Innate Immunity Cellular Responses
Revision as of 15:57, 13 August 2010 by Bara (talk | contribs) (Created page with "thumb|right|125px|<p>'''Macrophage'''</p><sup>© Nottingham Uni</sup> * If pathogens breach the barriers formed by the skin and mucus membra...")
- If pathogens breach the barriers formed by the skin and mucus membranes, they must be detected and destroyed by cellular and humoral means
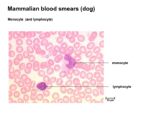
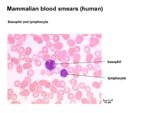
- The cells involved with innate protection are:
- Blood granulocytes, or Polymorphonuclear Cells
- Notable for their multi-lobed nuclei
- Neutrophils: phagocytose bacteria
- Eosinophils: kill parasites by the release of granules
- Basophils/ mast cells: kill parasites by the release of granules
- Blood [[monocytes]]: phagocytose bacteria
- Tissue mast cells and macrophages: phagocytose bacteria
- Blood granulocytes, or Polymorphonuclear Cells
- Effectively, innate cellular response seeks to hold off the infection until the adaptive response can back it up with a more specific attack
Macrophages
- The role of macrophages in Innate Immunity is to act as primary phagocytes
- Macrophages are present within tissues and take the form of distinct, tissue-specific populations:
- Alveolar macrophages
- Tissue histiocytes
- Glomerular macrophages
- Hepatic Küpffer cells
- CNS microglia
- Sinus-lining macrophages of the lymph nodes and spleen
- Monocytes (immature macrophages) are circulating phagocytes
- Circulate for 6-8 hours
- Can function as phagocytes within the blood and as newly migrated cells in tissues
- Chiefly function to replace the various tissue macrophage populations
Neutrophils
- Neutrophils are the principal, highly active phagocytes in the blood
- Comprise 30-70% of white blood cells depending on species
- Kill and digest microbes in a similar way as macrophages
- Neutrophils can also cause extracellular bacterial killing by disrupting bacterial membranes
- Secrete small antibacterial peptides
- E.g. defensins and bactenecins
- Secrete small antibacterial peptides
- Neutrophils produce vasoactive peptides
- E.g. histamine and bradykinin
- Cause a great increase in extravasation of blood granulocytes and monocytes and plasma proteins at the site of infection
- Neutrophils are the archetypal cell associated with acute inflammation
- Are attracted to sites of inflammation by:
- Complement activation
- Cytokine production
- Changes to vascular endothelium
- Neutrophil activation in an inflammatory lesion results in the release of prostaglandins
- Responsible for vasoactive changes and for pain
- Are attracted to sites of inflammation by:
- The accumulation of dead and dying neutrophils at the site of infection is called pus
- Their removal from the site after the removal of infection is an important step in the resolution of the lesion
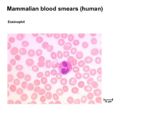
Eosinophils
- Eosinophils are less common than neutrophils, and they are not phagocytic
- Make up <5% of the leukocytes in normal blood
- Eosinophil numbers are increased:
- Slightly during the resolution phase of inflammation
- Many-fold in parasite-infected animals
- The presence of a large proportion of eosinophils in a blood smear is highly indicative of parasitaemia
- Mainly function by targeting the surface of parasites by means of specific antibody or complement
- Release a large range of toxic molecules that break down the parasite integument
- Prominent in allergic (anaphylactic) reactions
Basophils / Mast Cells
- Basophils/mast cells are principally localised at epithelial surfaces
- Very small numbers are present in blood
- Less than 0.5% circulating leukocytes
- Very small numbers are present in blood
- They have two principal functions:
- Induction of acute inflammation
- Trauma and/ or bacterial infection causes the production of cytokines by the mast cells that induce a classical acute inflammatory response
- Response to parasite infection
- Specific IgE binds cells
- Subsequent contact with antigen causes the mast cells to degranulate
- Release enzymes and vasoactive substances that can result in a high level of mucus secretion and smooth muscle contraction
- Induction of acute inflammation
- Also produce factors that influence local host cell physiology
- Various mediators increase the ratio of phagocyte to microbe