Regenerative and Non-Regenerative Anaemias
Introduction
Anaemia refers to a reduction in packed cell volume (PCV), haemoglobin concentration or the level of total red blood cells. In the clinical approach to the anaemic patient, the initial step is to determine whether the anaemia is regenerative or non-regenerative. Regeneration refers to the production of new erythrocytes from the bone marrow and their subsequent release into the circulation. In dogs, there is a lag period of 48-72 hours before immature red blood cells (reticulocytes and nucleated red blood cells ) begin to appear in the circulation and the extent of the regenerative response is usually in proportion to the severity of the anaemic insult.
Causes of Anaemia
The major causes of anaemia are:
- Immune-mediated disease including immune-mediated haemolytic anaemia, a disease caused by an autoimmune response directed against endogenous erythrocytes, and neonatal isoerythrolysis, the result of a maternal immune response directed against foetal antigens inherited from the sire.
- Haemorrhage
- Haemolysis
- Anaemia of Chronic Disease
- Infectious Diseases, notably:
- Equine Infectious Anaemia caused by EIA virus.
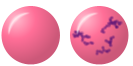
- Canine and feline infectious anemia caused by Mycoplasma haemocanis and Mycoplasma haemofelis respectively. Candidata M. haemominutum and M. turicensis may also cause anaemia in cats.
- Leptospira spp. may cause anaemia, usually when an animal is exposed to a non-host-adapted serovar.
- Babesia spp. may cause anaemia in dogs and cattle.
- Hepatozoon spp. in dogs and pigs.
- Clostridium haemolyticum causing Redwater Fever in cattle.
Regenerative or Non Regenerative?
The following features may be used to determine whether anaemia is regenerative or non-regenerative:
| Feature | Regenerative | Non-regenerative | Image |
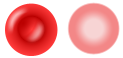
| Mean Corpuscular Volume (MCV) | Increased as reticulocytes are larger than mature erythrocytes | Normal | |
| Mean Corpuscular Haemoglobin Concentration (MCHC) | Decreased as reticulocytes are larger cells and less packed with haemoglobin (as the marrow is trying to produce cells at a faster rate it means they are not as well formed) and they also contain the remnant of the ribosomal RNA that is lost with progressive development of the cell | Normal | |
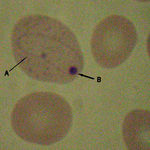
| Blood Smear | Howell-Jolly bodies may be present as small basophilic spots within red blood cells. These represent the remnant of the endoplasmic reticulum of the erythrocyte. Large polychromatic red blood cells may be evident when the smear is stained with a Romanowsky stain. These cells probably represent reticulocytes but this cannot be confirmed unless a smear is also stained with a supra-vital stain such as new methylene blue. This latter procedure can be used to estimate the degree of reticulocytosis and to determine if this is appropriate to the severity of the anaemia. |
The red blood cells are usually normochromic and normocytic but poikilocytosis may be apparent in cases of maturation defect anaemia. |
Regenerative Anaemia
The major causes of regenerative anaemia are haemorrhage and haemolysis.
Haemorrhage
This may be acute, transient severe haemorrhage or chronic, persistent haemorrhage. There may be evidence of blood loss, such as external haemorrhage from wounds, lesions or body orifices (nares, anus); may be associated signs of trauma (RTA) or possibly defective haemostasis. Internal haemorrhage may be intracavity or into the GI or urinary tract and evident in excreted material (urine, faeces, vomit). It can appear as fresh or altered blood. Small amounts of blood may not be visible to the naked eye but may be visualized microscopically or detected chemically.
Immediately following acute haemorrhage the PCV and other RBC indices remain relatively stable, whole blood has been lost and haemodilution, due to fluid shifts from the extravascular to the intravascular compartment, takes time to develop. Splenic contraction may also helpmaintain the PCV. After 2-3 hours, haemodilution becomes evident, leading to reductions in red cell indices and plasma protein concentrations. The full magnitude of blood loss may not be evident until 24hrs after the onset of haemorrhage. Red cell indices may be less affected following haemorrhage into body cavities because two thirds of the erythrocytes may return to the circulation; plasma proteins and iron from the remaining RBCs are retained and can be utilised for erythropoiesis. Anaemia is initially normocytic normochromic but after 2-4 days there is a significant erythroid response, which is most marked by day 7, and features polychromasia, reticulocytes, Howell-Jolly bodies, nucleated RBCs, increased MCV. If reticulocytosis and thrombocytosis, with reduced plasma proteins persist after 2-3 weeks, continuing haemorrhage should be suspected. PCV should have returned to low normal by 2 weeks following a single episode of haemorrhage.
By the time chronic haemorrhage causes clinical signs of anaemia, regeneration should have begun, The regenerative response is more marked with acute haemorrhage. With persistent chronic haemorrhage, particularly with blood loss from the body, the RBCs may be microcytic and hypochromic due to iron deficiency. There is initially an increased reticulocyte count which then falls as iron deficiency develops.
Even after haemorrhage the regenerative response may be poor or absent if the bone marrow is damaged or activity is suppressed by, for example, neoplasia or infection.
Leucocyte changes. Acute blood loss is usually accompanied by a leucocytosis with neutrophilia and a left shift (in- creased band cells). This is not associated with infection but may reflect inflammation secondary to hypoxic damage. Immediately post haemorrhage there may be a mild to moderate transient thrombocytopaenia due to increased platelet consumption; this is followed by thrombocytosis with large immature platelets, reflecting the bone marrow response to increased demand.
Chronic blood loss is often associated with thrombocytosis (platelet count 500-1000x109/l).
Biochemical changes. Plasma protein and albumin levels will be low after severe acute haemorrhage and may be low with chronic haemorrhage.
