Difference between revisions of "Labrador cross with mass on antebrachium"
| (10 intermediate revisions by the same user not shown) | |||
| Line 8: | Line 8: | ||
</big></b> | </big></b> | ||
<br><br> | <br><br> | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
<center><WikiQuiz | <center><WikiQuiz | ||
questionnumber="1" | questionnumber="1" | ||
| Line 165: | Line 147: | ||
</WikiQuiz></center> | </WikiQuiz></center> | ||
| − | <center><gallery widths=200px perrow= | + | <center><WikiQuiz |
| − | File:Case 19- | + | questionnumber="9" |
| − | File:Case 19- | + | question="Unfortunately radiation therapy is not available, and the clients refuse amputation. The specialist oncology surgeon plans the surgery to achieve the widest margins possible (deep and lateral), and then reconstructs the deficit with an axial pattern flap. What is an axial-pattern flap?" |
| − | File:Case 19- | + | choice1="A skin flap rotated around an axis in a specified pattern" |
| − | File:Case 19- | + | choice2="A skin flap containing a direct cutaneous artery and vein " |
| + | choice3="A skin flap, which is detached from the donor site and placed on the recipient site in an axial pattern " | ||
| + | choice4="A skin flap, which is tubed and after 2 weeks is then ‘caterpillared’ to cover the skin deficit " | ||
| + | choice5="" | ||
| + | correctchoice="2" | ||
| + | feedback1="'''Incorrect'''. You need a better understanding of possible surgical options. Review a general animal surgery text and choose again." | ||
| + | feedback2="Correct. This means the skin flap has a 50% greater chance of survival than a skin flap, which does not contain a direct cutaneous artery and vein." | ||
| + | feedback3="'''Incorrect'''. You need a better understanding of possible surgical options. Review a general animal surgery text and choose again." | ||
| + | feedback4="'''Incorrect'''. You need a better understanding of possible surgical options. Review a general animal surgery text and choose again." | ||
| + | feedback5="" | ||
| + | image= ""> | ||
| + | </WikiQuiz></center> | ||
| + | |||
| + | <center><WikiQuiz | ||
| + | questionnumber="10" | ||
| + | question="Which axial-pattern flap would be most appropriate to close this deficit (see photo)?" | ||
| + | choice1="Cranial superficial epigastric" | ||
| + | choice2="Caudal superficial epigastric " | ||
| + | choice3="Omocervical" | ||
| + | choice4="Thoracodorsal" | ||
| + | choice5="Superficial brachial " | ||
| + | correctchoice="4" | ||
| + | feedback1="'''Incorrect'''. You need a better understanding of possible surgical options. Review a general animal surgery text and choose again." | ||
| + | feedback2="'''Incorrect'''. You need a better understanding of possible surgical options. Review a general animal surgery text and choose again." | ||
| + | feedback3="'''Incorrect'''. You need a better understanding of possible surgical options. Review a general animal surgery text and choose again." | ||
| + | feedback4="'''Correct'''. This is the flap that would be expected to cover this deficit." | ||
| + | feedback5="'''Incorrect'''. You need a better understanding of possible surgical options. Review a general animal surgery text and choose again." | ||
| + | image= "File:Case 19-Q11-thoracodorsal draped in.JPG"> | ||
| + | </WikiQuiz></center> | ||
| + | |||
| + | <center><gallery widths=200px perrow=3> | ||
| + | File:Case 19-Q11-thoracodorsal prior to start.JPG | ||
| + | File:Case 19-Q11-thoracodorsal tumour out.JPG | ||
| + | File:Case 19-Q11-thoracodorsal elevated flap.JPG | ||
| + | File:Case 19-Q11-thoracodorsal end sx 2.JPG | ||
| + | File:Case 19-Q11-thoracodorsal end sx.JPG | ||
</gallery></center> | </gallery></center> | ||
<center><WikiQuiz | <center><WikiQuiz | ||
| − | questionnumber=" | + | questionnumber="11" |
| − | question="" | + | question="You resect the tumour and send tissue for histopathology. How do you prepare the resected tissue so that the pathologist is best equipped to give the information you need?" |
