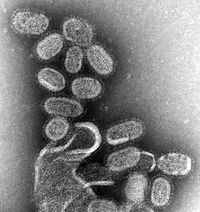
Avian influenza (AI) is a notifiable disease. It is part of the Orthomyxoviridae family, possessing a single negative sense RNA strand. Within the influenza virus family there are 3 subtypes; A, B and C, with only A causing disease in birds. Type A can then be further subdivided based on the haemagglutinin (HA) and neuraminidase (N) envelope glycoproteins present, with subtype antigens H1-17 and N1-9. Each virus possesses one HA and one N antigen. Each isolate can then be further subdivided into viral lineages called clades [1]
Influenza A viruses affecting birds are divided into two groups based of the severity of clinical disease; highly pathogenic avian influenza (HPAI) and low pathogenic avian influenza (LPAI). HPAI viruses are found within (though not all of) H5 and H7 subtypes. HPAI viruses are thought to be a result of mutations within an LPAI strain. HPAI is defined by the ability to infect and kill chickens using a standardized dose given intravenously (World Organization for Animal Health, 2006). The mutation occurs after the virus has moved from the wild bird host into the poultry population and may take days to months to occur. The longer the virus persists the more likely it is to adapt and mutate into a highly pathogenic strain, and once in poultry in can then spread to other species.[2]
Initially AI cases were found to decrease as the ambient temperature increased but in 2009 cases were documented all year round with increased cases during the warmer months of the year.[3] AI viruses can persist for long periods of time at low temperatures in water, and therefore can reinfect migratory water fowl in the spring and lead to further spread. [4] Geographical separation of the virus can also increase independent evolution of the virus and potentially increase virulence.
AI Spread
Wild birds (in particular aquatic birds) are the main reservoir for the virus, and hence are responsible for its continuous spread and maintenance, which is easy and quick. The migration of many wild birds across distances has led to long distance spread and the introduction of AI into other countries. Different species of wild birds have different genetic pools of virus and different susceptibilities. Most infection within Europe has been detected in dead wild birds. A majority of cases, especially in developing countries, have been the result of secondary spread within poultry, most of which is human mediated.[5] Most AI viruses are well adapted to their host species, so when they infect a new species they replicate and transmit poorly. Domestic poultry (especially ducks) are reservoirs for HPAI, and, in some cases, birds can produce the virus for weeks with no clinical signs.
AI is spread by movement of birds, direct contact with respiratory secretions or faeces as well as via fomites (inanimate objects). AI can also be transmitted by eating uncooked infected bird products, including uncooked eggs. AI virus has been found on the surface of eggs but so far there has been no evidence of transmission to people by the consumption of egg products.[6] The practice of manure spreading also increases the possibility of disease transmission.
Recent Outbreaks
H5N1 is an HPAI strain that can persist in wild bird populations. In April 05 this strain caused high mortality in ducks and gulls in Qinghai Lake in China. Wild bird migration led to the virus being carried to Europe and Africa and over winter 2006 a large number of wild birds were found to be infected. Migratory birds in Egypt tested positive for H5N1 three months before the outbreak in poultry. The virus is thought to still be present in wild bird populations but at a lower level. This subtype proved harder to control due to the maintenance of infection within wild birds and the increased susceptibility of poultry to the strain (as shown by a low MID50, meaning that only a small amount of virus is needed to produce infection)[2] .H5N1 has spread to over 60 countries and is currently endemic in China, Egypt, Vietnam, India, Bangladesh and Indonesia.[7]
The most recent cases reported in China on the 29th March 2013 involve the H7N9 subtype, which has been shown to be more virulent in people than poultry. Currently no animal outbreaks have been identified in the area surrounding the confirmed cases and only a small proportion of birds have tested positive for the virus; however 77% of those people infected have been exposed to poultry/swine (including live bird markets). Three family clusters of 2-3 cases each have been identified where limited human to human transmission may have occurred.[8] [9]
At the moment it is thought that H7N9 was transmitted from healthy poultry or swine to people either directly or through contaminated environments.[10] As few H7N9 positive birds have been detected, this may indicate that the virus is widespread in poultry and is asymptomatic which could lead to silent spread of the virus.
