Difference between revisions of "Acute Inflammation - Introduction"
Rjfrancisrvc (talk | contribs) |
Rjfrancisrvc (talk | contribs) |
||
| Line 11: | Line 11: | ||
==Sequence of Events== | ==Sequence of Events== | ||
| − | + | The following sequence of events is provoked by the presence of the irritant. | |
# '''Momentary vasoconstriction''' | # '''Momentary vasoconstriction''' | ||
Revision as of 15:08, 9 May 2012
Introduction
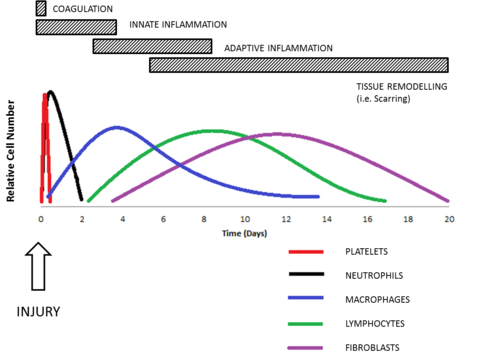
Acute inflammation is characterised by a sudden onset and may last for a few hours to a few days. Vascular, humoral and cellular alterations cause the 5 cardinal signs of inflammation as a result of exposure of tissues to various causes.
When acute inflammation becomes over-active it can be fatal. A classic example is septic shock caused by bacterial LPS. In most cases though acute inflammation acts to protect and repair the damage to the tissue by resolving by regeneration in association with the host defence mechanisms. To assist in resolving and controlling inflammation therapeutic measures have been developed, with some being very recognisable therapies, for example the Non-Steriodal Anti-Inflammatory Drugs (NSAIDs e.g. Aspirin and Ibuprofen N.B. NOT paracetomal).
A repair mechanism that can occur is fibrosis, otherwise known as scarring. There are also conditions, for example arthritis, where the acute inflammation can become chronic. First the inflammation goes through a subacute phase, though whether the inflammation becomes chronic is dependent upon the persistence of the agent and the amount of damage caused.
Sequence of Events
The following sequence of events is provoked by the presence of the irritant.
- Momentary vasoconstriction
- Following contact with the irritant, there is momentary vasoconstriction of the blood vessels in the affected area.
- This is reversed within minutes.
- Dilation of the blood vessels
- Initially, dilation of the capillaries is caused by the release of chemical mediators.
- Arterioles then dilate under the influence of a local axon reflex.
- This gives rise to an initial acceleration of the blood flow to the area.
- This later gives way to a slowing of blood flow, caused by alterations in vascular endothelial permeability and the filling of previously closed capillaries.
- Exudation of fluid
- Follwing the slowing of blood flow and altered capillary permeability, a protein-rich fluid is exudated.
- Margination of leukocytes
- Circulating white blood cells are attracted to the altered endothelial surfaces.
- Emigration of leukocytes
- Leukocytes migrate through the altered endothelium to reach the injured area.
- This is an active process - chemotaxis.
- The cells are attracted to the endothelium by release of proteins, and further into the tissues by factors released from cells in the damaged area.
- The emigrated leukocytes and components of the fluid exudate are also chemotactic.
- More cells and fluid are attracted to the area.
- Emigration of red blood cells
- Erythrocytes migrate through the gaps in the altered endothelium to the damaged tissue.
- Induction of an increase in temperature
- This may occur either locally or systemically.
- A systemic rise in temperature is known as pyrexia.
- Occurs in generalise acute inflammation.
- Pyrogens act on the temperature control centres in the hypothalamus, and are released from:
- Neutrophils, eosinophils and macrophages
- Particulary neutrophils when they begin to phagocytose.
- The cellular coat of gram-negative organisms.
- Necrosis of damaged tissue cells.
- Antigen-antibody complexes.
- Tumours.
- Particularly those which have metastasised
- It may be difficult to separate this from the pyrexia caused by the central necrosis in such tumours.
- Neutrophils, eosinophils and macrophages
Cells
- The classical cells of acute inflammation are neutrophils, eosinophils, macrophages, mast cells and basophils at an early stage of the inflammatory response, with the lymphocytes and fibroblasts forming the later stages.
- Macrophages are a common feature of acute and chronic inflammation.