| − | choice1="" | + | choice1="Put the entire tumour in a 10:1 formalin:tumour ratio for 24 hours, then double-wrap the specimen and post it to the pathologist." |
| − | choice2="" | + | choice2="Ink selected lateral and deep margins with tissue-marking or India ink. Take a large wedge from the centre of the tumour, and discard the rest of the tissue. Fix these samples in 10:1 formalin:tumour for 24 hours, and then post to the pathologist in separately labelled pots." |
| − | choice3="" | + | choice3="Suture the underlying fascia to the skin on the lateral margins so that the tissue resembles the in situ tumour dimensions. Incise the tumour every few centimetres to allow the formalin to penetrate into the tumour mass: these incisions should be two-thirds through the depth of the tumour. Ink the lateral and deep margins with tissue-marking or India ink. Fix the tumour in 10:1 formalin:tumour for 24 hours, then double-wrap the specimen and post it to the pathologist." |
choice4="" | choice4="" | ||
choice5="" | choice5="" | ||
| − | correctchoice=" | + | correctchoice="3" |
| − | feedback1="" | + | feedback1="'''Incorrect'''. This is not the best option. Choose again." |
| − | feedback2="" | + | feedback2="'''Incorrect'''. This is not the best option. Choose again." |
| − | feedback3="" | + | feedback3="'''Correct'''." |
feedback4="" | feedback4="" | ||
feedback5="" | feedback5="" | ||
| + | image= ""> | ||
| + | </WikiQuiz></center> | ||
| + | |||
| + | <center><gallery widths=200px perrow=2> | ||
| + | File:Case 19-Q9-specimen skin surface.JPG|Skin surface | ||
| + | File:Case 19-Q9-specimen muscle surface.JPG|Muscle surface - note that the underlying deep fascia has been resected en bloc with the tumour) | ||
| + | File:Case 19-Q9-specimen inked.JPG|Specimen inkeed | ||
| + | File:Case 19-Q9-specimen sliced.JPG|specimen sliced | ||
| + | </gallery></center> | ||
| + | |||
| + | |||
| + | <center><WikiQuiz | ||
| + | questionnumber="12" | ||
| + | question="The margins are clear and the pathologist confirms your histological diagnosis of grade 2 STS: it is a haemangiopericytoma. What other tumours fit the STS category, characterized by similar biological behaviour? (Choose three of the following.) | ||
| + | choice1="Synovial cell sarcoma, Histocytic sarcoma, Brachial or lumbar plexus nerve root tumours" | ||
| + | choice2="Splenic haemangiosarcoma, Histocytic sarcoma, Malignant schwannomas" | ||
| + | choice3="Splenic haemangiosarcoma, Peripheral nerve sheath tumours, Brachial or lumbar plexus nerve root tumours" | ||
| + | choice4="Synovial cell sarcoma, Peripheral nerve sheath tumours, Fibrosarcoma" | ||
| + | choice5="Peripheral nerve sheath tumours, Malignant schwannomas, Fibrosarcoma" | ||
| + | correctchoice="5" | ||
| + | feedback1="'''Incorrect'''. One of more of the options selected are incorrect. Choose again." | ||
| + | feedback2="'''Incorrect'''. One of more of the options selected are incorrect. Choose again." | ||
| + | feedback3="'''Incorrect'''. One of more of the options selected are incorrect. Choose again." | ||
| + | feedback4="'''Incorrect'''. One of more of the options selected are incorrect. Choose again." | ||
| + | feedback5="'''Correct'''. Synovial cell sarcoma have a greater affinity for lymph node metastasis than subcutaneous STS. Splenic haemangiosarcoma are more systemically aggressive, with microscopic or macroscopic systemic metastasis expected in 90% of cases at diagnosis. Histocytic sarcoma have a much more aggressive, early metastatic pattern. Brachial or lumbar plexus nerve root tumours have a different pattern of local invasion, extend proximally and distally along nerve roots and can invade the spinal cord." | ||
image= ""> | image= ""> | ||
</WikiQuiz></center> | </WikiQuiz></center> | ||
<center><WikiQuiz | <center><WikiQuiz | ||
| − | questionnumber=" | + | questionnumber="13" |
| − | question="" | + | question="What next step do you propose?" |