The complete virus is a recombination of three viruses found in Asia, H7 of the virus has been found to be closest to that found in domestic ducks in Zhejiang and the N9 closest to the wild bird strain in South Korea. Genetic changes have also been found that lead to increased virus binding and replication in mammalian respiratory cells and thus increased severity of infection. The virus has been shown to be weakly pathogenic in poultry and testing of different populations for H7N9 specific antibodies may be helpful in finding the source, though viruses with H7 HA may not trigger a strong antibody response. No cases have been reported outside of China.[9]
Signalment
There is a higher risk of LPAI on farms housing ducks, geese and game birds as compared to chickens, turkeys and indoor layer farms. This may be due to the rearing methods, as birds reared outside have a higher risk of coming into contact with wildfowl and thus becoming infected with LPAI. Contaminated drinking water, including water that wild birds have access to, increases the risk of infection, as does feeding uncooked meat and offal. Turkeys and ducks appear more susceptible to AI [11], as are many gallinaceous species. LPAI has been shown to be present in low levels in turkeys but HPAI rarely found, only five cases of HPAI since 1959 have been found to result primarily from turkeys. HPAI viruses are well adapted to poultry. Wild pigeons may not be as susceptible to AI as other wild birds. Psittacine birds are rarely affected and viruses found in ratites show a low level of virulence to chickens [12] . The density of lamellae and feeding style within ducks has been shown to be associated with AI infection, suggesting feeding methods may have an effect on exposure to AI virus [13]. AI has also been detected in asymptomatic swine and donkeys.
Clinical Signs
LPAI viruses cause milder disease, most commonly respiratory symptoms (e.g. rales, coughing) combined with reduced egg production and depression, though clinical signs can range from none to death. Other signs can include swelling of the infraorbital sinuses, pyrexia and loss of appetite. If other bacteria or viruses (e.g. Pasteurella spp, Newcastle disease, Mycoplasma spp, Escherichia coli) are present along with LPAI the consequences of infection can be more serious, often causing high mortality. The age, immune status and species of the infected bird can also have an impact on the severity of disease, as can the environment the bird is housed in. Many flocks are infected with LPAI every year and are only recognised due to seroconversion as the disease is asymptomatic. Most infections are transient due to lack of host adaptation, though some establish due to virus variation.
By contrast, HPAI infection may only be recognised by sudden onset mortality within the flock, which can reach 100% within a couple of days. If the birds are still alive symptoms can include those of LPAI (though egg laying has often stopped) and excessive lacrimation, sinusitis, oedema of the head, subcutaneous haemorrhage, cyanosis of the skin (including comb and wattles), diarrhoea and occasional neurological signs. Severity of signs depends on the species and strain of the virus, for example some ducks infected with HPAI rarely showed clinical signs.[14]
Diagnosis
Laboratory diagnosis is essential when dealing with suspected cases of AI due to the lack of classical clinical signs, zoonotic potential, and need to differentiate between HPAI and LPAI as well as the virus subtype. The diagnosis is based on isolation and characterisation of the virus. Tracheal/ cloacal swabs or faeces are taken from live birds and suspended in antibiotic solution before being inoculated into the allantoic cavity of 9-11 day old embroyanted chicks. Taking lower respiratory tract samples is important, as the virus may not be found in the upper respiratory tract. Faecal or organ samples from dead birds can also be used. Following incubation the allantoic fluid is tested for haemagglutination, a positive result (i.e. haemagglutination is present) indicating viral infection. An immunodiffusion test can be used to confirm the presence of influenza A virus, using antiserum to the nucleocapsid or matrix antigens. Polyclonal chicken antisera can be used to further identify the virus subtype by observing which specific antiserum inhibits the haemagglutinating activity of the virus (haemagglutination inhibition)[14]
Virulence assessment can be performed by injecting chickens with infective allantoic fluid and observing the presence/absence and severity of disease for 10 days.[14]
Paired serum samples can be taken in order to identify seroconversion. One sample is taken in the acute phase of infection before antibodies are produced and another 2-3 weeks later. A fourfold increase in antibody levels (usually identified by haemagglutination inhibition) will show that infection with the virus has occurred. This can only provide a retrospective diagnosis but can be useful in identifying which flocks have been exposed to AI, especially in cases where it is an asymptomatic infection.
