Description
A chronic disease caused by Mycobacterium bovis
Signalment
Diagnosis
Clinical Signs
Laboratory Tests
Radiography
Pathology
Treatment
Prognosis
References
- Reside primarily within macrophages where they multiply and result in characteristic granulomatous inflammation (macrophages and giant cells, epithelioid cells)
- Cattle can be infected by inhalation of the organism or through milk
- The primary complex
- Describes the initial focus of infection at the portal of entry (lungs) plus involvement of regional lymph nodes
- 90% of cases exhibit the pulmonary form
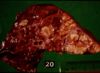
- Grossly:
- Small tubercles in dorsocaudal subpleural areas which progress to larger confluent areas of caseous necrosis
- Usually start at bronchio-alveolar junction an progress to the alveoli
- Caseous lesions, may calcify or be encapsulated
- Multiple foci may coalesce
- Ulcers in trachea and bronchi due to coughed up bacteria
- Spreads into pleura
- Microscopically:
- Typical granulomatous inflammation
- Epitheliod and giant cells at centre of tubercles
- Macrophages with ingested bacteria, forming epithelioid cells - large vesicular nuclei, abundant pale cytoplasm
- Giant cells, formed by fusion of macrophages, with multiple nuclei
- Narrow layer of lymphocytes, mononuclear cells and plasma cells at the periphery of the tubercle
- With time, peripheral fibroplasia and central necrosis develop
- If the infection is not contained in the primary complex described above, the mycobacteria can disseminate via lymphatics to other organs and lymph nodes
- This can allow the development of miliary tuberculosis, i.e. numerous small foci of infection in many organs/ tissues
- inhalation of Mycobacterium bovis most common via droplets
- some tubercle bacilli enter the lymph and travel to the bronchial or mediastinal nodes
- inhaled bacilli reach the alveoli, set up a focus of inflammation
- phagocytosed by alveolar macrophages
- two processes may develop if the animal has not encountered the organism before:
- - the organism may grow in the phagocytes as intracellular parasites
- - produces a nodule of parasitised swollen macrophages known as a tuburculous nodule or a tubercle granuloma
- - ultimately, macrophages are killed and infection spreads
- - the organism may be broken down and some antigens taken up by the immune system
- - cell mediated immune system produces cytotoxic T-lymphocytes
- - T-lymphocytes can attack and destroy cells harbouring bacilli
- - leads to type IV (delayedd type) hypesensitivity
- - 'caseous' or cheesy type of necrosis
- - if bacterium destroyed, further infection/disease is prevented
Sequelae
- chronicity
Tuberculosis pleurisy
- caseous lymph node ruptures
- results from extensive tissue necrosis
- - if located in lung alveoli, the follicle may rupture into a bronchus, causing spread of the disease to all the other lobules served by that bronchus
- - if the ensuing necrosis erodes the wall of a large pulmonary vessel, this ruptures into the lung and a fatal haemoptysis might follow