| − | choice1="" | + | choice1="Adjuvant doxorubicin chemotherapy to reduce the chance of development of pulmonary metastatic disease, followed by frequent checks for local recurrence (every 3 months for a year) and repeat radiographs at 6 and 12 months postoperatively. " |
| − | choice2="" | + | choice2="Frequent checks for local recurrence (every 3 months for a year) and repeat radiographs at 6 and 12 months postoperatively. " |
| − | choice3="" | + | choice3="Long-term piroxicam chemotherapy as an antiangiogenic treatment to reduce the development of pulmonary metastatic disease, as well as frequent checks for local recurrence (every 3 months for a year) and repeat radiographs at 6 and 12 months postoperatively." |
| − | choice4="" | + | choice4="Adjuvant carboplatin chemotherapy to reduce the chance of development of pulmonary metastatic disease, followed by frequent checks for local recurrence (every 3 months for a year) and repeat radiographs at 6 and 12 months postoperatively." |
choice5="" | choice5="" | ||
| − | correctchoice=" | + | correctchoice="2" |
| − | feedback1="" | + | feedback1="'''Incorrect'''. Adjuvant chemotherapy for grade 2 STS is not indicated, as there is no proven benefit, nor is it proven to be of benefit for grade 3 STS in dogs. Chemotherapy may have some value for highly anaplastic sarcomas, where immunohistochemistry is required to determine histiogenesis; however, even this is unproven. Choose again." |
| − | feedback2="" | + | feedback2="'''Correct'''. Adjuvant chemotherapy is of no benefit for grade 2 STS, so should not be offered." |
| − | feedback3="" | + | feedback3="'''Incorrect'''. Adjuvant chemotherapy for grade 2 STS is not indicated, and is likely to be of little benefit for grade 3 STS. It may have some value for highly anaplastic sarcomas, where immunohistochemistry is required to determine histiogenesis; however, even this is unproven. The chemotherapeutic agent with the most expected benefit is doxorubicin or similar, so this would be inappropriate therapy. Choose again." |
| − | feedback4="" | + | feedback4="'''Incorrect'''. Adjuvant chemotherapy for grade 2 STS is not indicated, and is likely to be of little benefit for grade 3 STS. It may have some value for highly anaplastic sarcomas, where immunohistochemistry is required to determine histiogenesis; however, even this is unproven. The chemotherapeutic agent with the most expected benefit is doxorubicin or similar, so this would be inappropriate therapy. Choose again." |
feedback5="" | feedback5="" | ||
image= ""> | image= ""> | ||
| Line 207: | Line 249: | ||
<center><WikiQuiz | <center><WikiQuiz | ||
| − | questionnumber=" | + | questionnumber="14" |
| − | question="" | + | question="You recheck your patient frequently and after 12 months there is evidence of a 5 × 3-cm wide, fixed soft-tissue swelling along one area of the surgical suture line at the proximal lateral antebrachium and overlying the ventrolateral chest wall. You biopsy this swelling as a small wedge biopsy and this confirms local recurrence of tumour, this time as a grade 3 STS. You had warned the clients that amputation was your preferred treatment option due to the difficulty in attaining margins because of tumour size and location, and so they are disappointed but not unprepared. It was also explained to them that recurrent disease has a poorer prognosis than optimally treated first-time, curative intent surgery. What would you do next?" |
| − | choice1="" | + | choice1="Thoracic radiographs + abdominal ultrasound (as now grade 3) before amputation if staging is negative." |
| − | choice2="" | + | choice2="Thoracic radiographs + abdominal ultrasound (as now grade 3) + contrast-enhanced advanced imaging (e.g. CT, magnetic resonance imaging (MRI)) of local disease to ensure recurrent disease is resectable before wide surgical resection (most likely amputation)." |
| − | choice3="" | + | choice3="Thoracic radiographs + abdominal ultrasound (as now grade 3) + contrast-enhanced advanced imaging (e.g. CT, MRI) of local disease followed by marginal resection of local recurrence and adjuvant radiation therapy." |
