Interstitial Pneumonia
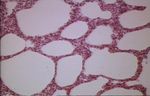
Revision as of 18:05, 19 February 2011 by Bara (talk | contribs) (Created page with "[[Image:Interstitial pneumonia micro.jpg|right|thumb|150px|<small><center>Interstitial pneumonia (Image sourced from Bristol Biomed Image Archive with permission)</center></small...")
- Lung inflammation that occurs primarily in alveolar walls rather than in alveolar spaces
- Can be widely distributed but is often most severe in caudal lung lobes
- Diffuse or patchy damage to alveolar septa, may be acute or chronic
- Lesions in most cases result from blood-borne insult and are more likely to involve the dorsocaudal regions, although the damage is often diffuse
- No concentrated inflammatory response in the airway, only secondary to damage of alveolar walls
- As part of systemic infection
- Canine distemper (in alveolar macrophages as inclusions)
- Salmonellosis
- Toxoplasmosis (in alveolar wall)
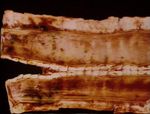
- Acute interstitial pneumonia is characterised by exudation into the alveolar lumen and in cattle is associated with interstitial emphysema
Examples:
Acute bovine pulmonary emphysema and oedema (ABPEE)
- Synonym: fog fever
- Usually seen in adult beef cattle in the autumn as an outbreak
- Associated with a change in pasture (from dry to lush, green)
- Severe respiratory distress with laboured breathing and grunting on expiration
- Can result in diffuse fibrosing alveolitis
- Gross appearance is that of enlarged wet lungs, the interlobular septa are markedly widenedith oedema and emphysema
- Underlying pathogenesis is ingestion of L-tryptophan in the pasture which is metabolised to 3-methylindole -> bloodstream -> lungs -> metabolised into a compound toxic to Type 1 pneumonocytes and non-ciliated bronchiolar epithelium
- Their loss allows massive flooding of the alveoli with a protein-rich fluid
- The sequence of events in the lung is as follows:
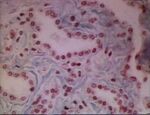
- Alveolar flooding with a protein-rich fluid due to the necrosis of Type 1 epithelium
- As the incoming air dries this fluid, fibrinous 'hyaline membranes' form
- Proliferation of the more resistant cuboidal Type 2 epithelium which line the alveoli, called 'epithelialisation'
- Then either there is
- Digestion of the hyaline membranes by macrophages which when completed, allows some of the proliferated Type 2 epithelium to differentiate into Type 1 and reconstitute the functional respiratory unit - a normal alveolus
- Or
- Organisation of the fibrin into fibrous tissue in the lumen - destroying the alveolus or proliferation of fibrous tissue in the alveolar wall with retention of the epithelialised appearance to the alveolus
- Sequel
- Residual scarring if animal survives initial onslaught
- In chronic exposures there may be extensive fibroplasia
- Ingestion of sweet potatoes ifested with Fusarium solani mould or pasture contaminated with stinkweed or purple mint, rapeseed and kale also cause pulmonary oedema, emphysema and interstitial pneumonia
Paraquat Poisoning
Diffuse alveolitis
- Chronic disease of adult cattle occuring sporadically
- Probably caused by repeated subclinical incidents of fog fever or farmer's lung
- Farmer's Lung
- Extrinsic allergic alveolitis
- Hypersensitivity of ingested or inhaled moulds
- May occur as an outbreak or sporadically in adult cattle
- Hypersensitivity diseases often cause an lymphocytic interstitial pneumonia
- Chronic interstitial pneumonia progresses to fibrosis
- Sometimes called pneumonitis