Difference between revisions of "Pharmacodynamics"
Phlancelot (talk | contribs) |
Phlancelot (talk | contribs) |
||
| Line 45: | Line 45: | ||
'''Please Insert Appropriate Graphs''' | '''Please Insert Appropriate Graphs''' | ||
| + | [[File:Dose-Response Curve.png|thumb|Add caption here]] | ||
From these graphs two figures can be achieved, the '''ED50''' or '''EC50'''. The ED50 is the effective dose at which 50% of a maximal response occurs or 50% of individuals respond. The EC50 is the same but is the effective concentration. Agonists with higher affinities will have a lower concentration and so EC50 than an agonist with a lower affinity. The first drug is therfore said to be more '''potent'''. | From these graphs two figures can be achieved, the '''ED50''' or '''EC50'''. The ED50 is the effective dose at which 50% of a maximal response occurs or 50% of individuals respond. The EC50 is the same but is the effective concentration. Agonists with higher affinities will have a lower concentration and so EC50 than an agonist with a lower affinity. The first drug is therfore said to be more '''potent'''. | ||
Revision as of 13:26, 4 May 2012
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
|
|
Pharmacodynamics is the actions of drugs on the body.
For drugs to act upon the body they must be able to exert some chemical influence upon a cell to result in a physiological response. They are capable of doing this by binding to a target molecule (usually proteins).
There are four main targets which drugs to bind to:
- Receptors - these are protein molecules that are capable of responding to endogenous chemical signals. They are usually found on the cell membrane, in the cytoplasm or on the nucleus and other organelles.
- Enzymes - both intracellular and extracellular ones.
- Ion Channels
- Transport proteins
Agonists
An agonist can be defined as a drug that binds to a target molecule and results in activation of the receptor and thus a tissue response.
- An agonist forms a complex with the receptor. This complex is dynamic as the agonist will continously associate and dissociate with the receptor. The agonist will continue to do this and thus produce a response, until the concentration of the agonist is reduced to a level at which binding no longer occurs.
- The rate of complex formation is dependent on two factors: agonist concentration and the number of free receptors.
- The affinity of a drug to a receptor varies and can be compared using the equilibrium constant or KA.
This can be defined as the concentration of a drug which results in 50% of receptors being bound in equilibrium or when K1=K-1.
Drug + Number of Free Receptors = Drug-Receptor Complexes Where K1 is the rate constant in a forward direction (association rate constant) and K-1 is the rate constant in a backward direction (dissociation rate constant)
Therefore a drug that has a higher affinity to a receptor has a lower KA value.
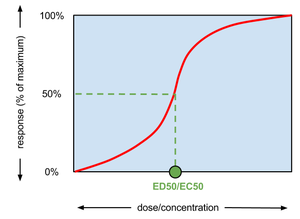
- The biological response resulting from an agonist binding is proportional to the number of receptors occupied. The size of a response can be measured and plotted against the dose/concentration of the agonist. As the size of a response normally increases in a non-linear manner (until the maximum is reached) the response is normally plotted against the log of the concentration.
Please Insert Appropriate Graphs
From these graphs two figures can be achieved, the ED50 or EC50. The ED50 is the effective dose at which 50% of a maximal response occurs or 50% of individuals respond. The EC50 is the same but is the effective concentration. Agonists with higher affinities will have a lower concentration and so EC50 than an agonist with a lower affinity. The first drug is therfore said to be more potent.
The potency of a drug is very important clinically as it will determine the dose needed to have the desired clinical effect. Often if a drug is more potent it is usally more selective to which target molecules it binds to.
Full and Partial Agonists
- A full agonist is defined as an agonist that is capable of producing the maximal response of a tissue. To achieve this the number of receptors occupied varies and in some cases very few receptors need occupying. This is called the spare receptor hypothesis and is very relevant when thinking about multiple drugs working at the same receptor site simultaneously.
- A partial agonist is unable to produce the maximum tissue response however great the dose or concentration of the drug. It must be remembered that a partial agonistmay have a greater, lesser or equal affinity to a receptor site compared to a full agonist.
The difference between the full and partial agonist is it's efficacy. This is defined as the strength of the tissue response that results from the formation of a agonist-receptor complex. The efficacy of the partial agonist is lower than that of the full agonist.
It is still unclear why molecules that are chemically very similar have differing efficacies. Only now are the mechanisms behind it being gradually understand. This however doesn't mean that we ignore efficacy. It is of great practical importance as some drugs of equal affinity for a specific receptor may have widely differing efficacy.
Inverse Agonists
These are agonists that bind to receptors that are continuely activated (even if no ligand is present) and result in the reduction of the level of activation. They therefore have a negative efficacy.
Effector Linkage Mechanisms
Once the agonist binds to the receptor the cell response can be formed in three different ways:
- By the opening of a ligand gated ion channel
- By an intracellular second messenger system
- By DNA transcription
Antagonists
An antagonist can be defined as a drug that inhibits the action of an agonist.
Antagonists bind to similar receptors as agonist but crucially they don't activate any intracellular events and so there is no tissue response. It's effect is produced by reducing the amount or capability of an agonist to bind to it's target molecule.
Antagonists like agonists bind to receptors in a dynamic fashion, and so it is the antagonists affinity to the receptor that determines it's inhibitory response. The amount of inhibition thus depends on the concentration of the drug at the target site and the number of free receptor sites.
Competitive Antagonism
Reversible Competitive Antagonism
Here the antagonist competes with the agonist for the occupation of the receptor site. Since less agonist is able to bind to the target molecule the size of the tissue response will decrease. As the dose/concentration of the antagonist increases so the size of the tissue response will further decrease.
The formation of receptor complexes is dynamic in it's nature and so if the agonist' dose/concentration is increased it will out-compete the antagonist for receptor occupation and the size of the tissue response will start to increase. Therefore the antagonists action is reversible.
Irreversible Competitive Antagonism
This form of antagonism essentially works in the same manner as above except for one crucial difference. The antagonist forms very strong bonds to the receptor sit meaning that it dissociates very slowly or not at all. This means that increasing the amount of agonist present is unable to out-compete the antagonist as receptor sites are always full.
A partial agonist can effectively act as an antagonist when it is present in very high concentrations as it out-competes the full agonist for the receptor site.
Non-Competitive Antagonism
Here the agonist binds to its receptor but the antagonist acts further along the sequence of events resulting in a tissue response. As this chain is blocked the agonist is incapable of producing a response.
Pharmacokinetic Antagonism
The antagonist reduces the effect of another drug by reducing its absorption or increasing its rate of metabolism or increasing its rate of excretion.
Self-antagonism
If some drugs are repeatedly given its effect can decrease. This is called tachyphylaxis or desensitisation. If a gradual decrease in response to a drug occurs this is called tolerance and if the drug loses total therapeutic efficacy it is deemed refractory. Many types of mechanisms occur to cause this phenomenon, the most important include:
- change in receptor type
- loss of receptors
- exhaustion of cell mediators
- increased metabolic degradation of the drug
- physiological adaptation
- active extrusion of the drug from cells
Chemical Antagonism
This is where the interaction of two drugs results in the failure of an biological activity.
Physiological Antagonism
This occurs when two drugs have opposing actions on the body and so their actions cancel each other out.