choice4="" | choice4="" | ||
choice5="" | choice5="" | ||
| − | correctchoice=" | + | correctchoice="2" |
| − | feedback1="" | + | feedback1="'''Incorrect'''. It is best to have advanced imaging of local tumour before surgery, as this may help you plan your surgery. Choose again." |
| − | feedback2="" | + | feedback2="'''Correct'''." |
| − | feedback3="" | + | feedback3="'''Incorrect''', because you are irradiating over the chest wall and may incur long-term complications of fibrosis of irradiated lung. Therefore this is not your preferred option, as long as the dog has no intercurrent orthopaedic or neurological disease which precludes amputation. Choose again." |
feedback4="" | feedback4="" | ||
feedback5="" | feedback5="" | ||
| Line 224: | Line 266: | ||
<center><WikiQuiz | <center><WikiQuiz | ||
| − | questionnumber=" | + | questionnumber="15" |
| − | question="" | + | question="Luckily, your thoracic radiographs are negative for pulmonary metastatic disease, and there is still no palpably enlarged regional lymph node. You have optimized this patient’s outcome by ensuring frequent rechecks. However, you need to treat the primary tumour. What is the commonest cause of death for dogs with subcutaneous STS?" |
| − | choice1="" | + | choice1="Metastatic disease" |
| − | choice2="" | + | choice2="Uncontrolled or inadequately treated local disease" |
choice3="" | choice3="" | ||
choice4="" | choice4="" | ||
choice5="" | choice5="" | ||
| − | correctchoice=" | + | correctchoice="2" |
| − | feedback1="" | + | feedback1="'''Incorrect'''. Review STS before retrying.]]>" |
| − | feedback2="" | + | feedback2="Correct." |
feedback3="" | feedback3="" | ||
feedback4="" | feedback4="" | ||
| Line 241: | Line 283: | ||
<center><WikiQuiz | <center><WikiQuiz | ||
| − | questionnumber=" | + | questionnumber="16" |
| − | question="" | + | question="The clients are prepared for amputation, which your advanced imaging shows is most appropriate, as you will not be able to attain wide margins without it. You perform the amputation and succeed in attaining 3-cm margins around gross tumour, confirmed by the pathologist. You continue your frequent rechecks. Unfortunately, after 6 months there is evidence of two nodules in the caudal lung fields.Now it is optimal for you offer the clients doxorubicin chemotherapy. True or false?" |
| − | choice1="" | + | choice1="True" |
| − | choice2="" | + | choice2="False" |
choice3="" | choice3="" | ||
choice4="" | choice4="" | ||
choice5="" | choice5="" | ||
| − | correctchoice=" | + | correctchoice="2" |
| − | feedback1="" | + | feedback1="'''Incorrect'''. This treatment is of no proven benefit." |
| − | feedback2="" | + | feedback2="'''Correct'''. There is no proven benefit of giving adjuvant doxorubicin in this setting. You have done all you can do for this dog. It is a shame that the clients would not agree to amputation initially, as a surgical cure was likely at the first adequate surgical attempt at resection with wide clean margins. A marginal excision and adjuvant radiation therapy would have also given a good prognosis.]" |
feedback3="" | feedback3="" | ||
feedback4="" | feedback4="" | ||
| Line 256: | Line 298: | ||
image= ""> | image= ""> | ||
</WikiQuiz></center> | </WikiQuiz></center> | ||
| + | <br><br> | ||
| + | {{Elsevier | ||
| + | |url = http://www.elsevierhealth.co.uk/product.jsp?isbn=9780702042508 | ||
| + | |book = North and Banks, Small Animal Oncology | ||
| + | |image = North and Banks SA Oncology.jpg | ||
| + | }} | ||
| + | |||
| + | [[Category:Case-based Quizzes]] | ||
Latest revision as of 18:09, 4 October 2012
Signalment:
- 7-year-old male neutered Labrador cross
Presenting sign:
- 7 x 5 cm firm mobile mass on the caudal aspect of the proximal antebrachium, which has grown over the past three months. Otherwise clinically well, with no evidence of lameness and no other history of illness. Physical exam is otherwise within normal limits.
