Principles of Fluid Therapy
What is Fluid Therapy?
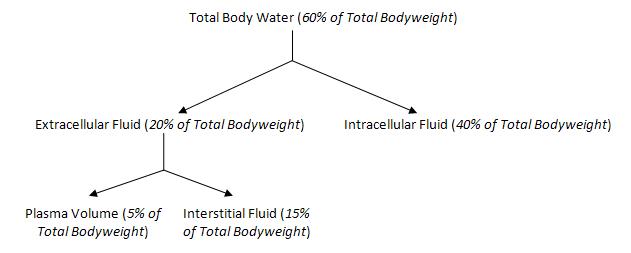
Fluid Therapy is the administration of fluids to a patient as a treatment or preventative measure. It can be administered via an intravenous, intraperitoneal, intraosseous, subcutaneous and oral routes. 60% of total bodyweight is accounted for by the total body water. This can further be divided into intracellular or extracellular as shown below.
Fluid therapy is indicated either when there is a loss of fluid to any part of these compartments or there is a risk of loss of fluid. The severity of the fluid loss, and the compartment from which it has been lost, influence the choice of fluid and the speed at which it needs to be administered. If fluid therapy is performed as a treatment then it is necessary to diagnose and treat the underlying condition.
Indications
- Hypotension
- Hypovolemia
- Electrolyte, metabolic and acid base disorders
- Decreased oxygen delivery
- Geriatric patients at risk of organ failure
Definitions
- Osmosis is the net movement of water across a semi permeable membrane. The movement is caused by a concentration gradient due to different solute concentrations on each side of the membrane.
- Osmotic Pressure is the pressure caused by the solutes within the solution. The solute concentration prevents water movement across the membrane.
- Tonicity is the term used to compare the osmotic pressure of different solutions
- A hypotonic solution is one that has an osmotic pressure lower than plasma.
- A isotonic solution is one that has an osmotic pressure the same as plasma.
- A hypertonic solution is one that has an osmotic pressure higher than plasma.
- 'Hypovolaemia is a reduction in normal blood volume which can be caused by:
- Excessive sweating
- Water deprivation
- Vomiting and diarrhoea
- Haemorrhage
- Pathological dilatation of capacity of the ciruclatory system, and therefore a relative reduction in circulating blood.
- Hypervolaemia' is an increase in blood volume, which can be caused by congestive heart failure.
Types of Fluids
- Crystalloids are able to enter all body compartments.
- Colloids are restricted to the plasma compartment.
If there is an electrolyte imbalance present then it may be necessary to add the appropriate electrolyte solution.
Fluid Rate Calculations
When calculating the fluid requirements of a patient, there are 3 elements to consider -
- Replacement
- Maintainance
- Ongoing Losses
Replacements are calculated based on the level of dehydration. Dehydration is based upon clinical assessment of each individual patient. Most commonly, skin tent is used for assessment. To calculate the amount required for replacement within a 24 hour period, the percentage dehydration is used in the following calculation.
| Replacement = % Dehydration x Bodyweight (kg) x 10 |
|---|
Maintainance is the basic rate which a patient requires during a 24 hour period. It is commonly calculated as 50ml/kg/24hr, or 2ml/kg/hr.
Ongoing losses are calculated based on a predicted fluid amount lost by a patient within a 24 hour period. Common losses include vomitting and diarrhoea. It is often helpful here if the owners are able to give a detailed history as this makes it easier to predict the pattern of losses. In some patients there may be no ongoing losses and so this step can be skipped. To calculate the fluid requirement, the following calculation is used.
| Ongoing losses = Amount per loss (ml/kg) x Bodyweight (kg) x No. of losses |
|---|
These calculations are then added together to allow for the total fluid requirement in a 24 hour period. It is important to assess these requirements on a daily basis as losses may be increased/reduceed for example.
The calculated fluid requirement is multiplied by the bodyweight of the individual patient to give the total amount of fluid required for that patient as ml/24hr period. This is then further calculated depending on whether a drip pump is used or fluid rate is adjusted manually as shown below.
| Requirement per hour (ml/hr) = Requirement per day (ml/24hr) ÷ 24
|
|---|
Monitoring Fluid Therapy
Fluid therapy can be monitored by observing urine output, Packed Cell Volume (PVC), Total Protein (TP, or Total Solids, TS), mucous membrane colour, and blood pressure among others. It is important to also observe for signs of oedema, such as pulmonary oedema or ascites. It should not be stopped until hydration of the patient has returned to normal and the patient is able to maintain a normal hydration status independently.
