Thyroid Gland - Pathology
|
|
Anatomy and Physiology
Anatomy and Physiology of the Pituitary Gland ca be found here.
Functional Anatomy (summary)
The thyroid gland lies in the neck, in front of the upper part of the trachea. Two types of hormones are produced:
- Iodine-containing hormones: Tri-iodothyronine(T3) and Thyroxine (T4). Thyroid hormones regulate the basal metabolic rate and are important in the regulation of growth of tissues, particularly nervous tissue. Release stimulated by TSH from the pituitary.
- Calcitonin: Regulates blood calcium levels along with parathyroid hormone. Acts to reduce blood calcium by inhibiting its removal from bone.
The majority of the gland is derived from a downgrowth of the foetal tongue. The calcitonin producing cells are different and are derived from the fourth branchial pouch.
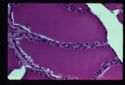
The throid gland is divided into follicles which are bounded by a single layer of cuboidal epithelial cells and a basement membrane. Follicles contain a homogenous colloid material called thyroglobulin. This is a store of thyroid hormones prior to secretion. The thyroid gland is the only endocrine gland to store its hormone in large quantities.
In the active gland:
- Colloid is diminished.
- Epithelial cells are tall and columnar.
Parafollicular cells are found in clusters in the interfollicular space. Also known as clear cells as their cytoplasm doesn't stain with H and E. These cells synthesise and secrete calcitonin in response to raised plasma calcium.
Goitre
Refers to a benign enlargement of the throid gland. May be hypofunctional or hyperfunctional. (More often see increased function with neoplasia of the thyroid or the pituitary glands).
Diffuse parenchymatous goitre
Hypofunctional goitre, low levels of thyroglobulin is produced.
Aetiology:
- Dietary iodine deficiency.
- Goitrogenic compounds E.g. Thiocyanates. Reduce uptake of iodine by the thyroid. Includes rape, kale and white clover.
Most often seen as a congenital disease in areas with iodine deficient soil.
Clinical signs:
- Lamb/calf/piglet born dead or moribund.
- Hairless.
- Oedema of head and neck.
Pathophysiology:
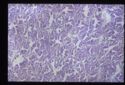
No thyroid hormones are produced and there is overstimulation of the thyroid gland by TSH as there is no negative feedback. Histopathologically seen as hyperplasia of the epithelial lining cells as they are stimulated by TSH. Very little colloid is formed as no iodine is available and the epithelial cells form papillary ingrowths into the follicle centre.
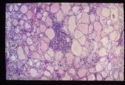
Diffuse colloid goitre
Also hypofunctional. Failure at the pituitary level to produce TSH. TSH is needed for the release of thyroglobulin so without it colloid will accumulate and the follicles will become inactive, seen as:
- Large amounts of densely staining colloid.
- Flattened, low cuboidal epithelium.
- Follicles may coalesce to form cystic spaces.
Usually due to damage to the TSH producing cells of the pituitary.
Nodular goitre
Results from a cycle of hyperplasia and hypoplasia.
Hypothyroidism
The most commonly described endocrinopathy in the dog. Multiple possible aetiologies, including:
- Primary hypothyroidism:
- Congenital: Cretinism, rare.
- Acquired: E.g. Neoplasia. Represents 90% cases.
- Secondary hypothyroidism: Pituitary dysfunction ,10% cases.
- Tertiary hypothyroidism: Hypothalamic dysfunction, rare.
- Miscellaneous E.g. iodine deficiency, rare.
Clinical signs:
- Lethargy
- Obesity
- Intolerance to cold
- Bradycardia
- Bilaterally symmetric, non-pruritic alopecia
- Occasional neurological signs with neoplasia
Cretinism
Affected animals are disproportionate dwarfs with broad skull, heavy legs and an ataxic gait. Thyroid hormones are needed for normal osteogenesis and endochondral ossification. Also see myxoedema (deposition of mucoid material in the skin giving a tragic facial expression).
Lymphocytic thyroiditis
Causes primary hypothyroidism in the adult. Exact aetiology unknown but thought to be an autoimmune disease. Thyroid has an infiltrate of lymphocytes. See fibrous replacement of thyroid tissue which progresses to complete destruction. Clinical signs are not seen until 75% of the functional tissue of the thyroid is lost.
Similar disease to Hashimotos thyroiditis in humans.
Primary hypothyroidism in the adult animal may also be due to;
- Neoplasia
- Goitre
- Atrophy
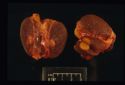
Hyperthyroidism
Seen most commonly in the cat. Elderly cats are affected with the average age of onset being 12-13 years.
Clinical signs:
- Weight loss despite polyphagia
- Increased activity, nervousness (approximately 10% will show apathy)
- Polyuria and polydipsia
- Heat intolerance, panting
- Tachycardia >240 bpm
- Poor coat, matted and unkempt
- Palpable thyroid mass often present
Often see a hypertrophic cardiomyopathy due to chronically increased heart rate and activity.
Aetiopathogenesis:
>98% are a functional adenoma of the thyroid gland and many will be palpable.
Treatment:
Surgical removal of the affected thyroid gland(s). If bilateral it is important to preserve at least one parathyroid gland to maintain calcium homeostasis.
Medical treatment:
- Carbamizole: Interferes with thyroid hormone synthesis.
- Radioactive iodine therapy. Useful for intrathoracic thyroid nodules.