Due to continual antigenic drift and shift specificity and sensitivity of diagnostics is a big problem.
Treatment
There is no treatment for HPAI in birds, and all affected birds should be culled as well as any birds in contact with diseased stock.
Control
Within developed countries a combination of vaccination, culling, movement restrictions and disinfection are used. Once the disease is endemic it is harder to control. During the H5N1 outbreak in Egypt these methods were unsuccessful so mass vaccination (with inactivated H5 vaccines), surveillance and pre emptive culling of birds was carried out alongside the above methods. A problem was encountered with the disposal of carcasses post culling (both the speed of disposal and the methods used) which may have led to increased spread. Dead infected birds are often eaten by stray dogs and cats which can increase circulation of the virus. Since the 1st of July 2010 there has been a ban on selling live poultry in Egypt and only licensed slaughter houses are allowed to handle poultry.[3]
The presence of live bird markets and live bird trade in many countries has made control of AI harder. Live bird markets can act as viral reservoirs to maintain and increase the spread of the disease, both through fomites and movement of infected birds. This increase in circulation can aid the development of more, potentially zoonotic, strains. Fragmenting the live bird market network through disinfecting both the market (daily) and the vehicles coming in and out would greatly reduce the spread. The concept of ‘rest days’ to limit spread has also been introduced in some areas. Previously a ban on live bird markets has only served to result in illegal bird markets, which have resulted in further spread of AI both due to the lack of knowledge of where these were taking place and the lack of control over biosecurity. Education of the local population plays a key role in the reduction of the spread of AI. Bioexclusion (excluding the virus) in farms and villages should be the aim, whereas biocontainment (containing the virus) should be the aim with markets.
Vaccination
Vaccination against AI is usually only used in order to help control an outbreak. A majority of the vaccines used are inactivated vaccines, though some are starting to use vectored vaccines. A reverse genetic engineered reassortant (rg) vaccine is also available. This vaccine has been updated twice due to changing field viruses.[7]
The duration of immunity from vaccination is largely unknown due to the logistical problems of studying this. Current studies vary from 12 weeks to 138 weeks with different vaccines. The effect of repeat dosing is also unclear, though dosing twice has shown an increase in immunity from 1 to 10 months.[7]
Within the commercial sector breeding birds and layers are usually the only birds vaccinated due to the high cost. Also, the addition of adjuvants (e.g. oil emulsion) requires a withdrawal time that is usually longer than the lifespan of a meat chicken thus meaning that, in most cases, it is economically unviable to vaccinate. Egypt has however vaccinated meat birds as part of a routine vaccination program. Hong Kong is the only place that has achieved national flock immunity.[7] In developing countries the vaccination rate within village poultry is too low to achieve population immunity, and proper vaccine storage is also a problem.
Suboptimal vaccination, and thus incomplete immunity, can lead to an increase in antigenic drift by increasing immune pressure exerted in hosts and can also increase the rate at which the virus is able to cross species. It could also lead to clinical symptoms being masked and thus increasing disease spread. Suboptimal immunity can occur through a number of ways: host immunosupression, vaccine spoilage, inadequate dosing, poor antigenic match between vaccine and virus, low vaccination uptake in the population or exposure to the virus before full immunity has developed.
