Difference between revisions of "Sporothrix schenckii"
Jump to navigation
Jump to search
| Line 1: | Line 1: | ||
| − | + | ||
| − | * | + | |
| − | * | + | |
| − | * | + | [[Image:Sporotrichosis horse.jpg|thumb|right|150px|Sporotrichosis in a horse -Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] |
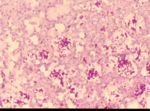
| − | ** | + | [[Image:Sporotrichosis cigar cells.jpg|thumb|right|150px|Sporotrichosis cigar shaped cells -Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] |
| − | ** | + | *''Sporothrix schenckii'' |
| − | * | + | |
| − | ** | + | *Occurs in soil, wood and vegetation |
| − | ** | + | **Saprophyte of both decaying and healthy vegetation |
| − | * | + | |
| + | *Worldwide | ||
| + | |||
| + | *Exogenous infections through wounds | ||
| + | |||
| + | *Sporadic infections | ||
| + | |||
| + | *Non-contageous | ||
| + | |||
| + | *Causes subcutaneous nodules or granulomas | ||
| + | **Nodules ulcerate discharging pus | ||
| + | |||
| + | *Spread via the [[Lymphatic System - Anatomy & Physiology|lymphatics]] | ||
| + | |||
| + | *The [[Bones and Cartilage - Anatomy & Physiology|bones]] and viscera can be involved which terminates in mortality | ||
| + | **This is rare | ||
| + | **Reported in dogs and horses | ||
| + | |||
| + | *Affects dogs, horses, cats, monkeys, mules, camels, donkeys, cattle, fowl and rodents | ||
| + | **Most commonly seen in horses as an ascending lymphocutaneous infection of the legs | ||
| + | **Can be confused with [[Subcutaneous Mycoses#Epizootic Lymphangitis|epizootic lymphangitis]] in horses | ||
| + | |||
| + | *Single cell, cigar shaped | ||
| + | **Usually found within [[Neutrophils|neutrophils]] | ||
| + | **Yeast cell clusters with peripheral eosinophilic rays can be seen in tissue sections | ||
| + | |||
| + | *Stained using PAS, Gram stain (positive), fluorescent antibody and Calcofluor White | ||
| + | |||
| + | *Latex agglutination and immunodiffusion serology can be performed | ||
| + | |||
| + | *Grows on Blood agar and Sabouraud's Dextrose agar in one to three weeks | ||
| + | **At 37°C: | ||
| + | ***Colonies are smooth, cream to tan coloured and soft | ||
| + | ***No mycelium can be seen | ||
| + | **At 25°C to 27°C: | ||
| + | ***Colonies turn from white and soft to tan to brown to black | ||
| + | ***Leathery, wrinkled and coarse | ||
| + | ***Mycelium can be seen as branching septate hyphae | ||
| + | ***Conidiospores can also be seen | ||
| + | |||
| + | *Potassium iodide treatment orally | ||
| + | **[[Antifungal Drugs#Flucytosine|5-fluorocytosine]] and [[Antifungal Drugs#Polyene Antifungals|amphotericin B]] can also be used[[Category:Subcutaneous_Mycoses]] | ||
| + | [[Category:To_Do_-_Fungi]] | ||
Revision as of 11:33, 30 June 2010
- Sporothrix schenckii
- Occurs in soil, wood and vegetation
- Saprophyte of both decaying and healthy vegetation
- Worldwide
- Exogenous infections through wounds
- Sporadic infections
- Non-contageous
- Causes subcutaneous nodules or granulomas
- Nodules ulcerate discharging pus
- Spread via the lymphatics
- The bones and viscera can be involved which terminates in mortality
- This is rare
- Reported in dogs and horses
- Affects dogs, horses, cats, monkeys, mules, camels, donkeys, cattle, fowl and rodents
- Most commonly seen in horses as an ascending lymphocutaneous infection of the legs
- Can be confused with epizootic lymphangitis in horses
- Single cell, cigar shaped
- Usually found within neutrophils
- Yeast cell clusters with peripheral eosinophilic rays can be seen in tissue sections
- Stained using PAS, Gram stain (positive), fluorescent antibody and Calcofluor White
- Latex agglutination and immunodiffusion serology can be performed
- Grows on Blood agar and Sabouraud's Dextrose agar in one to three weeks
- At 37°C:
- Colonies are smooth, cream to tan coloured and soft
- No mycelium can be seen
- At 25°C to 27°C:
- Colonies turn from white and soft to tan to brown to black
- Leathery, wrinkled and coarse
- Mycelium can be seen as branching septate hyphae
- Conidiospores can also be seen
- At 37°C:
- Potassium iodide treatment orally
- 5-fluorocytosine and amphotericin B can also be used