Thrombosis
Introduction
Thrombosis may be due to:
- Endothelial injury.
- Altered blood flow E.g. abnormal stasis.
- Hypercoagulability.
Often associated with other disease processes such as disseminated intravascular coagulation (DIC).
Commonly see posterior paralysis of cats with cardiomyopathy.
Spontaneous venous thrombosis is rare. Seen in cattle with traumatic reticulo-peritonitis in the caudal vena cava.
Description
Thrombosis is a localized or generalized intravascular clot formation. Thrombi form as the result of trauma or pathological processes affecting the blood vessel endothelium or disturbances to blood flow and/or blood composition. Some diseases such as infective endocarditis and heart worm increase the risk of thrombi formation.
Diagnosis
History & Clinical Signs
- Signs depend on the area affected and the size of the blocked vessel.
- Poor perfusion below affected area.
- Malfunction and necrosis of affected organs
Laboratory Findings
Abnormalities associated with lack of blood perfusion and/or pathological conditions.
Ultrasonography
- Blood stasis
- Visualization of a thrombus
Angiography
- May show lack of opacity in affected region
Treatment
- Treat underlying problem
- Give IV Fluids
- Use an anticoagulant (Heparin for short term treatment, Aspirin for long term treatment)
Prognosis
Prognosis depends upon the underlying condition.
Pathophysiology
Terminology
- A thrombus is a solid blood clot that forms within the vessels or heart during life.
- The process of thrombus formation is known as thrombosis.
- Thrombii may occur anywhere within the cardiovascular system.
Thrombosis formation
The process usually begins with platelets becoming sticky. They adhere to each other and to the endothelium. This increased "stickiness" is induced by contact with:
- Collagen
- Basement membrane
- Damaged endothelial cells
- Bacteria
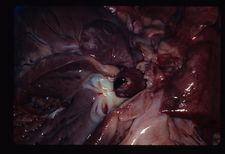
Microscopic Appearance of a Thrombus
A thrombus is a layered mass which is attached to the vessel wall. The composition consists of red blood cells, [[Neutrophils - WikiBlood|neutrophils]] and platelets bound together by fibrin.
Thrombi take different appareance depending on whether they are arterial or venous:
- Arterial thrombi tend to be pale and have a tail in the direction of blood flow. The high rate of blood flow sweeps red cells away - the thrombus is composed of mainly white cells, platelets and fibrin which are left behind.
- Venous thrombi tend to be a darker red. The slow blood flow allows the clot to form quicker which is loosely arranged and contains many red blood cells.
Causes of Thrombosis
- Thrombosis is caused by any condition that allows platelets to adhere to the endothelial wall.
Damage to the Vessel Wall
- When there is damage of the overlying endothelium, collagen is exposed and platelets will attach to this.
- The blood clotting process will occur, giving formation of an intraluminal blood clot.
- The process of formation occurs in phases giving a cross section of the clot a laminated appearance.
- The blood clotting process will occur, giving formation of an intraluminal blood clot.
- Vessel walls may be damaged in several ways:
- Trauma
- Localisation by colonies of bacteria
- Viral infection of endothelial cells
- Migration of parasites.
- Repeated puncture of the jugular vein is a common cause of serious or fatal thrombosis.
Changes in Normal Blood Flow
Stasis
- Stasis prevents coaglation factors being cleared by the liver and reticuloendothelial system.
- Coagulation factors build up, leading to clot formation.
- When stasis occurs in a vein, the thrombus forms behind the valve cusps.
- Quickly enlarges to fill the lumen.
Turbulence
- Turbulence disrupts the laminar flow.
- Platelets are brought into contact with the endothelial wall and may even damage the endothelium.
- Thrombi tend to form at arterial branches and venous junctions where there are eddy currents and local stasis.
Changes in Blood Composition
- An increase in the number and adhesiveness of platelets, or in plasma fibrin and clotting factors results in a hypercoagulateable state
- There may also be a decrease in the activity of the fibrinolyltic system.
- This may be caused by surgical or traumatic shock, or inflammation with toxaemia.
Types of Thrombosis
Arterial Thrombosis
- Although this is common in man, it is uncommon in domestic animals.
- A major problem in man associated with atherosclerotic vascular disease.
- When they do occur in animals, arterial thrombi are usually small lesions.
- However, these may be sited strategically, thereby causing problems.
Arteriosclerosis
- Seen in aged dogs and horses.
- Affect the coronary artery and other major arteries.
Verminous arteritis
- May occur with or without aneurysm.
- Seen in horses as a result of Strongylus vulgaris infestation.
- Affects the root of cranial mesenteric artery, renal artery and aorta.
- Results from larval migration in vessel walls.