AI vaccines are constantly being updated to cover for new strains of AI due to antigenic drift. Vaccines are currently being developed that target the M2 protein, which is conserved among different subtypes of virus. Subunit vaccines are being developed but the cost would inhibit use in poultry and there is a lack of data on whether it would provide protection in chickens.[7]
rNDV (recombinant Newcastle Disease virus) vaccines may offer a solution to the labour intensive administration of traditional vaccines in that they can be administered through drinking water. NDV vaccination is routine worldwide, and NDV replicates in the same tissues as AI therefore can confer better immunity at smaller doses than would otherwise be required. NDV will also replicate in chickens and turkeys. However, maternal antibodies to the vector will interfere with immunity. Fowl poxvirus vectored vaccines are licensed for use in the US and have been used in China and Mexico.[7]
HI tests can be used post vaccination to monitor the immune response, though HI tests used after vaccination in Egypt showed the antibodies produced by the vaccine to have no cross reactivity with field antigens. Serum from vaccinated birds from one strain found in Egypt showed no reaction with other H5 based antigens of vaccine strains found in Egypt, thus showing the importance of using the correct field antigens present when developing vaccines. Monoclonal antibody ELISA tests based on the H5N1 Asian strain did not detect the Egyptian variant either.[3]
Inactivated vaccinations have played an important role in H9 control in China, though AI still persists in chicken populations, even those that have been vaccinated, due to genetic variation. Vaccination of poultry can decrease disease and virus shedding if birds become infected, and can also lead to an increase in the amount of virus needed to infect vaccinated birds.
Within the countries that have endemic H5N1 Bangladesh and India are the only countries not to have vaccination programs, though Bangladesh is in the process of developing a program.[7]
A majority of the vaccine research being performed is related to human vaccines due to the public health risks associated with AI. DNA vaccines are currently being developed, though due to cost and the need for multiple doses to be individually administered it is unlikely they will be used in poultry.
The development of DIVA system (differentiating infected from vaccinated animals) is currently an important focus of research due to trade and political issues.
References
- ↑ Mahy, B.W.J., Meulen, V.T.(2007)Topley & Wilson’s Microbiology and Microbial Infections Virology Vol. 1. Amer. Soc. for Microbiology; 10th edition
- ↑ 2.0 2.1 Suarez, D.L. (2010), Avian influenza: our current understanding, Animal Health Research Reviews 11(1); 19–33
- ↑ 3.0 3.1 3.2 Abdelwhab, E.M., Hafez, H.M. (2011), An overview of the epidemic of highly pathogenic H5N1 avian influenza virus in Egypt: epidemiology and control challenges, Epidemiol. Infect. 139, 647–657.
- ↑ Zhang G, Shoham D, Gilichinsky D, Davydov S, Castello J.D., Rogers S.O. (2006), Evidence of influenza A virus RNA in Siberian lake ice. Journal of Virology 80: 12229–12235.
- ↑ Biosecurity for Highly Pathogenic Avian Influenza Issues and options (2008) FAO Animal Production and Health Paper No. 165
- ↑ Diaro, M.D., Elelu, N., (2013) Knowledge and preventive practices related to Avian influenza among livestock farmers and poultry traders in Ikorodu, Lagos state, Nigeria, Journal of Public Health and Epidemiology, Vol. 5(4), 202-207, April
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Spackman E., Swayne, D.E. (2013), Vaccination of gallinaceous poultry for H5N1 highly pathogenic avian influenza: Current questions and new technology, Virus Research, March 21st.
- ↑ Centers for Disease Control and Prevention: Morbidity and Mortality Weekly Report, Emergence of Avian Influenza A(H7N9) Virus Causing Severe Human Illness — China, February–April 2013, May 10, 2013 / 62(18);366-371
- ↑ 9.0 9.1 Koopmans, M., de Jong, M.D. (2013), Avian influenza A H7N9 in Zhejiang, China, The Lancet, 26th April 2013.