Special Considerations
Shock
Shock is defined as decreased oxygen delivery or utilisation by tissues that may lead to irreversible cellular damage if prolonged. Patients who present in a state of shock require immediate fluid therapy. To assess whether a patient is in shock the following signs may be seen -
- Tachycardia
- Pale mucous membranes (May be dark if distributive shock)
- Prolonged/Absent capillary refil time
- Reduced/Absent periperhal pulses
- Hypotension
There are 3 forms of shock:-
- Hypovolemic is seen when there is reduced circulating blood volume and the most common form of shock.
- Cardiogenic is seen in any condition when there is a failure for the heart to pump effectively.
- Vascular can be sub-divided into -
- Obstructive is seen when there is an obstruction to blood flow to a region of tissue.
- Distributive is seen when there is inappropriate vasodilation. This leads to changes in blood flow distribution between tissues.
The first choice fluid in hypovolemic shock cases are isotonic crystalloid fluids and are given at a high flow rate. They are often administered as a rapid bolus followed by the high flow rate. In cardiogenic shock cases, often the patient is already in volume overload and so often treated with a diuretic. Obstructive shock is often treated by removal of the obstruction.
Anaesthesia
Pre-anaesthetic
Before an anaesthestic is performed, it is important to stabilise a patient, both fluid deficits and any electrolyte or acid-base inbalances. In many cases, it is ideal to have a minimum blood database. This should include PCV and TP and if possible urea, creatinine, electrolyes and glucose. If there is any evidence of haemoconcentration, azotemia, or electrolyte imbalances then the patient should be given fluids to correct these abnormalities before the anaesthetic. Even if these parameters are normal it is often advisable to place the patient on fluids as most anaesthetic agents will alter fluid homeostasis, even in healthy patients.
When giving fluids ideally they should be warmed to help the patient maintain a normal body temperature.
Intra-anaesthetic
During an anaesthetic, normal homeostatic functions of the patient are altered and so fluid therapy should be initiated to any patient undergoing an anaesthetic to allow for maintained fluid balance. During any procedure, glucose levels should be closely monitored, especially patients with diabetes, liver disease or paediatric patients. If necessary it is then possible to add glucose or dextrose to the fluid the patient is receiving.
Some patients may develop an anaesthetic-induced hypotension from the side-effects of the agents used to induce and maintain anaesthesia. Fluids are therefore often given as a preventative measure. If there is significant blood loss during a procedure, it is necessary to replace these losses, either using blood products or an appropriate fluid.
As mentioned previously, it is also ideal to administer warm fluids to a patient to help maintain a normal body temperature during any procedure. This can be done by warming the fluids in a water bath, or wrapping the giving set line around a glove of warm water to help warm the fluids before they reach the patient.
Post-anaesthetic
If a patient has been receiving fluids during a procedure, it is often continued after until the patient is either stable and fully recovered from the anaesthetic. The length of time the fluids continue for after the procedure is dependent on the individual patient and the individual case.
Cardiac Disease
It is important to avoid fluid overload in cardiac patients who often have reduced cardiac function. This means it is important to closely monitor fluid adminstration in these patients as it may worsen the patient's condition.
Hepatic Disease
Patients with hepatic diease often have alterations in protein levels due to reduced production, as well as changes in clotting factors. Hypoproteinemia will affect patients undergoing anaesthetics as many agents are protein bound so the reduction in protein means that more of the agent may be available. However, the hypoproteinemia may also be affected by the adminstration of certain fluid types so it is important to have a baseline so that the most appropriate fluid can be selected.
If there are any clotting disorders then it may be necessary to give blood products so that the missing clotting factors are available to the patient, while the underlying cause is diagnosed and treated.
Central Nervous System Disease
Patients with head trama or increased intracranial pressure are particularly suscetible to insufficient or excessive fluid loading. It is therefore with care that fluids are administered and monitored. The choice of fluid is dependent on the other clinical signs of the patient such as haemodynamics. The status of the blood brain barrier is an important consideration in any patient and in the selection of fluid. However, fluids containing glucose should be avoided in these patients.
Literature Search
Use these links to find recent scientific publications via CAB Abstracts (log in required unless accessing from a subscribing organisation).
Why did fluid therapy kill my patient? Schaer, M.; Gething, M.; Jones, B.; Australian Small Animal Veterinary Association, Bondi, Australia, 33rd World Small Animal Veterinary Association Congress, Dublin, Ireland, 20-24 August 2008, 2008, pp 437-439 - Full Text Article