Increased blood urea nitrogen with normal serum creatinine can be seen with gastrointestinal haemorrhage.
References: NationWide Laboratories
Any form of spontaneous haemorrhage with no apparent cause may suggest the presence of an underlying coagulopathy. The most common haemorrhagic presentations are:
- Epistaxis due to disruption or erosion of blood vessels of the nasal cavity by trauma, neoplasia, fungal infection or a foreign body.
- Haematuria which may arise due to haemorrhage from any part of the urinary tract, especially the kidney (due to trauma, neoplasia or idiopathic haematuria) and bladder (due to trauma, cystitis, urolithiasis and neoplasia).
- Melaena, haematochezia or haematemesis due to gastro-intestinal haemorrhage. Meleana refers to the production of black tarry faeces with digested blood whereas haematochezia refers to the production of fresh blood with the faeces. Classically, haematemesis is described as resembling 'coffee grounds' as blood is denatured by a low gastric pH but, as the gastric pH of the dog may vary widely between 2 and 6, vomited blood may also appear as fresh red blood.
- Haemoptysis refers to the production of blood from the respiratory tract. It may occur with severe forms of pneumonia and with pulmonary haemorrhage.
- Haemoabdomen, haemothorax and haemopericardium are all forms of haemorrhagic effusion that occur in body cavities.
Haemolysis
Usually presents as a markedly regenerative anaemia without hypoproteinaemia or other evidence of blood loss. Haemolysis may be intravascular or extravascular.
- Extravascular haemolysis relates to the pathological phagocytosis of erythrocytes by macrophages in spleen, liver and bone marrow and is the most common form of
haemolytic anaemia.
- Intravascular haemolysis relates to destruction of erythrocytes within the circulation and often results in more acute and severe haemolysis then extravascular haemolysis. Haemoglobinuria is often a feature. The most common causes are complement fixing immune-mediated haemolytic anaemia and Heinz body anaemia.
- When both forms occur together, the haemolysis is classified by the predominant type.
- Haemolytic anaemias often result in a degree of hyperbilirubinaemia which, if sufficiently severe, will be evident as icterus. RBC destruction leads to an increased level of unconjugated bilirubin which exceeds the rate of hepatic excretion. Acute severe anaemia may also cause hypoxic or toxic hepatic injury, resulting in decreased bilirubin metabolism and cholestasis. Although hyperbilirubinaemia results primarily from increased unconjugated bilirubin, conjugated bilirubin also increases and leads to bilirubinuria. Evaluation of unconjugated versus conjugated bilirubin is often not helpful when trying to differentiate between pre-hepatic and hepatic jaundice.
References: NationWide Laboratories
Haemolysis may occur in the following processes:
- Immune-mediated disease including Immune Mediated Haemolytic Anaemia and Neonatal Isoerythrolysis.
- Infectious agents including Babesia spp. in dogs and cattle, Mycoplasma haemofelis in cats, Leptospira spp. in various species and Clostridium haemolyticum causing redwater fever in cattle.
- Inherited defects of red blood cells enzymes including pyruvate kinase (which is occur most commonly in West Highland white terriers) and phosphofructokinase (PFK).
- Pyruvate Kinase deficiency. This is an autosomal recessive genetic disease in dogs causing severe persistant extravascular haemolysis. There is usually moderate to severe anaemia (PCV18-25%) with marked reticulocytosis, possibly due to rapid RBC turnover and splenomegaly. PK-deficient RBCs have a shortened life span with inefficient energy production. Affected dogs are young and usually die by the age of 3 years with, in many cases, myelofibrosis and osteosclerosis. PK deficiency is transmitted as an autosomal recessive trait in many breeds of dogs with the highest prevalence in Basenji’s and Beagle’s. PK deficiency has been reported in the DSH, Abyssinian and Somali breeds of cat. References: NationWide Laboratories
- Phosphofructokinase deficiency. Has been reported in English Springer spaniels and Cocker spaniels. Commonly there is recurring haemoglobinuria, splenomegaly and/or icterus. Intravascular haemolysis is precipitated by respiratory alkalosis associated with stress induced hyperventilation. A haemolytic crisis may develop following exercise. References: NationWide Laboratories
- Hypophosphataemia which occurs in post-parturient cattle (causing post-parturient haemoglobinuria), with refeeding syndrome and when animals with diabetes mellitus are stabilised with insulin.
- Exposure to toxins including rape and kale (which contain SMCO radicals) in cattle, onions and garlic in dogs and paracetamol in cats.
- Microangiopathic anaemia which occurs when red blood cells are forced through small meshworks of fibrin as with haemangiosarcomas, disseminated intravascular coagulation (DIC) or bacterial endocarditis.
Haemolysis usually results in a more strongly regenerative response than haemorrhage and can be differentiated by plasma protein concentrations; these will fall with haemorrhage, but not with haemolysis.
Non-regenerative Anaemia
The failure to regenerate indicates that there is a failure to produce red blood cells in the bone marrow. Erythrocytes are produced from stem cells in the bone marrow and they then undergo sequential stages of maturation before and after they are released into the circulation.
Failure of the bone marrow stem cells to produce erythroid cells
This occurs in the following conditions:
- Pure red cell aplasia
- Aplastic anaemia
- Bone marrow suppression
- Myelophthisis
- Myelodysplasia
Failure of erythrocyte maturation
This can occur with:
- Iron deficiency
- Vitamin B12/folate deficiency
| Regenerative and Non-Regenerative Anaemias Learning Resources | |
|---|---|
To reach the Vetstream content, please select |
Canis, Felis, Lapis or Equis |
 Test your knowledge using flashcard type questions |
Feline Medicine Q&A 08 |
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |