Difference between revisions of "Muscles Degenerative - Pathology"
Jump to navigation
Jump to search
m |
m |
||
| Line 188: | Line 188: | ||
**Later becoming calcified necrotic areas | **Later becoming calcified necrotic areas | ||
***More obvious | ***More obvious | ||
| − | **Pigs also have lesions in their [[Myocardial - Pathology#Hyaline degeneration|heart]] and [[Liver - | + | **Pigs also have lesions in their [[Myocardial - Pathology#Hyaline degeneration|heart]] and [[Liver General Pathology - Pathology#Hepatosis dietica|liver]] |
*Histologically: | *Histologically: | ||
**[[Muscles Degenerative - Pathology#Necrosis|Segmental necrosis]] +/- [[Muscles Degenerative - Pathology#Calcification|calcification]] and [[Muscles - normal#Regeneration|regeneration]] | **[[Muscles Degenerative - Pathology#Necrosis|Segmental necrosis]] +/- [[Muscles Degenerative - Pathology#Calcification|calcification]] and [[Muscles - normal#Regeneration|regeneration]] | ||
Revision as of 12:18, 21 August 2008
|
|
Degeneration
- Different types of degeneration
- May, or may not, be reversible
- Cloudy swelling, hydropic, vacuolar, granular and fatty change
- Occur following many different types of insult and are usually segmental
- If regeneration does not occur after formation of small vacuoles, necrosis follows
- Vacuolation -> floccular degeneration -> granular degeneration -> hyaline and Zenker’s degeneration
- Vacuolar degeneration:
- Due to swelling of organelles or due to glycogen or fat accumulation
- May be caused by hypokalaemia, hyperkalaemia or necrosis
- Histologically:
- Swollen
- Hypereosinophilic
- Lost cross striations
Calcification
- Due to:
- Old age - myofibres
- Following necrosis - dystrophic calcification
- May be visible grossly as white foci
Ossification
- Metaplasia of muscle to bone
- Localised
- Only in single muscle or a single group of muscles
- May be associated with trauma
- Seen in horses and dogs
- Histologically:
- Central zone - proliferating undifferentiated cells and fibroblasts
- Middle zone - osteoblasts depositing osteoid and bone
- Outer zone - trabecular bone remodelled by osteoclasts
- Progressive (fibrodysplasia ossificans progressiva)
- In connective tissue associated with skeletal muscle
- Secondary involvement of muscle tissue
- In pigs and cats
- Histologically:
- Bundles of dense fibrous connective tissue
- May contain accumulations of cartilage, bone or calcium
- Hyperplastic connective tissue -> compression of adjacent skeletal muscle -> atrophy
Pigmentation
- Lipofuscin
- Wear and tear pigment accumulating in secondary lisosomes -> converted into compact residual bodies
- Due to old age, past or recent cachexia or starvation
- Mostly stored in skeletal muscle of old high producing dairy cattle
- Masseters and diaphragm mainly involved
- No clinical importance
- Histologically:
- Rounded yellow to brown granules at both poles of nucleus of the skeletal myofiber
- Melanin
- As part of congenital melanosis of calves in fascial sheaths and epimysium
- Grossly - black foci
- Myoglobin
- After extensive muscle necrosis - rhabdomyolysis
- Leaks to adjacent tissue after sudden injury
- May also be present after some types of intramuscular injections e.g. iron dextran or tetracycline
Necrosis
- Necrosis of an entire myofibre is uncommon
- Segmental necrosis is more typical
- Muscle cell contents may leak into the blood if the cell membrane is damaged
- Creatine kinase (CK) is an enzyme which leaks following injury
- Used to measure the extent of muscle damage
- Often is followed by regeneration
- Histologically:
- Hyaline hypercontracted fiber rounded at cross-section and increased diameter and eosin staining
- May also be an artifact due to hypercontraction of normal fibres at fixation
- Fragmenting portions of fibre -> floccular or granular
- Normal portion of fibre may detach from necrotic part -> retraction caps
- Infarction may cause discoid degeneration - necrotic fibres detach at Z lines
- May mineralise
- Hyaline hypercontracted fiber rounded at cross-section and increased diameter and eosin staining
- Zenker's degeneration - secondary to systemic disease
- Scattered small segments of necrosis and fast regeneration
- Sacrolemmal tubes are intact
Atrophy
- Decreased myofibre or whole muscle diameter
- Myofibrils removed by disintegration -> sacrolemma too large -> forms folds
- Caused by:
- Disuse (e.g. fracture, failure to use limb, recumbency)
- Slower than denervation atrophy
- Reversible unless too prolonger or severe to cause loss of myofibres
- Denervation
- Any interference or damage to its nerve supply results in muscle atrophy
- Can be rapid - over 50% of muscle mass may be lost in a few weeks e.g. roarer horses with laryngeal hemiplegia
- May be reversible if innervation re-established
- Histologically:
- Fibres become rounded in cross section unless compressed by normal fibres
- Increased concentration of nuclei as they take much longer to disintegrate
- Fibrous stroma of epimysium and endomysium condenses -> more prominent
- End result in muscle consisting of almost only fibrous tissue
- Sometimes replaced by fat tissue -> increased size of muscle = pseudohypertrophy
- Muscle may have a mixture of atrophied and hypertrophied (due to increased work load) fibres if some motor units are not damaged
- Any interference or damage to its nerve supply results in muscle atrophy
- Metabolisation of muscle protein for nutrients during:
- Malnutrition, cachexia, senility
- Gradual onset except for some febrile diseases causing cachexia
- Postural muscles are not affected, sometimes even hypertrophy
- Histologically:
- Some nuclei disappear as myofibre volume is decreased
- Grossly:
- Smaller, darker, thinner muscles
- Disuse (e.g. fracture, failure to use limb, recumbency)
Toxic myopathy
- Plants
- E.g. Cassia occidentalis (coffee senna), Karwinskia humboldtiana (coyotillo), Eupatorium rugosum (white snakeroot), cotton seed
- Lesion an skeletal and cardiac muscle
- Grossly:
- Pale areas with ill-defined borders
- May involve very extensive necrosis
- Histologically:
- Segmental necrosis, no calcification
- Regeneration may occur in surviving animals
- Drugs
- E.g. corticosteroids, cholinesterase inhibitors, vincristine, dimethyl sulfoxide (DMSO)
- Monensin is a coccidiostat toxic to horses, donkeys, zebras, cattle, sheep, dogs and birds
- Causes muscle necrosis in heart and skeletal muscle
- Grossly:
- Pale streaks, mostly in hind limbs
- Histologically:
- Segmental necrosis
- Possibly regeneration in surviving animals
- Can cause rapid onset recumbency and potentially death
- Usually due to mixing errors in feed
- Also from intramuscular injections, e.g. oxytetracycline, lidocaine, chloramphenicol, produce local necrosis
- As satellite cells are destroyes, repair is via fibrosis with some budding
- Chemicals
- Iron injections can cause local myonecrosis
- Mycotoxins
- Metabolites cause persistent tremors
- Lesions in skeletal muscle only, possibly secondary to sustained contractions (similar to exertional myopathy)
- Histologically:
- Tiny foci of segmental necrosis
Endocrine myopathy
- Hyperadrenocorticism
- Muscle weakness is a clinical sign
- -> muscle atrophy
- Type II myofibre atrophy is non-specific
- Type IIB myofibre atrophy is preferential in hyperadrenocorticism
- Hypothyroidism can cause muscle atrophy
Nutritional myopathy
- Very important economic disease of sheep, cattle and pig
- Caused by:
- Deficiency of selenium, vitamin E or both
- Exacerbated by rapid growth, unaccustomed exercise or other dietary factor
- Pathogenesis:
- Oxygen free radicals (OFR) can damage cell membranes
- Vitamin E usually mops up OFRs
- Selenium as part of glutathione peroxidase neutralises effects of OFRs
- If Vit E or Se are deficient -> the balance shifts to membrane damage, calcium entry and mitochondrial damage -> cell swells and dies -> segmental muscle necrosis
- Grossly:
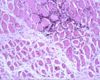
- Histologically:
- Segmental necrosis +/- calcification and regeneration
- Multifocal and multiphasic lesions
Exertional myopathies
- Caused by intensive and exhaustive activity of major muscle masses
- Glycogen used up -> local heat and lactic acid -> muscle degeneration
- Other forms include capture myopathy, racing greyhounds, sheep chased by dogs
Equine rhabdomyolysis
- Azoturia (Monday morning disease)
- Acute
- Due to exercise following a prolonged period of rest
