| This article is still under construction. |
See also Pathology in WikiPath
Signalment
- Sled dogs
Description
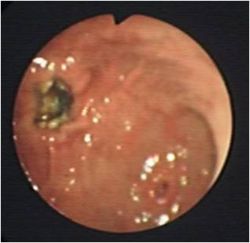
Is a round or oval punched out lesions ranging from 1-4 cm in diameter caused by damage to the gastric mucosa.
There are many disease associations including:
| Disease type | E.g. |
|---|---|
| Hypotension | Shock, Sepsis |
| Drug - induced | Non-steroidal anti-inflammatory drugs (NSAIDs) |
| Idiopathic | Stress, exercise induced |
| Inflammatory | Gastritis |
| Neoplastic | Adenocarcinoma, lymphosarcoma, leiomyoma |
| Metabolic/endocrine | Hypoadrenocorticism, liver disease, uraemia, Disseminated Intravascular Coagulation (DIC), mastocytosis and hypergastrinaemia |
Gastric ulceration is caused by damage to the gastric mucosa through the above mechanisms. NSAIDs directly damage the mucosa and interfere with the prostaglandin synthesis. Gastric ulceration is worsened by the use of NSAIDs in combination with corticosteroids. This risk can be minimised by using cyclooxygenase-1 (COX-1) sparing NSAIDs (carprofen, meloxicam and deracoxib).
Gastric acid hypersecretion following mast cell degranulation of histamine and gastrin secretion from gastrinomas is a major cause of gastric ulceration. Sled dogs and equine race horses are prone to gastric ulceration.
Diagnosis
History and Clinical Signs
History may involve:
- Access to toxins and drugs such as NSAIDs
Clinical Signs:
- Vomiting
- Haematemesis
- Malaena
- Pale mucous membranes
- Abdominal pain
- Weakness
- Inappetance
- Hypersalivation
- Circulatory comprimise
Haematology
- Anaemia - regenerative initially, may progress to microcytic, hypochromic and minutely regenerative.
- Thrombocytosis
- Lack of stress leucogram (and lymphocytosis and eosinophilia) supportive of hypoadrenocorticism
- Examination of the buffy coat may detect mastocytosis
- Neutrophilia and a left shift - signs of inflammation or gastric perforation
- May show abnormalities in haemostasis
Biochemistry
- Dehydration - azotaemia
- Hepatic disease - increased liver enzymes and bilirubin, decreased urea, albumin and cholesterol
- Renal disease - azotaemia
- Hypoadrenocorticism - Sodium:Potassium ratio of less than 27:1
- Vomiting will lead to electrolyte and acid-base abnormalities - metabolic alkalosis, hypokalaemia and hypochloraemia
Urinalysis
- Dehydration - Hypersthenuria
- Renal disease - Isosthenuria
Plain radiography
Not usually diagnostic but rules out differentials.
Positive contrast radiography
May show filling defects.
Ultrasonography
Shows gastric thickening and rules out differentials.
Endoscopy and Biopsy
Diagnostic test of choice and allows biopsies to be taken. NSAID related ulcers are reguarly located in the antrum and there is limited mucosal thickening or irregularity whereas ulcerated gastric tumours will have thickened mucosa and edges. Any biopsies should be taken at the edge of normal and diseased to avoid further deepening or perforation.
Treatment
The main aim is to treat any primary underlying cause whilst giving general support. This may be hydrating, restoring electrolytes and acid-base and also helping the gastric lining to recover.
Fluid Therapy
Depends upon degree of dehydration, prescence of shock and any other diseases that are affected by volume. Prolonged vomiting or anorexia may lead to hypokalaemia so KCl may need adding to any fluids given. Normal rates for treatment of shock apply with dehydration being overcome by a fluid rate over 24 hours to replace the defecits along with a maintenance rate.
Acid-base correction
Imbalances should be corrected after taking a blood gas reading.
- If metabolic acidotic: give sodium bicarbonate (1mmol/kg), but do repeated blood gas
- If metabolic alkalosis: replace volume defecit with intravenous NaCl and KCl.
- Blocking of acid secretion:
- Histamine receptor antagonists:
- cimetidine
- ranitidine
- famotidine
- Gastrin antagonists:
- proglumide
- Acetylcholine receptor antagonists:
- atropine
- pirenzepine
- Adenyl cyclase inhibitors:
- prostaglangin E2 (PGE) analogues (misoprostol)
- H+:K+ATPase inhibitors :- for use when patient is refractory to histamine antagonists
- omeprazole - good for exercise induced gastric ulceration
- Histamine receptor antagonists:
Mucosal protectants
Such as misoprostol can be given alongside NSAIDs to decrease the risk of ulceration. Sucralfate, which is polyaluminium sucrose sulphate, binds to damaged mucosa and assists in the treatment of gastric ulceration. It is best given 2 hours after acid inhibitors to prevent interference.
Prophylaxis
Prophylactic treatment has been shown not to prevent gastric ulceration. Sucralfate is reported to be the best drug in patients receiving high doses of glucocorticoids.
Anti-emetics
Indicated if vomiting is severe causing fluid and electrolyte imbalances and discomfort. See Anti-emetics for drug details.
Analgesia
Is best provided by opiods such as buprenorphine, pethidine and fentanyl.
Antibiotics
Animals suffering from shock and gastric barrier dysfunction may require prophylactic antibiotic cover. First line drugs include ampicillin or a cephalosporin which are effective against Gram-positive, some Gram-negative and some anaerobes. These can be combined with an aminoglycoside which are effective against Gram-negative aerobes if sepsis is present. Enrofloxacin can also be used instead of an aminoglycoside in skeletally mature animals
Surgery
May be required to investigate or to resect peforating ulcers which may lead to peritonitis.
Prognosis
Depends upon the cause
References
Hall, J.E., Simpson, J.W. and Williams, D.A., (2005) BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition) BSAVA