- ↑ Qun Li, M.D., Lei Zhou, M.D., Minghao Zhou, Ph.D., Zhiping Chen, M.D., Furong Li, M.D., Huanyu Wu, M.D., Nijuan Xiang, M.D., Enfu Chen, M.P.H., Fenyang Tang, M.D., Dayan Wang, M.D., Ling Meng, M.D., Zhiheng Hong, M.D., Wenxiao Tu, M.D., Yang Cao, M.D., Leilei Li, Ph.D., Fan Ding, M.D., Bo Liu, M.D., Mei Wang, M.D., Rongheng Xie, M.D., Rongbao Gao, M.D., Xiaodan Li, M.D., Tian Bai, M.D., Shumei Zou, M.D., Jun He, M.D., Jiayu Hu, M.D., Yangting Xu, M.D., Chengliang Chai, M.D., Shiwen Wang, M.D., Yongjun Gao, M.D., Lianmei Jin, M.D., Yanping Zhang, M.D., Huiming Luo, M.D., Hongjie Yu, M.D., M.P.H., Lidong Gao, M.D., Xinghuo Pang, M.D., Guohua Liu, M.D., Yuelong Shu, Ph.D., Weizhong Yang, M.D., Timothy M. Uyeki, M.D., M.P.H., M.P.P., Yu Wang, M.D., Fan Wu, M.D., and Zijian Feng, M.D., M.P.H. (2013)Preliminary Report: Epidemiology of the Avian Influenza A (H7N9) Outbreak in China, The New England Journal of Medicine, April 24th 2013
- ↑ Gonzales J.L., Stegeman, J.A., Koch, G., de Wit, S.J., Elbers, A.R.W.(2013), Rate of introduction of a low pathogenic avian influenza virus infection in different poultry production sectors in the Netherlands, Influenza and Other Respiratory Viruses Volume 7, Issue 1, pages 6–10, January 2013
- ↑ Alexander, D.J. (2000), A Review of avian influenza in different bird species, Veterinary Microbiology, Volume 74, Issues 1–2, 22 May 2000, Pages 3–13
- ↑ Hill N.J., Takekawa J.Y., Cardona C.J., Ackerman J.T., Schultz A.K., Spragens K.A. and Boyce W.M. (2010). Waterfowl ecology and avian influenza in California: do host traits inform us about viral occurrence?, Avian Diseases 54: 426–432.
- ↑ 14.0 14.1 14.2 Alexander, D.J.(2008) , Avian Influenza – Diagnosis, Zoonoses and Public Health Volume 55, Issue 1, pages 16–23, February 2008
OIE Avian Influenza accessed June 23, 2013
SH Lu, XH Xi, YF Zheng, Y Cao, XN Liu, HZ Lu (2013) Analysis of the clinical characteristics and treatment of two patients with avian influenza virus (H7N9). Bioscience trends, 2013 ;7(2):109-112.
DEFRA Avian Influenza accessed June 23, 2013
Fournié, G., Guitian, J., Desvaux, S., Cuong, V.C., Dung, D.H., Pfeiffer, D.U., Mangtani, P., Ghani, A.C.(2013), Interventions for avian influenza A (H5N1) risk management in live bird market networks, PNAS, May 6, 2013, doi: 10.1073/pnas.1220815110
Chen R.A., Lai H.Z., Li L., Liu Y.P., Pan W.L., Zhang W.Y., Xu J.H., He D.S., Tang Z.X.(2013), Genetic variation and phylogenetic analysis of hemagglutinin genes of H9 avian influenza viruses isolated in China during 2010-2012. Vet Microbiol. 2013 Apr 12
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
Error in widget FBRecommend: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt67240b61e0a620_91954971 Error in widget google+: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt67240b61f3fbd4_65184350 Error in widget TwitterTweet: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt67240b6213b868_76643363
|
| WikiVet® Introduction - Help WikiVet - Report a Problem |