- Clincal signs:
- Unable to move
- Sweating
- Tremors
- Swollen and hard lumbar, gluteal and femoral muscles
- Myoglobin leaks from muscle cells -> leaks into urine -> urine is dark red/brown (myoglobinuria) -> damages renal tubules
- Grossly:
- Salmon pink muscles -> dark, moist, swollen +/- pale streaks
- Histologically:
- Segmental myofibre necrosis
- Multifocal and monophasic, but may be multiphasic if repeated bouts
- Both, type IIA and IIB fibres affected; type IIB preferentially affected in acute disease
- Minor inflammatory reaction and calcification
- Segmental myofibre necrosis
- Tying-up
- Similar to azoturia but much milder
- Grossly - normal muscle
- Histologically - same as azoturia
Porcine stress syndrome
- =Malignant hyperthermia
- Pigs, dogs, humans
- Possibly a cellular defect resulting in high intacellular calcium ion concentration
- -> Activates myofibrillar ATPase -> rapid intracellular glycolysis -> increase in body heat -> denature protein -> cell death -> leakage of cellular content -> oedema
- Grossly:
- Muscles are pale, soft and exudative
- Histologically:
- Segmental hypercontraction
- Monophasic, multifocal segmental necrosis
- Inherited
- Triggered by halothane anaesthesia, stress of handling, transportation or slaughter
Neuromuscular junction diseases
Aquired myasthenia gravis
- See congenital MG
Botulism
- Caused by:
- Ingestion of Clostridium botulinum toxin which inhibits acetyl choline release
- Diagnosis by demonstration of toxin in faeces, ingested material or serum
Circulatory disturbances
Congestion
- Localised or generalised stasis -> dark red muscle
- E.g. in ruminal tympany (bloat) - congestion of muscles cranial to thoracic inlet
- May resemble haemorhage grossly
Ischaemia
- Firstly segmental necrosis
- -> death of satellite cells
- Causes regeneration but myoblast precursors have to be recruited from viable fibres
- -> death of all cells
- Mostly healed by fibrosis and scar formation
- May attempt regeneration by budding
Main causes:
- Vascular occlusion
- Infarction from embolism is rare due to collateral circulation
- Extension of infarcts depends on size of vessels occluded
- Small capillaries -> segmental necrosis
- Large arteries -> whole muscle areas, including sattelite cells, are killed
- Healed by fibrosis
- May be due to:
- Blockage of iliac arteries by aortic-iliac thrombosis in horses
- Blockage of aortic bifurcation in cats
- Dirofilaria immitis arteritis in dogs
- Vasculitis due to bluetongue virus in sheep
- Equine purpura haemorrhagica
- Non-contagious, sporadic
- Grossly:
- Subcutaneous oedema
- Scattered haemorrhagic foci throughout skin and muscles
- Vasculitis -> infarcts of muscles
- May cause myoglobinuria if extensive
- Possibly immune mediated
- In horses post streptococal infection, especially strangles
- External pressure
- During prolonged recumbency, e.g. anaesthesia, inability to rise, or due to too tightly fitting bandages or casts
- Post anaesthesia myopathy especially in horses
- Dorsal recumbancy -> gluteals and longissimus ischaemia
- Lateral recumbancy -> triceps brachii, pectoralis, deltoideus and brachiocephalicus ischaemia
- Caused by pressure on muscle > perfusion pressure of capillaries
- Downer cows - vetral recumbency -> ischaemia of pectoral muscles and muscles of limbs tucked under the animal
- Pregnant ewes with twins or triplets -> internal abdominal oblique muscle ischaemic necrosis -> potential rupture
- Muscle swelling where it cannot expand
- E.g. supracoracoid muscle infarction in some breeds of turkeys after flapping their wings
- Surrounded by inelastic fascial sheath and bone
- E.g. supracoracoid muscle infarction in some breeds of turkeys after flapping their wings
Trauma
- Due to:
- Direct transection of myofibres
- Compression of myofibres
- Secondary from haemorrhage (bruising)
- Partial rupture - e.g. of diaphragm in road traffic accident
- Complete rupture - e.g. quadriceps of racing greyhounds
- Myorrhexis (tearing) - e.g. slippery floor causing 'splits' in cattle -> adductor muscle tear
- Healing is by regeneration
- Fibrosis (scarring) will compromise function
- During fractures, fragments may cause further trauma if moved