1 |
What would be your next step? |
| Histopathology report |
|---|
| Gross pathology One pot is submitted:biopsy of the leg. A pece of pale tan resilient tissue measuring 7 x 5 x 5 mm. A representative section is placed in Cassette A. Histopathology This is a section of a tumour composed of sheets of neoplastic pleomorphic polyhedral to spindle cells with a mitotic index approximating 1-2 mitoses per high power field. They are accompanied by minimal collagen. The neoplastic cells have mild karyomegaly and nucleolar prominence together with abundant eosinophilic, vacuolated cytoplasm. Diagnosis Cutaneous soft-tissue sarcoma, grade 2. Comments This diagnosis is in keeping with the previous cytological findings. The minimal collagen and cytoplasmic vacuolation evident in this case raises the possibility of liposarcoma as a more specific diagnosis. In any case, this tumour is likely to be characterized by infiltrative local growth but negligible tendency for metastatic spread. |
2 |
Review the histopathology report. What do you understand about the behaviour of soft-tissue sarcomas (STS)? |
3 |
What is the metastatic rate of grade 2 STS? |
4 |
What is the metastatic rate of grade 1 STS? |
5 |
What is the metastatic rate of grade 3 STS? |
6 |
What would you choose to do next? |
7 |
You now know that the regional lymph node is not palpable, and the thoracic radiographs are unremarkable. You have adequately staged this tumour to stage I (primary site only). What can be expected with adequate treatment of this tumour? |
8 |
Haematology, biochemistry and urinalysis before surgery are within normal limits. What is your preferred option for treatment of the local tumour? |
9 |
Unfortunately radiation therapy is not available, and the clients refuse amputation. The specialist oncology surgeon plans the surgery to achieve the widest margins possible (deep and lateral), and then reconstructs the deficit with an axial pattern flap. What is an axial-pattern flap? |
10 |
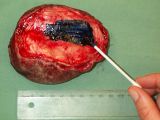
Which axial-pattern flap would be most appropriate to close this deficit (see photo)? |
11 |
You resect the tumour and send tissue for histopathology. How do you prepare the resected tissue so that the pathologist is best equipped to give the information you need? |
12 |
The margins are clear and the pathologist confirms your histological diagnosis of grade 2 STS: it is a haemangiopericytoma. What other tumours fit the STS category, characterized by similar biological behaviour? (Choose three of the following.) choice1= |
13 |
What next step do you propose? |
14 |
You recheck your patient frequently and after 12 months there is evidence of a 5 × 3-cm wide, fixed soft-tissue swelling along one area of the surgical suture line at the proximal lateral antebrachium and overlying the ventrolateral chest wall. You biopsy this swelling as a small wedge biopsy and this confirms local recurrence of tumour, this time as a grade 3 STS. You had warned the clients that amputation was your preferred treatment option due to the difficulty in attaining margins because of tumour size and location, and so they are disappointed but not unprepared. It was also explained to them that recurrent disease has a poorer prognosis than optimally treated first-time, curative intent surgery. What would you do next? |
15 |
Luckily, your thoracic radiographs are negative for pulmonary metastatic disease, and there is still no palpably enlarged regional lymph node. You have optimized this patient’s outcome by ensuring frequent rechecks. However, you need to treat the primary tumour. What is the commonest cause of death for dogs with subcutaneous STS? |
16 |
The clients are prepared for amputation, which your advanced imaging shows is most appropriate, as you will not be able to attain wide margins without it. You perform the amputation and succeed in attaining 3-cm margins around gross tumour, confirmed by the pathologist. You continue your frequent rechecks. Unfortunately, after 6 months there is evidence of two nodules in the caudal lung fields.Now it is optimal for you offer the clients doxorubicin chemotherapy. True or false? |
| This resource was adapted from North and Banks, Small Animal Oncology provided by Elsevier Health Sciences as part of the PublishOER Project. | 
|