Iliac thrombosis
- Seen in cats in the UK.
- Often referred to as "saddle embolus".
- Associated with cardio-myopathy and atrial thrombosis.
Cardiac Thrombosis
- Cardiac thrombosis is usually valvular, but can occasionally be mural.
Farm Species
- In farm animals, and rarely in the horse, infective/ inflammatory thrombosis occurs.
- Known as endocarditis.
Dogs and Horse
- Cardiac thrombosis is generally of degenerative/ non-infectious cause.
- Endocarditis may occur, though uncommonly.
- There are important effects of cardiac thrombosis.
- Distortion of valve cusps leads to mechanical effects.
- Ineffective closeure gives leakage (incompetence).
- Distortion and enlargement of the valves by the thrombus mas fuves narrowing of the valve outflow (stenosis).
- These effects lead to progressive inefficiency of cardiac pumping.
- Causes general venous congestion, oedema and circulatory failure.
- Emboli are disseminated from the thrombus mass.
- If the lesion is on the left side of the heart, emboli are disseminated systemically.
- Become trapped in the capilarry beds, e.g. of the kidney and spleen.
- Blockage leads to local ischaemic necrosis.
- Become trapped in the capilarry beds, e.g. of the kidney and spleen.
- If the lesion is on the right side of the heart, there is pulmonary dissemination.
- If the lesion is on the left side of the heart, emboli are disseminated systemically.
- Distortion of valve cusps leads to mechanical effects.
Atrial Thrombosis
- Uncommon.
- Seen rarely in cats and dogs.
- Results from stasis in atrial appendages.
Venous Thrombosis
Description
- Thrombus formation in the venous system occurs most commonly as the result of trauma, venous catheterisation, or neoplastic conditions.
- Obstruction of the affected area or embolisation of the thrombus to distant areas results in a variety of clinical signs. As could be expected, the location of the insult determines the type of presenting signs. For example, pulmonary emboli cause respiratory problems while portal vein thrombi result in ascites and the possible development of hepatic encephalopathy or portosystemic shunting.
- Venous thrombosis is a fairly common type of thrombus in the veterinary species.
- This is because:
- Veins are relatively thin-walled.
- Are therefore more susceptible to distortion, inflammatory damage and iatrogenic vene puncture damage.
- Veins have relatively slower blood flow rates.
- Cell aggregates tend to persist more readily.
- Veins are relatively thin-walled.
- This is because:
- Most venous thrombosis in domestic animals results from :
- Extension of inflammatory reactions.
- Erosion/disruption caused by malignant tumours.
- Pressure from adjacent space-occupying masses.
- Vene puncture damage.
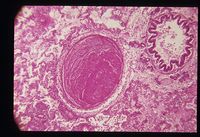
Capillary Thrombosis
- These are microthrombi.
- Only appreciable histologically.
- Formation may be:
- Localised
- Associated with acute local inflammation.
- Not very significant unless strategically sited.
- Generalised
- May be seen in terminal disease as a reflection of vascular failure.
- Often associated with shock syndromes as part of disseminated intravascular coagulation.
- Clinically very significant.
- Localised
Evolution of a Thrombus
- If the animal survives the immediate effects of a thrombus, the thrombus may evolve in one of the following ways:
- The thrombus may gradually enlarge and eventually cause total obstruction of a vessel.
- The thrombus may be completely removed by fibrinolytic activity.
- Fibrinolysis is a very active process - clots are usually removed within a few days of formation.
- Blood flow is crucial to the process of fibrinolysis.
- An occlusive thrombus may prevent the necessary enzymes from reaching the clot.
- To overcome occlusion, contraction of fresh clots under the influence of thrombasthenin (released by platelets) forms a slit-like channel beside the thrombus.
- The blood that then flows past may completely dissolve the clot.
- Organisation
- A thrombus acts as a foreign body, causing an inflammatory response in the underlying blood vessel or heart wall.
- The external surface of the thrombus quickly becomes covered by endothelium.
- Is excluded from the clotting mechanism.
- Neutrophils invade the mass and may digest the centre.
- Occasionally, subsequent invasion by bacteria may lead to to purulent inflammation.
- Normally, fibroblasts and capillary buds follow the neutrophils into the thrombus and a fibrous vascularised connective tissue forms.
- Capillaries channels anastomose to produce vessels that traverse the thrombus and re-establish blood flow.
- This is known as canalisation of a thrombus.
- Fibrous tissue matures and contracts, eventually causing the thrombus to become incorporated into the vessel wall as a fibrous lump.
- Capillaries channels anastomose to produce vessels that traverse the thrombus and re-establish blood flow.
- A piece of the thrombus may break off and form an embolus.